Tse-Yu Chen1,2,3, Mei-Hui Chen2, Patrick C. Y. Woo2,4*
1Department of Neurosurgery, Neurological Institute, Taichung Veterans General Hospital, Taichung 402, Taiwan
2Doctoral Program in Translational Medicine and Department of Life Sciences, National Chung Hsing University, Taichung 402, Taiwan
3Rong Hsing Translational Medicine Research Center, National Chung Hsing University, Taichung 402, Taiwan
4The iEGG and Animal Biotechnology Research Center, National Chung Hsing University, Taichung 402, Taiwan
*Corresponding Author: Patrick C. Y. Woo, Doctoral Program in Translational Medicine and Department of Life Sciences, National Chung Hsing University, 145 Xingda Road, South District, Taichung 402, Taiwan.
Abstract
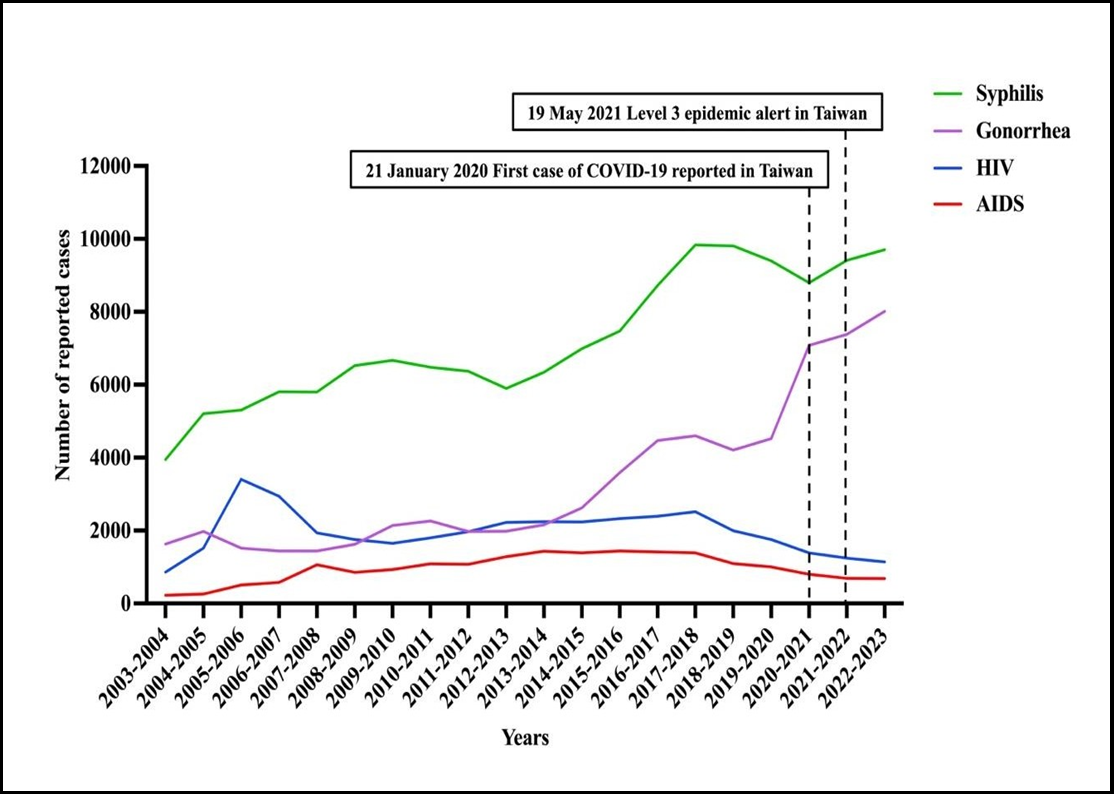
Infection control measures for COVID-19 have decreased the incidence of various infectious diseases, such as invasive pneumococcal disease and influenza. Two studies have shown that there may be an effect of COVID-19 on the incidence of sexually transmitted diseases (STDs) in Taiwan. In this article, we analyzed the incidence of four notifiable STDs in Taiwan over 20 years. The number of reported cases (2003-2022) for HIV infection, AIDS, gonorrhea, and syphilis were downloaded from a public database and analyzed. HIV cases rose from 2003 to 2005, decreased from 2005 to 2009, increased again from 2009 to 2017, and decreased after 2017. The AIDS cases rose quite steadily from 2003 to 2013, peaked and remained relatively stable from 2013 to 2017, and declined after 2017. The number of syphilis cases rose quite steadily from 2003 to 2022. The number of gonorrhea cases rose slowly from 2003 to 2013, with an acceleration in the rate of increase after 2013. There has been a differential change in the pattern of HIV infection, AIDS, syphilis, and gonorrhea in the last 20 years. The COVID-19 pandemic did not have any significant impact on the incidence of STDs in Taiwan.
Keywords: COVID-19; sexually transmitted diseases; Taiwan
Introduction
The COVID-19 pandemic has already resulted in an official loss of more than seven million human lives worldwide. Governmental policies and changes in personal practice have led to a slowdown of international and local travel, social distancing, and reduced interpersonal physical contact. It has been shown, in various studies, that these infection control measures for COVID-19 have also decreased the incidence of various infectious diseases, particularly respiratory tract infections, such as invasive pneumococcal disease and influenza [1,2,3,4]. Intriguingly, it has also been shown, in two independent studies, that the overall incidence of sexually transmitted diseases in Taiwan has increased, and such an increase was mainly attributed to a rise in the number of gonorrhea cases [5,6]. However, in both studies, the authors have only analyzed the number of patients with sexually transmitted diseases 1-2 years before and during the COVID-19 pandemic. In order to understand this intriguing phenomenon, we analyzed the incidence of four notifiable sexually transmitted diseases in Taiwan over 20 years. The reasons behind the change in incidence and the impact of COVID-19 on these four disease entities were speculated and discussed.
The number of reported cases for four clinical entities that were mainly transmitted through sexual contact, namely human immunodeficiency virus (HIV) infection, acquired immunodeficiency syndrome (AIDS), gonorrhea, and syphilis from 2003 to 2022, were downloaded from the National Notifiable Diseases Surveillance System, Center for Disease Control, Taiwan (https://www.cdc.gov.tw/). This is a publicly available open database developed before the SARS epidemic. Report of newly diagnosed notifiable diseases was mandatory and enforced by law. The downloaded incidence data were analyzed.
The number of reported cases of HIV infection rose rapidly from 2003 to its first peak in 2005, decreased from 2005 to 2009, increased again from 2009 to 2017, and decreased steadily from 2017 to 2022 (Figure 1). The number of reported cases of AIDS rose quite steadily from 2003 to 2013, peaked and remained relatively stable from 2013 to 2017, and decreased steadily from 2017 to 2022 (Figure 1). With some minor fluctuations, the number of reported cases of syphilis rose quite steadily from around 4,000 per year in 2003 to more than 9,000 per year in 2022 (Figure 1). With some ups and downs, the number of reported cases of gonorrhea rose slowly from 2003 to 2013 (Figure 1). From 2013 to 2022, there was an acceleration in the rate of increase in the number of cases of gonorrhea (Figure 1). Among these four clinical entities, the incidence of syphilis was the highest and that of AIDS was the lowest throughout the 20 years (Figure 1). From 2003 to 2013, the incidence of HIV infection and gonorrhea were similar, but from 2013 onwards, the incidence of gonorrhea has remained in the second position and that of HIV infection has remained in the third position throughout these 10 years (Figure 1).
Figure 1: Number of gonorrhea, syphilis, HIV and AIDS cases from 2003 to 2022 in Taiwan.
In this study, we showed that there has been a differential change in the pattern of HIV infection, AIDS, syphilis, and gonorrhea in the last 20 years in Taiwan. As a whole, the incidence of all four notifiable sexually transmitted diseases increased from 2003 to 2017. From 2017, the incidence of HIV infections and AIDS decreased gradually, while the incidence of syphilis remained relatively steady and that of gonorrhea has further increased (Figure 1). We speculate that such a phenomenon in the change in the incidence of the four sexually transmitted diseases for the last 20 years could be a result of a combination of several factors. First, more effective antiretroviral treatments, such as integrase inhibitors, have been used with fewer side effects. Such antiretroviral regimens have resulted in better compliance and control of HIV infection and AIDS, leading to a gradual reduction in the number of HIV infection and AIDS cases in the last few years moreover, the free distribution of needles in recent years has further reduced the transmission of HIV among intravenous drug users. However, such an improvement in treatment for HIV infection and AIDS is not present for syphilis and gonorrhea. Second, an increase in the circulation of levofloxacin-, ceftriaxone- and azithromycin-resistant strains of Neisseria gonorrhoeae might have been an obstacle to successful treatment, which might have accelerated the rate of increase in the incidence of gonorrhea in the recent 10 years [7,8]. Third, such a more rapid increase in the number of cases of gonorrhea since 2013 could also be due to the more widespread use of molecular tests for the laboratory diagnosis of gonorrhea in the last 10 years. Although molecular tests for gonorrhea have been accepted as a means of laboratory diagnosis for more than 15 years, their use has only become more and more popular in recent years.
Despite these changes in the disease patterns, the COVID-19 pandemic did not have any significant impact on the incidence of sexually transmitted diseases in Taiwan. As shown in Figure 1, it is demonstrated that there was no noticeable change in the trend of increase or decrease in the incidence of these four sexually transmitted diseases before and after the commencement of the COVID-19 pandemic. This is in contrast to other respiratory infections, such as invasive pneumococcal disease and influenza, where there was a dramatic fall in the incidence during the COVID- 19 pandemic [1,4]. In fact, since HIV infection and AIDS are chronic infections, the diagnosis of these conditions is usually made years after the patients acquire the virus through sexual contact or needle sharing. This is the reason why the start of antiretroviral therapy does not result in an immediate dramatic drop in the number of HIV infection and AIDS cases but only a gradual decrease in their incidence. Therefore, the incidence of new cases of HIV infection and AIDS during the COVID-19 pandemic reflected what had happened a few years ago. As for syphilis and gonorrhea, their incidence patterns before and after the commencement of the COVID-19 pandemic have reflected that there was not much change in the sexual behaviors of the population, irrespective of the governmental policies, travel restrictions, and changes in some other personal practice.
Conflict of Interest: The authors declare no conflict of interest.
Funding Statement: This work was partly supported by the framework of the Higher Education Sprout Project by the Ministry of Education (MOE-112-S-023-A) in Taiwan.
References
- Teng JLL, Fok KMN, Lin KPK, Chan E, Ma Y, et al. (2022) Substantial Decline in Invasive Pneumococcal Disease During Coronavirus Disease 2019 Pandemic in Hong Kong. Clin Infect Dis. 74(2): 335-338.
- Lim RH, Chow A, Ho HJ (2020) Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J Infect. 81(6): e19-e21.
- Juan HC, Chao CM, Lai CC, Tang HJ (2021) Decline in invasive pneumococcal disease during COVID-19 pandemic in Taiwan. J Infect. 82(2): 282-327.
- Heiskanen A, Galipeau Y, Little J, Mortimer L, Ramotar K, et al. (2023) Seasonal respiratory virus circulation was diminished during the COVID-19 pandemic. Influenza Other Respir Viruses. 17(1): e13065.
- Hung SH, Lin WT, Wang JH, Lai CC (2022) The impact of COVID-19 on the epidemiology of non-airborne/droplet-transmitted notifiable infectious diseases in Taiwan: A descriptive study. J Infect Public Health. 15(9): 1001-1005.
- Lai CC, Chen SY, Yen MY, Lee, Ko WC, et al. (2021) The impact of the coronavirus disease 2019 epidemic on notifiable infectious diseases in Taiwan: A database analysis. Travel Med Infect Dis. 40: 101997.
- Liu YH, Wang YH, Liao CH, Hsueh PR (2019) Emergence and Spread of Neisseria gonorrhoeae Strains with High-Level Resistance to Azithromycin in Taiwan from 2001 to 2018. Antimicrob Agents Chemother. 63(9).
- Lin HH, Li JW, Yang TY, Lee CY, Jain SH, et al. (2023) Emergence of a predominant sequence type ST7363 and the increasing trend of resistance to cefixime and ceftriaxone in Neisseria gonorrhoeae in Southern Taiwan, 2019-2021. J Microbiol Immunol Infect. 56(4): 833-841.