Isabela Cristina Coelho da Cunha e Castro1*, Ariane Furbringer2, Amanda Eduarda Nitchai2, Flavia Turmena Baggio2, Gabriela Dal Piva2, Glauco Araujo de Oliveira2, Júlia Casanova Vinhaga2, Leticia Woinarovicz2 and Lucas Souza Schaedler2
1Professor at Medical School, University of Vale do Itajaí
2Student at Medical School, University of Vale do Itajaí
*Corresponding Author: Isabela Cristina Coelho da Cunha e Castro, Professor at Medical School, University of Vale do Itajaí.
Case Report
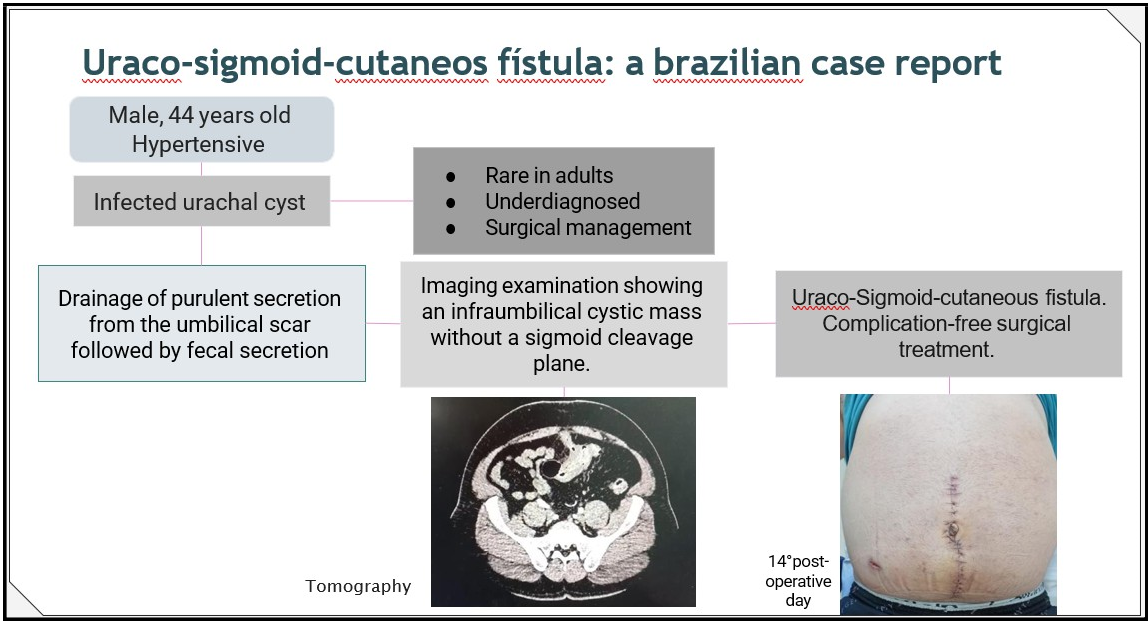
We describe the treatment of a patient with an enteral urachal fistula with months of development. A 44-year-old hypertensive male presented with an umbilical inflammation, initially diagnosed as an infected urachal cyst. He was medically treated and elective surgery was recommended. After a year, the patient sought emergency reporting daily occurrences of purulent and fecal discharge from the umbilicus, leading to the diagnosis of a uraco-sigmoid- cutaneous of unknown origin. Antibiotic therapy was initiated, and rectosigmoidectomy with en-bloc resection and primary anastomosis were performed. Pathological examination confirmed the absence of malignancy. Postoperative recovery was uneventful, and the patient was discharged on the seventh day, with no early or late complications observed on ambulatorial control. Data were collected from the medical records, diagnostic imaging, and a literature review. This case underscores the importance of an accurate diagnosis and timely intervention to prevent negative impact on life quality.
Keywords: Intestinal Fistula; Cutaneous Fistula; Urachal Cyst
Author Note
We have no known conflict of interest to disclose.