Aisha Alfituri*, Khaled Mangoush, Heba El-Zawawi
Assistant professor, University of Benghazi, Benghazi, Libya.
*Corresponding Author: Aisha Alfituri, Assistant professor, University of Benghazi, Benghazi, Libya.
Abstract
Paroxysmal visual manifestations may represent epileptic seizures arising from the occipital lobe. We report the case of a female adult patient from a Libyan outpatient clinic with bilateral recurrent attacks of reversible visual disturbances, and a positive family history of tonic-clonic seizures. She had unremarkable ophthalmological and neurological examination findings but had EEG abnormalities in both occipital lobes. The study seeks to emphasise the fact that occipital lobe epilepsy although rare, should be considered when patients present only with visual symptoms, along with registering occipital epileptic activity between seizures. Differential diagnoses were considered, including migraine.
Keywords: Visual Hallucination, Occipital epilepsy, Electroencephalography.
Introduction
Background
Focal seizures with visual hallucinations were previously classified as simple partial seizures. [1] A recent classification classifies them as focal sensory seizures with elementary symptoms, [2] or visual auras. [3]
They originate in the temporal–occipital cortices. Their incidence is not well known, but they are generally considered rare. They have been reported to constitute 8 % of total seizures in the predominant population with epilepsy. [4]
They are seizures with subjective visual phenomena, which are either positive (seeing images) or negative (not seeing in part or all of the visual field). Visual hallucinations can be coloured or colourless. [5] Simple visual hallucinations comprise dots or simple shapes. [6] Complex epileptic visual phenomena include visual illusions (mistaking one object for another) and hallucinations (seeing objects or scenes that are not there). Visual hallucinations are often unilateral and seizures with visual hallucinations are often associated with other eye-related signs such as blinking or ictal nystagmus.
Epileptic visual hallucinations may be quite prolonged, and in reporting a visual hallucination, there cannot be any loss of consciousness.
Visual hallucinations can occur in isolation or evolve into more objective seizures. These vary depending on the route of seizure propagation. Visual seizures can evolve into seizures with altered awareness, manual and oro-alimentary automatisms if they propagate into the temporal region. They can also evolve into tonic seizure activity with propagation into the frontal regions and may also present with hyperactive automatisms. Secondary generalization and status epilepticus are common. [7]
Seizures with visual hallucinations can be caused by structural lesions, in which permanent visual field deficits often present, or can be idiopathic such as benign late-onset childhood occipital epilepsy (Gastaut type).
Gastaut type epilepsy is characterized by seizures with visual hallucinations and typical occipital paroxysms on the EEG. [8] Consciousness is usually preserved, and seizures are followed by headache, nausea, and vomiting. [9] The onset of seizures is between 7 and 9 years, and seizures usually respond well to antiepileptic medication.
A family history of febrile seizures or epilepsy is common (seen in up to one-third of cases) and a family history of migraine is also reported (9-16 % of cases).
Benign early-onset childhood occipital lobe epilepsy (Panayiotopoulos type) has similar EEG findings with occipital paroxysms, but seizures are more dominated by autonomic symptoms such as vomiting. [10]
Interictal EEG recordings show paroxysms of posterior temporal– occipital spikes and sharp wave complexes. Rhythmic spiking or activity over the occipital regions during ictal events is typical. Prolonged visual hallucinations can have a pattern of "Periodic Lateralized Epileptiform Discharges" (PLEDS). Seizures with visual hallucinations that evolve into clinical seizures with altered awareness may show only a pattern of posterior temporal rhythmic activity, or nonspecific EEG changes, at the time of seizure onset. Intracranial EEG confirms occipital seizure onset and spread during visual hallucinations. EEG in benign childhood occipital epilepsy is characterized by diphasic spike-wave discharges over the occipital region in the interictal state. Spikes are activated in non-REM sleep and disappear with eye-opening. Ictal EEG shows rhythmic theta and delta activity in the posterior quadrant.
Structural imaging by means of Magnetic Resonance Imaging (MRI), High-Resolution Electrophysiological Non-Invasive Source Imaging, Positron Emission Tomography or Single Photon Emission Tomography can provide important information in difficult cases. [11]
Seizures with visual hallucinations, especially benign childhood occipital epilepsies, respond to treatment with antiepileptic medications. [12]
Case presentation
A 36-year-old Libyan woman presented with a history of frequent attacks of transient illusory visual symptoms in both eyes. The attacks started when the patient was 11 years old and recurred every year until the age of 14 years when the attacks disappeared completely. At the age of 29 years, the transient illusory visual symptoms recurred, when the patient was in the post-partum period after a Caesarean section for the birth of her fourth child; and from that time onwards the attacks became more frequent and had a longer duration. The most recent attack remained for one hour. Every attack was preceded by seeing flashes of light, except the last one, which happened without aura. Each attack was followed by a severe occipital headache, which was not relieved with analgesic medications. The patient described the attack as seeing the central part of an object with an inability to see the surrounding area. This was followed by seeing more parts of the object and ended by seeing only the peripheral part, with the inability to see its central part. There was no history of loss of consciousness. The patient had an unremarkable medical and surgical history. She had a family history of tonic-clonic epilepsy in her younger brother and her aunt. Ophthalmological and neurological examination results were normal. Extracranial EEG recording was performed (Figure 1, 2, 3, 4 and 5). MRI of the head was normal.
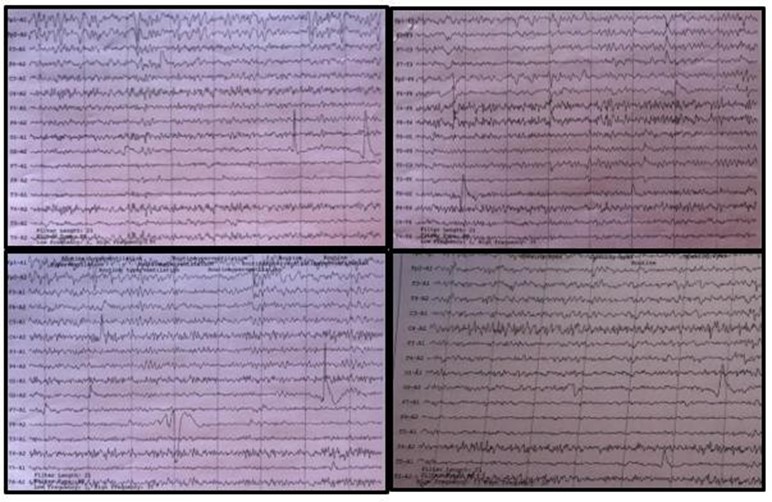
Figure 1. The interictal EEG showing episodic spike and wave discharges from the right occipital lobe.
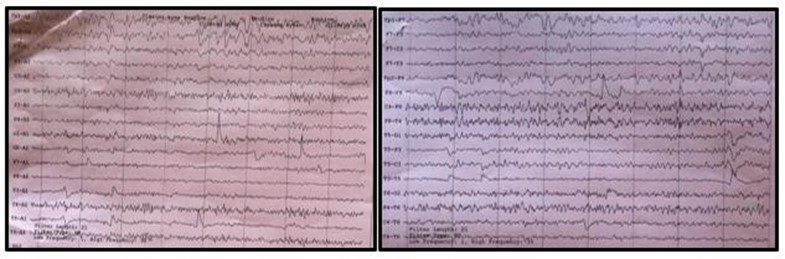
Figure 2. The interictal EEG showing episodic spike and wave discharges from the left occipital lobe.
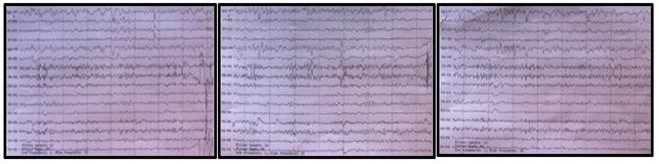
Figure 3. EEG recording of the patient showing multifocal spread of the epileptiform activity.
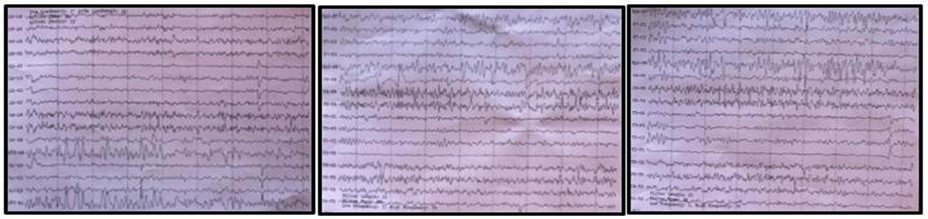
Figure 4. ECG recording of the patient showing similar multifocal spread of the epileptiform activity.
Figure 5. EEG recording of the patient showing further multifocal spread of the epileptiform activity.
Discussion and conclusions
We report the case of a patient with occipital epilepsy who presented with recurrent attacks of visual impairment as a main presenting symptom followed by severe occipital headache.
Visual manifestations and headaches can be caused by migraine. Epileptic visual hallucinations can be difficult to distinguish from the visual aura of migraine. [13] It has been reported that the frequency of epilepsy in patients with migraine is about 17 % higher than the frequency of epilepsy in the general population. [14] Furthermore, the prevalence of migraine is 23% higher among patients with epilepsy compared to normal individuals. Similar percentages (16.3 % of patients with headache had epilepsy, and Migraine was associated with epilepsy in 27.7 %) were reported in a local study from Benghazi, Libya. [15] The association between these two neurological conditions can be classified into preictal, ictal, postictal, and interictal headaches. [16] Preictal headaches occur in 5-15 % of cases, ictal in 3-5 %, postictal (a headache occurring within 3 hours after the cessation of a seizure) in 10-50 % of cases, and interictal in 25-60 %. [17] Our patient had a postictal headache, which is the most frequent headache associated with seizures. [23] Parisi et al., have suggested four criteria for a diagnosis of an epileptic headache to be made. These include duration of headache from seconds to hours, epileptic form discharges during the electroencephalogram with ipsilateral or contralateral focus with respect to the headache's location, epileptiform discharges on scalp EEG during a headache attack, and termination of the headache after intravenous administration of anticonvulsant therapy. [18,19,20]
We had strong electro-clinical evidence that our patient was suffering from seizures with the predominant presenting symptom being visual symptoms and postictal headache. The EEG recording findings of our patient conformed to the described findings in such cases. Positive family history is another supporting issue for diagnosing epilepsy.
Furthermore, visual hallucinations occur in psychiatric disorders and dementia; however, those hallucinations are less stereotyped than epileptic visual hallucinations and do not have EEG changes.
Moreover, occipital lobe epilepsy may masquerade as temporal lobe epilepsy. Posterior temporal seizures may also present with visual hallucinations. [27] In a study of focal onset seizures that included patients with temporal lobe epilepsy, postictal disturbances such as slow waves were found in 69 to 81 % of seizures, with no changes found in the remainder of the EEG. [21] Visual symptoms and occipital findings in the EEG suggest the diagnosis of occipital lobe epilepsy, but an absence of these features does not exclude the diagnosis. When posterior temporal EEG findings or multi-lobar involvement occurs, the diagnosis of occipital lobe epilepsy should be considered. [22] We believe that our patient may fit in this latter group of patients.
In conclusion: acute visual impairment can present as the main symptom of occipital lobe epilepsy when occipital lobes are involved, and its possible mechanism may be visual neglect.
Conflict of Interest: None
Ethical considerations: Approval for use of case clinical data and investigation results were obtained.
References
- Anonymous (1981) Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Commission on classification and terminology of the international league against epilepsy. Epilepsia. 22(4): 489 501.
- Engel J Jr. (2006) Report of the ILAE classification core group. Epilepsy. 47(9): 1558 1568.
- Luders H, Acharya J, Baumgartner C, Benbadis S, Bleasel A, et al. (1998) Semiological seizure classification. Epilepsia. 39(9): 1006 1013.
- Sveinbjörnsdòttir S, Duncan JS (1993) Parietal and occipital epilepsy. Epilepsia. 34(3): 493-521.
- Williamson PD, Thadani VM, Darcey TM, Spencer DD, Spencer SS, et al. (1992) Occipital lobe epilepsy: clinical characteristics, seizure spread patterns and results of surgery. Ann Neurol. 31(1): 3-13.
- Jobst BC (2010) Focal Seizures with Visual Hallucinations. In: Panayiotopoulos C.P. (eds) Atlas of Epilepsies. Springer, London.
- Jobst BC, Roberts DW, Williamson PD. Occipital nonconvulsive status epilepticus. In: Kaplan PW, Drislane F (eds) Nonconvulsive status epilepticus. Demos Medical Publishing, New York, 2008. pp 131 142.
- Gastaut H (1982) A new type of epilepsy: benign partial epilepsy of childhood with occipital spike waves. Clin Electroencephalogram. 13(1): 13-22.
- Jobst BC (2010) Focal Seizures with Visual Hallucinations. In: Panayiotopoulos C.P. (eds) Atlas of Epilepsies. Springer, London.
- Ferrie C, Caraballo R, Covanis A, Demirbilek V, Dervent A, et al. (2006) Panayiotopoulos syndrome: a consensus view. Dev Med Child Neurol. 48(3): 236 240.
- Panayiotopoulos CP (1999) Visual phenomena and headache in occipital epilepsy: a review, a systematic study and differentiation from migraine. Epileptic Disord. 1(4): 205 216.
- Çilliler AE, Güven H, Çomoğlu SS (2017) Epilepsy and headaches: Further evidence of a link. Epilepsy Behav. 70(Pt A): 161-165.
- El-Zawawi H (2019) Reflection of the burden of Headache and Facial pain on the community and underlying pathologies: A prospective study from Benghazi Libya. Journal of the Neurological Sciences. 405S: 116542
- Kingston WS, Schwedt TJ (2017) The Relationship between Headaches with Epileptic and Non-epileptic Seizures: A Narrative Review. Curr Pain Headache Rep. 21(3): 17.
- Bianchin MM, Londero RG, Lima JE, Bigal ME (2010) Migraine and epilepsy: a focus on overlapping clinical, pathophysiological, molecular, and therapeutic aspects. Curr Pain Headache Rep. 14(4): 276-283.
- Fanella M, Morano A, Fattouch J, Albini M, Manfredi M, et al. (2015) Ictal epileptic headache in adult life: Electroclinical patterns and spectrum of related syndromes. Epilepsy Behav. 53: 161-165.
- Parisi P, Striano P, Kasteleijn-Nolst Trenite DGA, Verrotti A, Martelletti P, et al (2012) Ictal Epileptic Headache: recent concepts for new classifications criteria. Cephalalgia. 32(9): 723- 724.
- Parisi P, Striano P, Verrotti A, Villa MP, Belcastro V (2013) What have we learned about ictal epileptic headache? A review of well- documented cases. Seizure. 22(4): 253-258.
- Parisi P, Kasteleijn-Nolst Trenite DGA, Piccioli M, Pelliccia A, Luchetti A, et al. (2007) A case with atypical childhood occipital epilepsy “Gastaut type”: An ictal migraine manifestation with a good response to intravenous diazepam. Epilepsia. 48(11): 2181- 2186.
- Bien CG, Benninger FO, Urbach H, Schramm J, Kurthen M, et al. (2000) Localizing value of epileptic visual auras. Brain. 123(Pt 2): 244 253.
- Kaibara M, Blume WT (1988) The postictal electroencephalogram. Electroencephalogram Clin Neurophysiol. 70(2): 99-104.
- Appel S, Sharan AD, Tracy JI, Evans J, Sperling MR (2015) A comparison of occipital and temporal lobe epilepsies. Acta Neurol Scand. 132(4): 284-90.



