Pacheco JA1*, Tholt B2, Molena KF3, Gontijo CRO4, Veiga EV5
1Research Coordinator at the Ribeirão Preto Cancer Hospital, Ribeirão Preto, Brazil. (0000-0002-5964-1887)
2Assistant Professor, Veiga of Almeida University, Rio de Janeiro, Brazil. (0000-0001-7783-3586)
3Doctoral student in the Postgraduate Program in Pediatric dentistry at the School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil. (0000-0002-7290-8451)
4Doctoral student in the Postgraduate Program in Pediatric dentistry at the School of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil. (0000-0001-7006-469X)
5Full Professor at Ribeirão Preto School of Nursing, University of São Paulo, Ribeirão Preto, Brazil. (0000-0003-3677-0210)
*Corresponding Author: Pacheco JA, Research Coordinator at the Ribeirão Preto Cancer Hospital, Ribeirão Preto, Brazil. (0000-0002-5964- 1887)
Abstract
In this case study, we present a description of the treatment approach of an oral manifestation caused by Sars-Cov-2, in an oncological patient, which manifested itself in the post-extubation period. This patient was referred to the DDCH-RP (Department of Dentistry, Hospital do Câncer de Ribeirão Preto), Brazil, because the oral lesion was resistant, in addition to changes in vital signs. The association between Antimicrobial Photodynamic Therapy (aPDT) and Systemic Photobiomodulation (PBMS) in the primitive carotid artery (PCA) was used as a treatment to reduce oral damage and stabilize vital signs (blood pressure, heart rate and O2 saturation), monitored by individualized responses, in the context of precision medicine.
Keywords: Photodynamic therapy; Systemic Photo biomodulation; Oral manifestation; SARS-CoV-2; Vital signs
1. Introduction
Cancer patients who are infected by coronavirus disease tend to show worse clinical and laboratory results when compared to non-cancer patients [1]. In this critical period of global health, several national and international studies are being published to assess the clinical characteristics of the contamination caused by Sars-Cov-2 in a timely manner. Moreover, with regard to cancer patients infected by the coronavirus, greater controlled attention is needed, as cancer therapy causes a transient or lasting immunosuppressed immunological changed by drugs. This factor, associated with the high age group among this public that is commonly affected, predisposes these patients with Sars-Cov-2 infection to progress to undesirable secondary opportunistic infections [2,3].
In the recent period, scientific evidence has supported the idea that the angiotensin-2 converting enzyme (ACE2) is considered the main host cell receptor of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), whose expression in the oral cavity is considerable, mainly in the epithelial cells of the tongue and salivary glands [4].
When the patient is positive for Covid-19, the immunosuppression process produces unreasonable refractory systemic effects that cause undesirable manifestations in the oral cavity, increasing the degree of virulence of the infection. Evidence of this type of viral replication in the oral mucosa is shown by extremely painful oral lesions that are resistant to conventional drugs. Studies have suggested that Sars-Cov- 2 can infect and replicate in keratinocytes and oral fibroblasts, causing oral alterations and superficial necrosis, with an eventual atypical development in the glossopharyngeal region, lips, palate, and oropharynx [5]. The common symptoms that typify Covid-19 are fever, dry cough, and fatigue, but the loss of smell or taste are symptoms reported in over 60 % of patients [6,7].
Due to the context of innovative therapeutic treatments in recent years, Low-Intensity Laser Therapy (LLLT) has emerged as an effective therapeutic tool in stomatology due to its ability to enhance wound healing, tissue repair and prevent necrosis in biological tissues, promoting the reduction of inflammation in chronic diseases, promoting analgesia, and decreasing oedema [8] (Figure 1).
Figure 1: Schematic representation of the main application areas of low-level laser therapy.
The application of LLLT on the biological tissues and haematological system of the human body produces an effect called photo biomodulation, which causes photons to be absorbed by electronic absorption bands belonging to some molecular chromophore/photoreceptor (8).
Another important consideration involves tissue properties. Both the absorption and diffusion of light in tissue are wavelength-dependent, and tissue chromophores have high absorption bands at wavelengths between 600 and 840 nm. Some researchers call this phenomenon the existence of a so-called "optical window" (Figure 2), as it involves the optical and absorptive properties of tissue cells [9].
Figure 2: Optical window in tissue due to reduced absorption of red and laser wavelengths (600-1200 nm) by tissue chromophores.
The use of LLLT on biological tissue associated with a photosensitive substance (methylene blue) is called Antimicrobial Photodynamic Therapy (aPDT). aPDT is a treatment that has previously been used in several health specialties, such as physiotherapy, dermatology, oncology, speech therapy, ophthalmology, and dentistry. It consists of administering a photosensitizing dye (PS), followed by irradiating the lesion with visible light, forming reactive species in the presence of oxygen, such as singlet oxygen and free radicals [10]. These chemical reactive species are cytotoxic and can cause the destruction of proteins, lipids, nucleic acids, and other cellular components, resulting in the destruction of microbial colonization [11].
The use of methylene blue in photodynamic therapy has shown effective results in inactivating colonization by microbes (viruses, fungi, and bacteria), but it is necessary to establish an adequate clinical protocol regarding pre-irradiation time and dye concentration, without toxic effects to the body cells.
The effects of aPDT are based on three components: light, a photoactive agent (photosensitizer), and the presence of oxygen [12]. The PS most used in clinical dental practice is of the phenothiazine class, called methylene blue (MB) [13]. Recently, almost all existing studies on aPDT have focused on pathogenic bacteria to reduce the level of inflammation in different regions of the oral cavity [12,13]. As regards the Systemic Photo biomodulation technique (PBMS), this is applied with the Low-Intensity Laser device, used indirectly, on the vascular anatomical region (vein or artery), directed by the active tip of the device. It is a non-invasive application without tissue damage, performed according to protocols pre-guided by the global literature and by the instructions of the manufacturer of each device [14].
Regarding the vagal structures, the primitive carotid artery (PCA) has a desirable caliber, is easily accessible and that allows for good vascularization of anterior facial areas, which contributes to a good prognosis [14,15].
Furthermore, with regard to vital signs in patients infected with Sars- Cov-2, there is evidence that median systolic blood pressure is higher in deceased patients (137.0 mm Hg) than in recovered patients (125.0 mm Hg). Indeed, more patients who died than those who recovered had blood pressures of 140 mm Hg or higher. Furthermore, heart rates were much higher in deceased patients (101.0 beats per minute) than in recovered patients (91.0 beats per minute). Respiratory rates were significantly higher in deceased patients (24.0 breaths per minute) than in recovered patients (20.0 breaths per minute). In 72 (64 %) of deceased patients, only 19 (12 %) who recovered had a percutaneous oxygen saturation of 93 % or less on admission [16].
PBMS is known to produce the benefits of a photobiological response within cells that have undergone micro and macrovascular changes, by triggering anti-ischemic activity, positively reacting to the rheological properties of blood, increasing permeability of the vascular wall, stimulating tubule development in capillaries, eliminating vasospasm and stasis, reversing blood flow, decreasing capillary edema, and increasing the number of functional capillary tubes [17,18]. Furthermore, PBMS induces the release of nitric oxide (NO), considered one of the main relaxation factors of endothelial cells with a potential vasodilator effect, which influences lower BP values, as well as a reduction in HR [19,20].
To date, there are no scientific publications or research on the use of aPDT and PBMS in oral manifestations and control of vital signs in infection caused by Sars-Cov-2 in cancer patients.
2. Case Report
Patient ESS, a 57-year-old man, in remission of oesophageal cancer, presented to the DDCH-RP (Department of Dentistry of the Ribeirão Preto Cancer Hospital), Brazil, with lesions in the oral cavity because of infection caused by Sars-Cov-2 (Figure 3). This diagnosis was confirmed by the positive rtPC-R for Covid-19 and the fact that 15 days previously, he was discharged from the intensive care unit of the public hospital in Brazil, where he had needed to be submitted to oropharyngeal intubation for 12 days.
Figure 3: Initial status of the tongue affected by lesions.
During extubation, the nursing team detected alterations in the intraoral region. These were located on the tongue and had clinical characteristics similar to those of a fungal lesion (symptoms of burning, pain, oedema, and hyperkeratosis that reduced the capacity for enteral nutrition).
During the assessment of the oral cavity in the DDCH-RP, a relative reduction in salivary flow was observed, in addition to painful glossopharyngeal [neuralgia] on the dorsum and lateral border of the tongue, erythemas that characterized burning throughout the oral cavity, pain in the sublingual region and difficulty in chewing food. The clinical characteristics of the lingual region suggested that it was Pseudomembranous candidiasis. a more common manifestation in immunosuppressed individuals using corticosteroids and/or broad-spectrum antibiotics or with systemic disorders such as decompensated diabetes, leukemia, and/or HIV infection [21]. The oral lesion was resistant to antibiotic drugs and did not disappear.
3. Methods
3.1 Complementary vital signs measurements
The patient's vital signs were initially measured, and the following values were recorded: Blood Pressure 120 x 80 mm / Hg, Heart rate 88 bpm, SpO2 89 % (O2 saturation). BP values were considered altered when, at the time of measurement, they were higher than or equal to 140x90 mm Hg [22]. The heart rate value was considered altered, as it was outside the range of 60-100 beats per minute [23]; and oxygen saturation (SpO2) was below normal (measurement range: 70 to 99 %). The purpose of this work was to obtain successful management by associating the aPDT and PBMS techniques for the treatment of cancer patients infected by Sars-Cov-2, to achieve repair of the oral manifestations and stabilization of vital signs.
3.2 Irradiation parameters
The low-level laser irradiation parameters are measured in wavelengths (nm), energy (joules), and fluency (J/cm2) [24,25]. The laser therapist dentist defined the application protocol based on the energy density of the device, however, the variety of types of laser equipment available on the market can change the proposed therapeutic responses, due to changes in parameters that vary according to the different manufacturers (Table 1).
Table 1: Irradiation parameters.
|
Irradiation Parameters |
Unit of measurement |
Description |
|
Wavelength |
nm |
It is the laser emission characteristic defined by different colours of the visible (400 to 700 nm) and invisible spectrum |
|
Fluence |
J/cm2 |
Fluency or dose is a description of the energy flow divided by the area of the laser emitter tip |
|
Energy |
Joule |
Energy is represented by the power of the equipment multiplied by the treatment time |
3.3 CRPP service protocol
Initially, asepsis of the entire oral cavity with 0.12 % Chlorhexidine gluconate mouthwash was applied on sterile gauze that was used to manually rub the area before each appointment. Moreover, a protective plastic was used on the active tip of the laser device.
3.4 aPDT (Therapy Photodynamic antimicrobial)
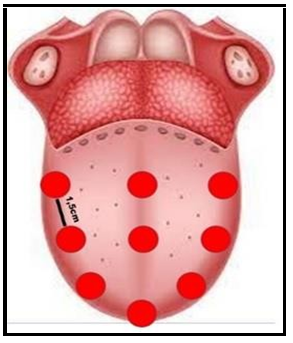
The methylene blue gel (0.01 %) was used to completely cover the tongue and stain the entire injured oral region. All excess gel was aspirated, and after waiting 5 minutes (pre-irradiation time) the patient was submitted to laser application with the red wavelength, using the following parameters: (Red laser - 660 nm; the power of 100 mW - Energy of 6 Joules per point). The lingual region received 9 points of laser application, with a distance of 1.5 cm between them (Figures 4- 7). The aPDT treatment proposed, consisted of 3 sessions, on alternate days, in the entire lingual region until the total repair of the injured tissue was obtained (Figure 8)
Figure 4: Application of methylene blue on the tongue.
Figure 5: Application of aPDT over the tongue.
Figure 6: Tissue repair in the lingual region.
Figure 7: Points of application of aPDT on tongue.
Figure 8: Evolution of the oropharyngeal condition using aPDT for the five consultations carried out at the Cancer Hospital of Ribeirão Preto.
3.5 PBMS transdermal in PCA (Primitive Carotid Artery)
The PBMS treatment was performed in the PCA with the aid of a collar adapted to the Laser Therapy device, in which the uninterrupted application of red wavelength (660 nm) was performed for 15 minutes. The total PBMS energy was 90 Joules. The primitive carotid artery extends from the level of the upper border of the lamina of the thyroid cartilage to a point behind the neck of the mandible, between the tip of the mastoid process and the angle of the mandible, that is, the region of the anterior edge of the sternocleidomastoid muscle (SCM) (Figure 9 and 10).
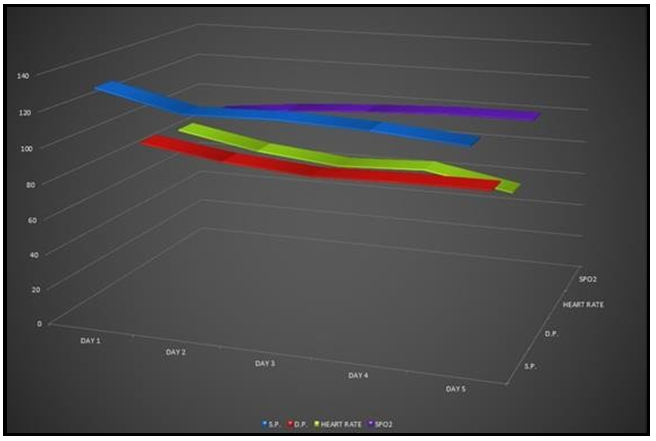
The PBMS treatment in PCA (right) proposed consisted of 3 sessions, on alternate days, in addition to using a manual device to monitor blood pressure (BP), heart rate (HR), and oxygen saturation (SPO2) markers (Figure 11).
Figure 9: Anatomical location of the primitive carotid artery.
Figure 10: Low-level laser applied over primitive carotid artery adapted to the cervical collar.
Figure 11: Data collection related to blood pressure (systolic and diastolic pressure), heart rate and oxygen saturation during the five consultations held at the Cancer Hospital of Ribeirão Preto.
4. Discussion
In this case study, rapid repair of the lingual lesion was observed, and the patient was satisfied with the result achieved, as the procedure was painless and non-invasive. In this case, aPDT was shown to be an effective, quick option, without side effects, and with high adherence to treatment by the patient [26]. The results were observed on the second day, after the first irradiation with aPDT, when the healing process and tissue repair occurred, of lesions caused by Covid-19 in the oral cavity [27]. Other associated oropharyngeal alterations, such as odynophagia, were re-established, according to the FOIS scale, from level 2 (dependent on the alternative route and minimal oral route of any food or liquid) to level 7, at which the enteral diet was stabilized [28]. The VAS scale represented the punctual decrease in analgesia and burning sensation [25].
In the assessment of vital signs, the values related to blood pressure were normalized, and especially, the heart rate decreased which would be a post-Covid prevention factor, because according to experts from the University of Texas Health Sciences Centre, in Houston (UTHealth), these patients would be at increased risks for later cardiovascular disease and possible heart damage, even if they do not have underlying heart problems. Relative to SpO2, the evolution was responsive with an increase from 89 % to 99 %.
Studies have suggested that the wavelength of light was absorbed by haemoglobin, and this illumination released nitric oxide (NO) from haemoglobin (specifically from the nitrosothiols in the beta chain of the haemoglobin molecule) into red blood cells. Dissociation of NO from Cox increased the respiration rate and protected cells against NO-induced cell death [29-32].
PBMS promotes important haematological and hemodynamic repercussions, such as stimulating the immune response; increasing IgG, IgM, and IgA immunoglobulins; stimulating interferons, interleukins, and TNF-alpha; stimulating lymphocyte proliferation; increasing phagocytic activity of macrophages; improving the antioxidant enzymatic system with antitoxic effect; improving erythrocyte regeneration and microcirculation; reducing thrombocyte aggregation; activating fibrinolysis; stimulating NO production in monocytes with vasodilation and improved endothelium; increasing production of ATP in the respiratory chain and normalizing cell membrane potential [33], which directly and indirectly have beneficial refractory effects on various physiological systems of the human body.
A relevant addition to the study was that this patient was in oncological remission and the results presented were satisfactory, with the acceleration of the lesion repair process, with no pain or discomfort during all consultations.
It must, however, be emphasized that contemporary dentistry is becoming more and more personalized, especially when associated and innovative health protocols are instituted.
5. Conclusion
Given the current pandemic context, for the prognosis, individualized management of each hospital patient is essential in order to impact the survival of these patients, who may present with transient or long- lasting systemic dysfunctions.
In other words, contemporary treatments need to be contextualized to a nostalgic but very current thought of the great Greek philosopher Aristotle, where equals must be treated equally and unequal’s unequally, to the extent of their inequality.
The aPDT associated with the use of systemic photo biomodulation (PBMS) in the primitive carotid artery (PCA) proved to be effective for the treatment of manifestations in the oral cavity promoted by the coronavirus and normalization of vital signs, respectively.
6. Ethics approval and consent to participate
Due to its retrospective nature, the study was exempted from the requirement to undergo review by the Research Ethics Committee of the Ethics Committee of the Ribeirão Preto Cancer Hospital, Brazil.
7. Conflict of interests: The authors have no conflict of interest to declare.
8. References
- Henry J, Henrik F (2021) Balance on the slack line; diagnostic intensity and patient safety during the SARS-CoV-2 pandemic. Acta Oncol. 60(1): 1-3.
- Qiu W, Yi F, Ren X, Li Z, Wang D, et al. (2020) Case Report: a nasopharyngeal cancer patient got covid-19 during radiochemotherapy in Wuhan. Front Oncol. 10: 1755.
- Yu J, Ouyang W, Chua MLK, Xie C (2020) SARS-CoV-2 transmission in cancer patients at a tertiary hospital in Wuhan, China. JAMA Oncol. 6(7): 1108–1110.
- Huang N, Pérez P, Kato T, Yu M, Kenichi O, et al. (2021) SARS- CoV-2 infection of the oral cavity and saliva. Nat Med. 27(5): 892–903.
- Brandão TB, Gueiros LA, Melo TS, Prado-Ribeiro AC, Nesrallah ACFA, et al. (2021) Oral lesions in patients with SARS-CoV-2 infection: could the oral cavity be a target organ? Oral Surg Oral Med Oral Pathol Oral Radiol. 131(2): e45-e51.
- Menni C, Sudre CH, Steves CJ, Ourselin S, Spector TD (2020) Quantifying additional COVID-19 symptoms will save lives. The Lancet. 395: e107-8.
- Horn A, Krist L, Lieb W, Montellano FA, Kohls M, et al. (2021) Long-term health sequelae and quality of life at least 6 months after infection with SARS-CoV-2: design and rationale of the COVIDOM-study as part of the NAPKON population-based cohort platform (POP). Infection. 49(6): 1277-1287.
- Madi M, Mahmoud MM (2020) The evaluation of the healing effect of low-level laser treatment after gingivectomy. Beni-Suef Univ J Basic Appl Sci. 9: 25.
- Rohringer S, Holnthoner W, Chaudary S, Slezak P, Priglinger E, et al. (2017) The impact of wavelengths of LED light-therapy on endothelial cells. Sci Rep. 7(1): 10700.
- Chen Q, Dan H, Tang F, Wang J, Li X, et al. (2019) Photodynamic therapy guidelines for the management of oral leukoplakia. Int J Oral Sci. 11(2): 14.
- Kwiatkowski S, Knap B, Przystupski D, Saczko J, Kędzierska E, et al. (2018) Photodynamic therapy – mechanisms, photosensitizers and combinations. Biomed Pharmacother. 106: 1098-1107.
- Machado AEH (2000) Photodynamic therapy: principles, application potential and perspectives. Química Nova. 23(2): 237- 243.
- Kim SH, Park SH, Chang BS, Lee SY, Lee JK, et al. (2017) Antimicrobial effect of photodynamic therapy using methylene blue and red color diode laser on biofilm attached to sandblasted and acid-etched surface of titanium. Laser Dent Sci. 1: (2-4).
- Pacheco JA, Schapochnick A, de Sá CC, Santiago ACM, Martinez GL, et al. (2019) Applied transdermal photobiomodulator therapy about the primary carotide artery in patients under hormone blockers and dynude disorders and pathogenic flora of orofaringeo and systemic repercussions. Am J Biomed Sci & Res. 4(4).
- Banks ND, Hui-Chou HG, Tripathi S, Collins BJ, Stanwix MG, et al. (2009) An anatomical study of external carotid artery vascular territories in face and midface flaps for transplantation. Plast Reconstr Surg. 123(6): 1677-1687.
- Chen T, Wu DI, Chen H, Yan W, Yang D, et al. (2020) Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 368: m1295.
- Mikhaylov VA (2015) The use of Intravenous Laser Blood Irradiation (ILBI) at 630–640 nm to prevent vascular diseases and increase life expectancy. Laser Ther. 24(1): 15–26.
- Ionin AP. Influence of low-energy irradiation of helium-neon laser on clinical and functional parameters of cardiovascular system in patients with various forms of a stenocardia. PhD thesis. Ekaterinburg, 1999.
- Lizarelli RFZ, Grecco C, Regalo SCH, Esteban Florez FL, Bagnato VS (2021) A pilot study on the effects of transcutaneous and transmucosal laser irradiation on blood pressure, glucose and cholesterol in women. Heliyon. 24;7(5): e07110.
- Oishi JC, De Moraes TF, Buzinari TC, Cárnio EC, Parizotto NA, et al. (2017) Acute hypotensive effect of photobiomodulation therapy in hypertensive rats. Life Sciences. 178: 56-60.
- Garcia-Cuesta C, Sarrion-Pérez MG, Bagán JV (2014) Current treatment of oral candidiasis: a literature review. J Clin Exp Dent. 6(5): e576-82.
- Candido SSV. Blood pressure tracking in the municipality of Franca: a proposal in line with the World Hypertension League. Dissertation, University of São Paulo, 2018.
- Andrade ED, Ranali J. Medical emergencies in dentistry. 3rd ed. São Paulo: Artmed; 2011.
- Silva LAD, Pinheiro SL (2021) Clinical Evaluation of Intravascular Blood Irradiation with Laser, Photobiomodulation, and Photodynamic Therapy in Cancer Patients with Mucositis. Photobiomodul Photomed Laser Surg. 39(11): 687-695.
- de Cunha LA, Firoozmand LM, da Silva AP, Camargo SEA, Oliveira W (2008) Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J. 58(4): 213- 7.
- Roomaney IA, Holmes HK, Engel MM (2021) Treatment of oral fungal infections using photodynamic therapy: Systematic review and meta-analysis. Clin Exp Dent Res. 7(3): 354-364.
- Ramires MCCH, Mattia MB, Tateno RY, Palma LF, Campos L (2021) A combination of phototherapy modalities for extensive labral lesions in a patient with SARS-CoV-2 infection. Photodiagnosis Photodyn Ther. 33: 102196.
- Mansouri V, Arjmand B, Rezaei TM, Razzaghi M, Rostami-Nejad M, et al. (2020) Evaluation of the effectiveness of low-level laser therapy. J Lasers Med Sci. 11(4): 369-380.
- Dovigo LN, Pavarina AC, Ribeiro DG, Adriano CS, Bagnato VS (2010) Photodynamic inactivation of four Candida species induced by photogem®. Brazil J Microbiol. 41(1): 42-49.
- Alrabiah M, Alsahhaf A, Alofi RS, Al-Aali KA, Abduljabbar T, et al. (2019) Efficacy of photodynamic therapy versus local nystatin in the treatment of dental stomatitis: a randomized clinical trial. Photodiagnosis Photodyn Ther. 28: 98-101.
- Mima EG, Vergani CE, Machado AL, Massucato EM, Colombo AL, et al. (2012) Comparison of photodynamic therapy versus conventional antifungal therapy for the treatment of denture stomatitis: a randomized clinical trial. Clin Microbiol Infect. 18(10): e380-8.
- Vladimirov Y, Borisenko G, Borisenko N, Kazarinov K, Osipov A (2000) NO-hemoglobin may be a light-sensitive source of nitric oxide both in solution and in red blood cells. J Photochem Photobiol B. 59(1-3): 115-22.
- Freitas LF, Hamblin MR (2016) Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron. 22(3): 7000417.