Pugh Sean M. DO, Galway Ursula MD*
Department of General Anesthesiology, Anesthesiology Institute, Cleveland Clinic Foundation, Cleveland Ohio, USA.
*Corresponding Author: Galway Ursula MD, Department of General Anesthesiology, Anesthesiology Institute, Cleveland Clinic Foundation, Cleveland Ohio, USA.
Abstract
Management of ventilation in upper airway surgery including tracheal balloon dilation can be achieved through numerous methods. The decision of which strategy to use depends on a multitude of factors including procedure type, operative time, the experience of the anesthesiologist and surgeon alike, as well as patient-specific anatomical and physiologic factors. The objective of this case report is to highlight one such method, intermittent ventilation, in the management of a 50-year-old female patient with a history of Left Ventricular Device (LVAD) and right heart dysfunction undergoing tracheal balloon dilation. We report the successful use of intermittent ventilation as a management strategy to prevent hypoxic and hypercarbia pulmonary vasoconstriction.
Keywords: Ventilation management; Intermittent ventilation; LVAD; tracheal dilation; hypercarbia
Abbreviations
LVAD – left ventricular assist device
MLT – micro laryngeal tube
ETCO2 - end tidal carbon dioxide
Introduction
There are many airway management techniques and ventilatory strategies that Anesthesiologists may employ during tracheal balloon dilation, all of which come with their own benefits and risks, even in otherwise healthy patients. Detailed understanding of a patient’s specific anatomy and physiology is vital in determining which strategy to use. One such physiologic state is that of an implanted Left Ventricular Device (LVAD). Management of patients with an LVAD for non-cardiac surgery requires an understanding of pertinent physiologic principles, such as afterload sensitivity and preload dependence, which guide anesthetic decision-making. Since right heart function remains unsupported in LVAD patients, it is important to understand the pre-operative function of the right ventricle in order to inform overall anesthetic decisions that are made for the patient which include proper airway and ventilatory management [1]. We present a case of safe and effective intermittent ventilation in a patient with an LVAD and signs of right heart dysfunction undergoing tracheal dilation for tracheal stenosis.
Case Report
A 50-year-old female admitted with suspected gastrointestinal bleeding and stridor was found to have moderate-severe tracheal stenosis on a CT scan. Her past medical history included paroxysmal atrial fibrillation, ST-elevation myocardial infarction requiring 2 drug-eluting stents, complicated by refractory shock requiring placement of an LVAD for destination therapy. Her course was also complicated by respiratory failure requiring prolonged intubation and ultimately tracheostomy, which was in place for approximately 2 months. The tracheal stenosis was likely due to previous prolonged intubation and prior tracheostomy. She had since been decannulated. Direct laryngoscopy and balloon dilation of her stenotic lesion was planned. A pre-operative transthoracic echocardiogram was obtained which demonstrated right ventricle dilation and decreased right ventricular systolic function.
The patient was brought to the operating room and placed in the supine position. She was accompanied by the institution's LVAD assistant nurse. Standard ASA monitors were applied. Non-invasive blood pressures were obtainable with a standard blood pressure cuff, however, we opted to place an arterial line for invasive blood pressure monitoring. An arterial line was placed with the assistance of an ultrasound probe.
After appropriate pre-oxygenation, anesthesia was induced with 20mg etomidate, 60mg lidocaine, and 40mg rocuronium. An additional 10mg of dexamethasone was given in anticipation of airway edema. Anesthesia was maintained with a Propofol infusion running at 75mcg/kg/min. Mask ventilation was found to be easy. When the patient was fully paralyzed, the airway was handed over to the ENT surgeons. Our plan was to use intermittent ventilation with a size 4 MLT endotracheal tube during the procedure to ensure the patient would neither become hypoxic or hypercarbia.
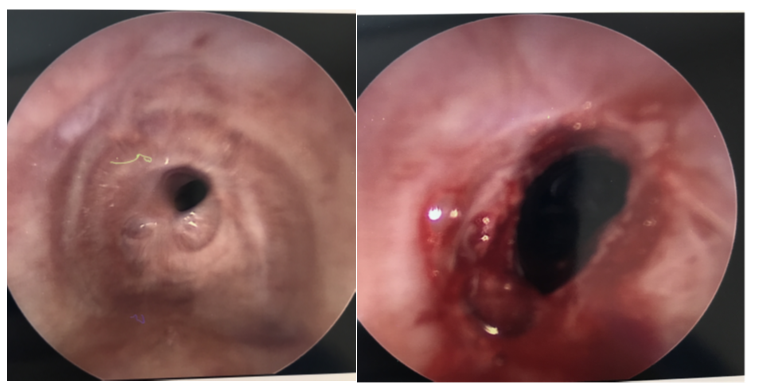
The teeth were protected and a Dedo laryngoscope was placed without difficulty. A Hopkins rod was used to evaluate the larynx and trachea and was used for microscopic visualization for the remainder of the case. The trachea was found to be approximately 85 % stenosed at the 4th tracheal ring. Steroid injection was attempted but the area of stenosis was found to be too inferior. Scissors were then used to make an incision at 3, 7, and 12 o’clock. A 14mm balloon dilator was then utilized the dilate the stenosis. (Figure 1) The size 4 micro laryngeal tube (MLT) was used on one occasion to ventilate during the case. The tube was inserted 3 minutes after the introduction of the Dedo laryngoscope as oxygen saturation was 91 % at that time. The highest recorded end-tidal carbon dioxide (ETCO2) when the MLT was inserted was 38 mmHg. She was ventilated for 2 minutes until her oxygen saturation improved to 99 %. The 4 MLT was then removed, and the procedure was completed. The vocal folds were sprayed with lidocaine and the laryngoscope was removed. The patient was reversed with 200mg sugammadex and mask ventilated until fully awake. The entire procedure took 8 minutes from the introduction of the Dedo laryngoscope to the removal of the laryngoscope. The patient remained hemodynamically stable throughout the procedure. The patient emerged uneventfully from anesthesia and recovered back in her ICU room.
Figure 1: Subglottic stenosis pre and post dilation
Discussion
Commonly used strategies for airway management and ventilation in airway surgeries, including tracheal dilation, include intermittent ventilation, jet ventilation, and high-flow nasal oxygenation, among others [2]. The choice of which strategy to use involves discussion with the surgical team, knowledge of patient-specific pathology and physiology, and comfort of the anesthesia provider in performing each strategy.
There are many advantages of Jet ventilation. These include providing oxygenation and ventilation without tracheal instruments that may obstruct the surgeon’s view [3]. Gas exchange is typically adequate and relies on passive expiration. The main disadvantages of jet ventilation are the lack of tidal volume that is set and the ability to manipulate ventilation parameters in order to maintain specific carbon dioxide levels. This can become problematic in patients highly sensitive to the physiologic changes associated with hypercarbic pulmonary vasoconstriction and rising ETCO2 levels.
High-flow nasal oxygenation (HFNO) was considered as a strategy for this specific case, but due to concerns of increased aerosolization of respiratory secretions due to high flows and the early stage of COVID 19 viral pandemic at the time, this method was not utilized.
An alternative strategy, which was employed during this case, is intermittent ventilation. Intermittent ventilation relies on the use of an endotracheal tube and periods of positive pressure ventilation followed by apnea with passive oxygenation through the use of a nasal cannula. The advantage of this method is the ability to control precise parameters such as respiratory rate and tidal volume in order to respond to changes in ETCO2 levels [3]. This allows for control of inspired oxygen content and active expiration of CO2 which may attenuate hypercarbia or hypoxic pulmonary vasoconstriction. Pulmonary vasoconstriction can worsen right heart failure, which will, in turn, decrease blood flow to the left ventricle which is essential for the ongoing function of the LVAD
In conclusion, we describe the successful use of intermittent ventilation as a method for ventilation in a patient undergoing direct laryngoscopy and tracheal dilation with known right heart dysfunction and an LVAD. Utilizing a micro laryngeal tube for controlled ventilation should be considered as an option that allows for avoidance of both hypoxic and hypercarbia pulmonary vasoconstriction that may worsen overall right heart function.
Conflicts of interest: None
Funding source: None
References
- Chung, M (2018) Perioperative Management of the Patient With a Left Ventricular Assist Device for Noncardiac Surgery. Anesthesia & Analgesia. 126(6): 1839-1850.
- Pathak V, Welsby I, Mahmood K, Wahidi M, Macintyre N, et al. (2014) Ventilation and Anesthetic Approaches for Rigid Bronchoscopy. Annals of the American Thoracic Society. 11(4): 628-634.
- Ahuja S, Cohen B, Hinkelbein J, Diemunsch P, Ruetzler K (2016) Practical anesthetic considerations in patients undergoing tracheobronchial surgeries: A clinical review of current literature. Journal of Thoracic Disease. 8(11): 3431-3441.