José Alexandre da Rocha Curvelo1,2*, Brenda Xavier1, Ana Clara Elbert1, Maria Elisa Rangel Janini1
1Department of Oral Pathology and Oral Diagnosis, School of Dentistry Federal University of Rio de Janeiro. 325 Prof. Rodolpho Paulo Rocco St., University City, 21941-617, Rio de Janeiro, RJ, Brazil.
2Department of General Microbiology, Institute of Microbiology, Federal University of Rio de Janeiro. 373 Carlos Chagas Filho Avenue, University City, 21941-902, Rio de Janeiro, RJ, Brazil.
*Corresponding Author: José Alexandre da Rocha Curvelo, Department of Oral Pathology and Oral Diagnosis, School of Dentistry Federal University of Rio de Janeiro. 325 Prof. Rodolpho Paulo Rocco St., University City, 21941-617, Rio de Janeiro, RJ, Brazil.
Abstract
Oral mucocele is a common benign pathology that affects minor salivary glands. It has a traumatic origin and is characterized by disruption or obstruction of a salivary gland duct causing mucin accumulation in underlying tissue. Clinically, oral mucocele is normally observed as a node or blister of variable size with floating consistency with a smooth and bright surface. Normally, it affects the lower lip of young patients varying from a few millimeters to one centimeter. Considering the usual aspects of this lesion, this article aims to report an atypical case of an oral mucocele measuring four centimeters located in the anterior cheek mucosa of a fifty-three-year-old patient, with no history of local trauma. Therefore, this report highlights that oral mucocele can present themselves in atypical manners impairing the establishment of initial diagnosis and should be considered as a differential diagnosis of submerged lesions in the oral cavity even when it does not meet the general diagnostic criteria.
Keywords: oral mucocele, differential diagnosis, salivary glands, atypical presentation, misdiagnosis, mucous retention cyst
Introduction
Oral mucocele (OM) is a very common benign minor salivary glands pathology, whose etymological definition means mucus-filled tumor [1]. In fact, it represents a clinical manifestation of two distinct phenomena that can involve these glands, the mucus leakage and the mucus retention, this latter one resembling common cystic characteristic [2-4]. Mucus overflow is normally caused by trauma or parafunctional habits that lead to the rupture of a salivary duct and consequently mucus congestion in adjacent tissue. On the other hand, mucus retention is the result of a salivary duct occlusion causing saliva accumulation inside itself. Despite the fact that both etiologies have similar clinical characteristics mucus extravasation leads to the accumulation of fluids produced by the acinos in the connective tissue surrounding the affected gland forming a cavity without epithelial lining or a pseudocyst, whereas in mucus retention, the obstruction of the excretory duct occurs by sialolithiasis or by scar tissue contraction after a traumatic injury. In this latter case, a true cyst occurs with expansion delimited by epithelium [5-8].
Clinically, OMs are normally observed as a blister or a submerged node, with variable size, soft on palpation, with a smooth and bright surface that can be bluish, translucent, or normochromic depending on its depth in tissues [9]. In general, OMs are presented on physical examination, as an asymptomatic swelling ranging from a few millimeters to 1.5 centimeters, circumscribed, dome-shaped, with floating consistency, which may cause discomfort in speech, chewing, and swallowing. They are predominantly located in the lower lip and occur more frequently in children and young adults, probably because they are more prone to trauma experiences due to the cusp formation of dental elements [5].
Complete surgical excision is normally the chosen treatment, and it must be done associated with the removal of any minor salivary gland involved in order to minimize the possibility of recurrence. However, the lesion size, extent, and depth, as well as the age of the patient are important parameters that should be considered to determine the best therapeutic technique [10]. Nevertheless, the spontaneous rupture of OM is not uncommon, spilling out the mucous content making the mucosal surface ulcerated which tends to heal within a few days [11]. Histopathological, 92 % of OMs are caused by mucus leakage and can be analyzed as a cavity filled with spilled mucin surrounded by connective or granulation tissue not coated by epithelium, i.e., a pseudocyst [12]. The intraductal or extra ductal accumulation of mucus causes inflammation in the surrounding tissues leading to the presence of Achantomatous macrophages and inducing granulation tissue formation that forms a fibrous capsule around the mucin deposit [13]. On the other hand, retention cysts represent only 8% of the cases, where a simple or stratified epithelium lining can be seen surrounding mucous content [12].
The preliminary diagnosis of OM is normally made based on the anamnesis and the clinical examination, considering properly features of the patient and the lesion itself, such as location, history of previous trauma, appearance, variations in size, color, and consistency. Yet, the definitive diagnosis must be established through histopathological analysis [14]. In some cases, fine needle aspiration and exploratory puncture can be performed to improve diagnosis arsenal by the aspiration of mucus, histiocytes, and inflammatory cells [15]. Nevertheless, since OMs are clinically similar to several other oral pathologies, the elaboration of a differential diagnosis cast must be made and should include benign and malignant salivary glands neoplasms, as well as lipoma, fibroma, lymphoepithelial cyst, adult gingival cyst, cysticercosis, and bullous lichen planus [11,16]. Notwithstanding, many agree that the appearance of OM is pathognomonic, and this appearance associated with the location, history of trauma, color, and consistency can determine the diagnosis of this pathology [8,17-18].
Considering the exposure, the objective of this study is to report a clinical case of OM discrepant of the parameters normally found in the literature.
Case Report
A male with 53 years old, was attended at the clinic of Stomatology of the School of Dentistry, Federal University of Rio de Janeiro, Brazil complaining of a large and painless swelling located in the internal mucosa of the cheek, with 20 days of evolution. During the anamnesis, the patient did not remember any history of local trauma. He declared that he has no significant medical history, systemic disease, allergy, or the use of systemic medications. Finally, he reported being a heavy smoker for the past 30 years.
On intraoral clinical examination, the presence of a large submucosal nodule, located in the left anterior cheek mucosa, measuring 4 cm in its largest diameter, normochromic, with floating consistency and smooth surface was observed (Figure 1). On extraoral clinical examination, no abnormalities were detected.

Figure 1: First intraoral clinical examination revealed a large normochromic nodular lesion located in the left anterior cheek mucosa.
Based on the clinical characteristics associated with the information collected in anamnesis, the hypothetical diagnosis was OM, mucoepidermoid carcinoma, and traumatic fibroma. After the clinical examination, an aspiration puncture was performed, and intralesional mucous content was obtained, pointing to the first diagnostic hypothesis of OM. Thus, the treatment chosen was excisional biopsy with complete surgical removal.
The surgical intervention was performed under local anesthesia, with 2 % lidocaine with epinephrine 1:200.000, resulting in the excision of the lesion, and the underlying accessory glands (figure 2A). Specimen obtained were referred for histopathological analysis (figure 2B). Microscopic examination of excised tissue revealed an area of spilled mucin, surrounded by granulation tissue, corresponding to a typical OM microscopic appearance (Figure 3) confirming the diagnosis of OM caused by mucus leakage.
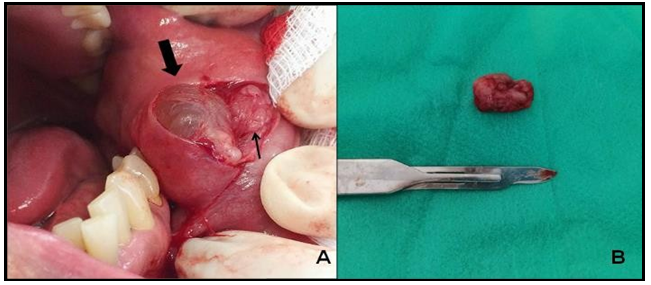
Figure 2: Surgery procedure, (A) before its removal, the pseudocapsule of the exposed mucocele could be seen (large arrow) associated with an accessory gland (thin arrow). (B) Gross features and microscopic aspects of the specimen removed.
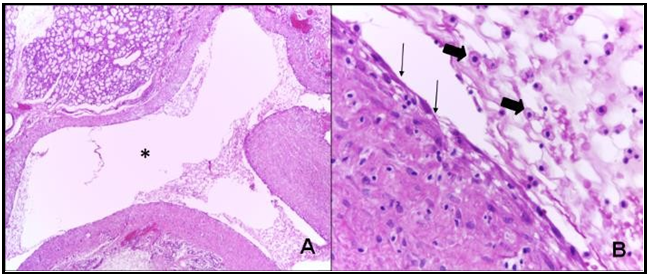
Figure 3: Histopathological analysis revealed (A) an area of spilled mucin, surrounded by a cavity not covered by epithelium (*), corresponding to a typical mucocele microscopy aspect and (B) a pseudocapsule composed by connective tissue (thin arrow) and chantomatous macrophages (large arrow) (HE; A x100; B x400).
Discussion
OM is a common benign pathology widely diagnosed, with usual parameters that form a well-established diagnostic criterion. However, uncommon clinical characteristics like the ones reported in this case may lead clinicians to confuse empirical interpretation misleading initial and differential diagnosis. Therefore, in order to address the rare peculiarities reported in this case, such as the patient's age, the history of previous trauma, the dimension, and the location where the lesion was established, we highlight these specific points to be considered atypical and to be discussed from now on.
It is well known that OM affects children and young adults more frequently, especially between the first and second decades of life, and, but rarely on children under one year old [12,14]. However, they have already been reported in all ages, from babies to older adults, despite the very lower incidence [19]. In this report, the patient was 53 years old, pointing to only 1 % frequency of OM classifying the exposed case as extremely uncommon [20-21].
Previous studies have already noticed that OM dimensions normally range from a few millimeters to 1.5 centimeters in 93 % of the cases, with a mean of 0.8 cm in its maximum diameter [19]. Opposing to previous literature, the case presented here shows an OM measuring 4 cm in its largest diameter. Thus, based on this information, the present case is also atypical considering its proportions as well.
OMs are located predominantly on the lower lip, but can also be found on the upper lip, tongue, cheek mucosa, and, more rarely, in the retromolar region and on the palate. They rarely affect anterior lingual salivary Blandin-Nuhn glands located in the central portion of the tongue [3,14,18]. In fact, an extensive study with 1,824 cases revealed that 81% of the cases occurred in the lower lip, and much less frequently on the floor of the mouth (5.8 %), ventral portion of the tongue (5.7 %), on the cheek mucosa (4,7 %) and on the palate (1.4 %) [19]. This high frequency may be explained by the fact that the mucus leakage phenomenon, in its great majority, occurs from the result of the rupture of the minor salivary ducts caused by parafunctional habits, such as lip biting or trauma [5,19]. Nevertheless, literature also agrees that OM can occur in any region susceptible to trauma or obstruction of a salivary gland duct, rarely happening on atypical locations such as the cheek mucosa, however, it is liable to occur [20,21]. Based on such information, and even with the agreement of previous reports, we consider that the exposed case is also unusual in terms of location.
As previously said in this report, OM represents the clinical manifestation of two distinct phenomena, mucus leakage and mucus retention that are etiologically and histopathologically distinct [2-4,22]. Indeed, previous systematic reviews identified that 97.1 % of OM were diagnosed as a mucus leakage phenomenon and only 2.9 % were diagnosed as a mucus cyst. Furthermore, the proportion between lesions caused by mucus extravasation and renal cysts has already been established in 15:1 [19,23]. Thus, we observed that the reported case has its histopathological characteristics coinciding with the reports in the literature about mucus retention phenomena, and thus being considered not atypical regarding its etiology.
Considering that the patient did not refer to any trauma episode and only noticed the volume increasing in his mouth in a period of 20 days, there was an absolute necessity to consider differential diagnosis for this case. Among the various diagnostic hypotheses, traumatic fibroma and salivary gland neoplasm and malignancies should be included [7]. Therefore, considering the clinical characteristics observed in the intraoral examination, associated with patient age, heavy tab agism, and the absence of trauma history, a hypothesis of mucoepidermoid carcinoma (MC) was also considered.
MC is the most frequent salivary gland cancer in the oral cavity, comprising 9% of all malignancies related to the salivary gland, but most frequently observed in larger ones such as parotids [24-25]. Clinically MC may manifest with a slow-evolving swelling, usually asymptomatic, but eventually associated with superficial ulceration. MC of accessory salivary glands usually present themselves with edema, sometimes with floating consistency and blue or normochromic coloration, all these characteristics in this specific case could have been easily jumbled the establishment of the real diagnosis of OM [26].
Traumatic fibroma was another differential diagnosis considered in this case, mainly due to the lesion location. Traumatic fibroma is a benign oral pathology quite commonly caused by repetitive trauma events in the same site, resulting in a chronic mucosal repair process, with no risk of malignancy. The most common site is the mucosa of the cheek along the dental bite region, followed by the tongue and lower lip. Clinically, it is presented as a fibrous submucosal swelling with a broad base, normochromic or whitish surface due to hyperkeratosis and in some cases may be ulcerated by secondary trauma. Its size can vary from 1 to 2 cm in diameter. Furthermore, they are more common in the fourth to sixth decades of life and the male-to-female ratio of the cases submitted to biopsy stays at 1:2 [27].
After considering OM as the first diagnosis hypothesis, followed by MC and traumatic fibroma, an aspiration puncture was performed and revealed a viscous, thick, and translucent content similar to saliva which pointed to the strong possibility of OM as a definitive diagnosis. For that reason, a treatment strategy was planned to aim at the complete removal of the nodule, as well as any minor salivary gland that could be associated. Many surgical treatments for OM have already been proposed such as complete excision, marsupialization, micro marsupialization, and cryosurgery [1,14,28]. However, most authors considered that they must be removed entirely with the associated minor salivary gland to provide a better prognosis and avoid recurrences. Nevertheless, micro marsupialization has been proposed for pediatric patients, considering that this technique is simple, quick, and allows the leakage of mucous content until its regression gets a high success rate for this population [29-31].
Resuming all the information discussed in this case report, we can highlight three relevant unusual OM features:
The patient age, despite the consensus that OM can affect all ages, most of the literature indicates that the young adults and children population is more affected by this pathology. In fact, very few similar records of OM cases affecting patients in the 53 years old age group were observed.
The location, even though most literature points to the lower lip as the most frequent region affected by OM, can be located in any region of the oral mucosa susceptible to salivary duct rupture or obstruction but being very less common. Nevertheless, very few records of OM located in the cheek mucosa were observed.
The size, the literature indicates that OM normally ranges between 0.5 and 1.5 cm long, however, no records of similar cases of OM having of 4 cm or higher were observed.
Considering this, we can conclude that although most OM owns classical characteristics, they also may carry a range of peculiarities where singularities such as the ones exposed in this case may lead to clinical misdiagnosis. Therefore, we conclude that OM should be included as a differential diagnosis of submerged lesions in the oral cavity in all cases, even when it does not meet the general diagnostic criteria.
Compliance with Ethical Standards
Conflict of interest: All authors declare that they have no conflict of interest to disclose.
Ethical Approval: This study was carried out following the 1964 Helsinki Declaration for a study involving human subjects.
Informed Consent: Formal informed consent from the patient has been obtained for this case report.
Funding: No funding was obtained
References
- Yagüe-García J, España-Tost AJ, Berini-Aytés L, Gay-Escoda C (2009) Treatment of oral mucocele - scalpel versus C02 laser. Oral Surg Oral Med Oral Pathol. 14(9): 469-74.
- Rebouças DS, Freitas DM, Costa TF, Farias TS, Pereira FB, Assis AF. Mucocele treatment with work Shira’s technique: case report. Rev Odontol Bras Central. 2015; 24(69): 81-3.
- Baurmash, HD (2003) Mucoceles and Ranulas. J Oral Maxillofac Surg. 61: 369-378.
- Bordini PJ, Grosso SFB, Carmo C (2001) Estomatologia na clínica infantil: principais alterações bucais. Assoc Paul Cir Dent. 55(5): 366-370.
- Choi Y-J, Byun J-S, Choi J-K, Jung J-K (2019) Identification of predictive variables for the recurrence of oral mucocele. Med Oral Patol Oral Cir Bucal. 24(2): e231–e235.
- Carneiro-Leão J, Gomes DO. Mucoceles, características clínicas e tratamento. J Radioface, 2001;2(4):4.
- Mustapha IZ, Boucree SA (2004) Mucocele of the upper lip: case report of an uncommon. J Can Dent Assoc. 70(5): 318-21.
- Andiran N, Sarikayalar F, Unal OF, Baydar DE, Ozaydin E (2001) Mucocele of the anterior lingual salivary glands: from extravasation to an alarming mass with a benign course. Int Journal Pediatr Otorhinolaryngol. 61(2): 143-47.
- Kaiser KM, Silva ALT, Rosa TF, Pereira MA (2008) Mucocele em mucosa de lábio inferior. RGO. 56(1): 85-88.
- Santos TS, Martins Filho PRS, Menezes FS, Maia MC, Carvalho RWF, et al. (2008) Tratamento cirúrgico de mucocele utilizando a técnica de Shira: relato de caso. UFES Rev Odontol. 10(4): 53- 58.
- Gupta B, Anegundi R, Sudha P, Gupta M (2007) Mucocele: Two Case Reports. J Oral Health Comm Dent. 1(3): 56-58.
- Stuani AS, Silva FWGP, Stuani MBS, Valério RA, Queiroz AM (2010) Mucoceles: lesões frequentes na cavidade bucal de crianças. Pediatria. 32(4): 288-292.
- Alves L, Nicoló R, Ramos C, Shintome L, Cristiani B. Mucocele retenção no lábio inferior, associado com o uso inadequado de chupetas. Dermatol Online J. 2010;16(7): 1-5.
- Ata-Ali J, Carrillo C, Bonet C, Balaguer J, Peñarrocha M (2010) Oral mucocele: review of the literature. J Clin Exp Dent. 2(1): 18- 21.
- Layfield LJ, Lopez EV (2002) Cystic lesions of the salivary glands: cytologic features in fine-needle aspiration biopsies. Diagn Cytopathol. 27(4): 197-204.
- Câmara LP, Santos VIM, Menezes VA, Neves HLS (2002) Mucocele: relato de caso clínico. J Bras Odontoped Odontol. 5(27):378-81.
- Bentley JM, Barankin B, Guenther LC (2003) A review of common pediatric lip lesions: herpes simplex/recurrent herpes labialis, impetigo, mucoceles, and hemangiomas. Clin Pediatr (Phila). 42: 475-82.
- Guimarães MS, Hebling J, Filho VA, Santos LL, Vita TM, et al. (2006) Extravasation mucocele involving the ventral surface of the tongue (glands of Blandin-Nuhn). Int J Paediatr Dent. 16(6): 435-39.
- Chi AC, Lambert PR, Richardson MS, Neville BW (2011) Oral mucoceles: a clinicopathologic review of 1,824 cases, including unusual variants. J Oral Maxillofac Surg. 69(4): 1086-93.
- Rashid AK, Anwar N, Asisah AM, Narayan KA (2008) Cases of mucocele treated in the dental department of Penang hospital. Arch Orofacial Sci. 3(1): 7-10.
- Jani DR, Chawda J, Sund-Aragiri SK, Parmar G (2010) Mucocele: A study of 36 cases. Indian J Dent Res. 21(3): 337-40.
- Largura LZ, Grando LJ, Rau LH, Gil JN (1998) Remoção cirúrgica de mucocele. Rev Assoc Paul Cir Dent. 52(6): 435-8.
- Esmeili T, Lozada-Nur F, Epstein J (2005) Common benign oral soft tissue masses. Dent Clin N Am. 49(1): 223–40.
- Santos TS, Melo DG, Andrade ESS, Silva EDO, Gomes ACA (2012) Carcinoma mucoepidermóide no palato: relato de caso. Rev Port Estomatol Med Dent Cir Maxilofac. 53(1): 29–33.
- Lee WH, Yoon JH (2003) Mucoepidermoid carcinoma of the hard palate: a rare cause of hypervascular tumor. Yonsei Med J. 44(4): 723–6.
- Munhoz EDE, Cardoso CL, Tjioe KC, Sant’ana E, Consolaro A, et al. (2009) Atypical clinical manifestation of mucoepidermoid carcinoma in the palate. Gen Dent. 57(6): e51–3.
- Gonsalves WC, Chi AC, Neville BD (2007) Common Oral Lesions: part 2. Masses and Neoplasia. Am Fam Physician. 75(4): 509-512.
- Cecconi D, Achilli A, Tarozzi M, Lodi G, Demarosi F, et al. (2010) Mucoceles of the oral cavity: A large series (1994-2008) and literature review. Med Oral Patol Oral Cir Bucal. 15(4): 551- 6.
- Sagari SK, Vamsi KC, Shah D, Singh V, Patil GB, et al. (2012) Micromarsupialization: a minimally invasive technique for mucocele in children and adolescents. J Indian Soc Pedod Prev Dent. 30(3): 188-91
- Danelon M, Lodi CS, Favretto CO, Crivelini MC, Cunha RF, et al. (2013) Diagnóstico e Tratamento de Mucocele em Odontopediatria: Relato de Caso. Arch Health Invest. 2(5): 47-53.
- Delbem AC, Cunha RF, Vieira AE, Ribeiro LL (2000) Treatment of mucus retention phenomena in children by the micromarsupialization technique: case reports. Pediatr Dent. 22(2): 155-8.



