M. Moumni*, J. Oubenjah, G. El Amri, H. Ould Cheikh El Wely, A.H. Da Costa, A. Ftouhi, G. Zakaria, M. Zalagh, S. Ouraini, A. Jahidi, B. Hemmaoui, N. Errami, F. Benariba
ENT and CCF service of the Mohammed V military training hospital in Rabat – Morocco
*Corresponding Author: M. Moumni, ENT and CCF service of the Mohammed V military training hospital in Rabat - Morocco
Abstract
Retropharyngeal tuberculosis is a rare localization of tuberculosis. It is clinically characterized by dysphonia and odynophagia and may in some cases remain asymptomatic. The diagnosis is based on imaging, bacteriology, and anatomic pathology.
We report the case of a patient who was admitted to our department for a retropharyngeal abscess and her surgical and medical management.
Keywords: retropharyngeal abscess – tuberculosis – surgical drainage – anti bacillary
1. Introduction
A retropharyngeal abscess is an infection in one of the deep spaces of the neck. It is rare in adults and can occur following local trauma, such as ingestion of a foreign body (fishbone) or instrumental interventions (laryngoscopy, endotracheal intubation, placement of a feeding tube, etc.), or in the specific context of associated disease.
Involvement of the posterior wall of the pharynx is rare but potentially serious, particularly because of its consequences on swallowing and especially on breathing. Retropharyngeal abscesses require rapid diagnosis and early management which frequently involves surgical drainage to achieve the best results.
The present study reviews, through a case of cold retropharyngeal abscess revealing pharyngeal tuberculosis, our experience in the management of these abscesses.
2. Clinical case
We report the case of a young 21-year-old patient with a CHIARI type II malformation as ATCDS for which she was operated on in 2018, lymph node tuberculosis in 2019 who received anti-tuberculosis treatment.
Admitted to the emergency room of the Mohammed V military instruction hospital for intense and permanent chronic headaches evolving for 01 months and associated with fever and unquantified weight loss without dysphagia or dyspnea
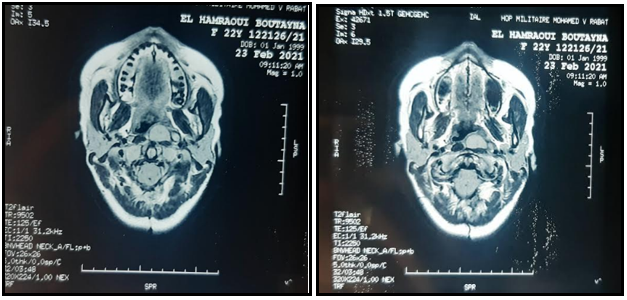
A cerebral CT showed a retropharyngeal collection enhanced peripherally after injection of PDC measuring 19 * 21 mm with adjacent necrotic adenopathy of 10 * 6 mm (Figure 1)
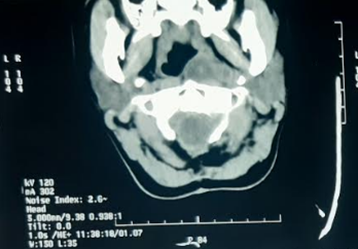
Figure 1: axial section of a cerebral computed tomography showing the retropharyngeal collection
She was hospitalized in the ENT and CCF departments for treatment.
The oropharyngeal examination objectified a bulging of the left posterolateral wall of the pharynx pushing back the ipsilateral tonsillar compartment. (Figure 2)
Cervical examination revealed no palpable lymphadenopathy.
The biological assessment was kept. The HIV serology was negative and the search for BK in the sputum came back negative
A cervical MRI objectified at the level of the left retropharyngeal space of two contiguous collections, in hyposignal T1, hyper signal T2, enhancing in the periphery after injection of Gadolinium, containing multiple partitions and extended over 15*26*47 (from the clivus to C3) suggesting a cold abscess. (Figure 3)

Figure 2: Endoscopic image showing the bulging of the left posterior wall of the oropharynx
The diagnosis of a cold retropharyngeal abscess was retained.
The patient underwent surgical drainage of the retropharyngeal abscess under general anesthesia bringing back a purulent liquid.
Detection of Mycobacterium tuberculosis by PCR (gene Xpert) came back positive with detection of resistance to rifampicin and culture on Löwenstein medium found Koch's bacilli. Histological examination revealed a morphological aspect of a necrotizing granulomatosis reaction with a caseous appearance in favour of tuberculosis.
The patient was put on anti-bacillary quadruple therapy combining rifampicin (10 mg/kg per day), isoniazid (5 mg/kg per day), pyrazinamide (30 mg/kg per day), ethambutol (15 mg/kg per day) for two months, then dual therapy combining rifampicin and isoniazid for seven months with a very good clinical and biological outcome.
Figure 3: axial sections of a cervical MRI showing the retropharyngeal abscess in T1 and T2
3. Discussion
The location of tuberculosis is pulmonary in 80 % of cases and extra-pulmonary (TEP) in 20 % of cases. PET mainly affects the lymph nodes (84.9 % of cases), and the intestines (8.7 %). [1]
ENT impairment is encountered in 9.73 % of cases.
Tuberculosis of the pharynx is a rare condition, accounting for 0.97 % of cases.
It is not uncommon to encounter different associated forms, yet isolated involvement of the posterior wall of the pharynx is possible. [2]
In addition to the military form of the pharynx, many authors report cases of abscessed collections involving the posterior wall of the pharynx. [3]
It is most often secondary to ingestion of a foreign body or trauma to the posterior pharyngeal wall. The tuberculous origin should be systematically sought, especially if it is a cold abscess [4]
The age of onset of tuberculosis in the oropharynx has two peaks at 30 and 60 years for Zanaret et al for all ENT locations [5]. Lecointre et al presented an age range of 15 to 87 years [6]
Women are the most affected, with a sex ratio of 0.66 [3]
There are three classic modes of contamination of tuberculosis, namely hematogenous, lymphatic and airborne. The lymphatic and hematogenous pathways would be involved in the pharyngeal localization observed in our patient. [3]
Clinical diagnosis can be difficult. The clinical symptomatology is variable and nonspecific, made up mainly of signs reflecting oropharyngeal compression: dysphagia, odynophagia, modification of the timbre of the voice or dyspnea. Signs of tuberculous impregnation are not systematically found [7]
The differential diagnosis is made with cancer of the pharynx as well as with other causes of granulomatosis of infectious origin or not [8]
CT and MRI are very useful for diagnosis by showing a retropharyngeal abscess, its reports and especially the pharyngeal extension of a lesion of the cervical spine (Pott's disease) [9]
The diagnosis of retropharyngeal tuberculosis is bacteriological and/or histological. The field of immunosuppression must always be sought. It can be diabetes, an infection with the acquired immunodeficiency virus. [10]
Treatment aims to eradicate the infection and restore swallowing function. [11]
The treatment is essentially medical. In advanced stages, surgery is indicated, such as incision – drainage of an abscessed collection from the posterior wall of the pharynx.
The prognosis under treatment is very favourable, with total recovery without sequelae [12]
Nevertheless, it remains a therapeutic emergency because of its complications if not well treated.
The high mortality rate associated with retropharyngeal abscess is due to its association with airway obstruction, mediastinitis, aspiration pneumonia, epidural abscess, jugular vein thrombosis, necrotizing fasciitis, sepsis, and erosion of the carotid artery. [10]
In a study of 234 adults with deep-space neck infections in Germany, the mortality rate was 2.6 %. The cause of death was primarily sepsis with multiple organ failure. [13]
4. Conclusion
Retropharyngeal tuberculosis is a rare condition, revealed by dysphonia but especially by dragging or chronic odynophagia; however, the clinical picture may be silent.
The diagnosis is pathological, confirmed by the presence of AFB in other locations aided by imaging (CT and MRI)
The treatment is essentially medical, surgery is an exceptional indication.
The prognosis under treatment is very favourable, with total recovery without sequelae.
References
- Talukder MS, Huq MH, Haque A, Sarker CB (2002) Extrapulmonary tuberculosis in surgical specimens. Mymensingh Med J. 11(2): 104-6.
- Nalini B, Vinayak S (2006) Tuberculosis in ear, nose, and throat practice: its presentation and diagnosis. Am J Otolaryngol. 27(1): 39-45.
- A.H.N. Rakotoarisoa, A.M. Andrianarivelo, N.N.M. Razafimanjato, N.P. Ramarozatovo, F.A. Rakoto A case of disseminated tuberculosis revealed by pharyngeal localization La Revue Médicale de Madagascar 2011;1(2):33-35.
- M. Elqatni, Y. Sekkach, S. Hammi, N. Elomri, J. Fatihi, F. Mekouar, M. Badaoui, T. Amezyan, A. Abouzahir, D. Ghafir, V. Ohayon A retropharyngeal abscess; the journal of internal medicine Vol 32 - N° 5 P. 319-320 - May 2011.
- Zanaret M, Dessi P. Tuberculosis of the pharynx. Encycl. Med. Chir. (Paris-France), Oto-Rhino-Laryngology 1992; 20575A10: 1-2.
- Lecointre F, Marandas P, Micheau C, et al. Head and neck mucosal tuberculosis, clinical study about 37 cases followed at the IGR (Institut Gustave Roussy). Ann Otolaryngol Chir Cervicofac 1980; 97: 423-33.
- Benhammou A, Bencheikh R, Benbouzid MA, Boulaich M, Essakali L, Kzadri M. Retropharyngeal abscess revealing cervical Pott's disease. Rev. Stomatol Chir Maxillofac 2007; 108: 543–6.
- Gousseff M, Mechaï F, Lecuit M, Lortholary O (2008) Systemic granulomatoses of infectious origin. Rev Med Internal. 29(1): 15-27.
- Portier F, Nowak C. Pharyngeal tuberculosis. Paris, EMC, 20-575-A-10.
- Harkani A, Hassani R, Ziad T, Aderdour L, Nouri H, et al. (2011) Retropharyngeal Abscess in Adults: Five Case Reports and Review of the Literature. The Scientific World JOURNAL. 11: 1623–1629.
- API TB Consensus Guidelines 2006: Management of pulmonary tuberculosis, extra-pulmonary tuberculosis and tuberculosis in special situations. J Assoc Physicians India. 54: 219-34.
- Kharoubi S. Miliary tuberculosis of the pharynx or Isambert's disease. Ann Otolaryngol Chir Cervicofac 2008; 125: 213–8.
- Ridder GJ, Technau-Ihling K, Sander A, Boedeker CC (2005) Spectrum and management of deep neck space infections: an 8-year experience of 234 cases. Otolaryngology—Head and Neck Surgery. 133(5): 709–714.