Maheen Sajid1*, Kunal Rathod2, Michael Magro2, Rajeev Prasad3
1GPST1 Queens Hospital, Romford, London RM7 0AG
2Consultant Obstetrician and Gynaecologist, Queens Hospital, Romford, London RM7 0AG
3Consultant Histopathologist, Queens Hospital, Romford, London RM7 0AG
*Corresponding Author: Maheen Sajid, GPST1 Queens Hospital, Romford, London RM7 0AG.
Introduction
Ovarian fibromas are an uncommon type of ovarian tumour, accounting for approximately 4% of all tumours, and are almost always benign in nature [1]. Their diagnosis is primarily based on pre- operative clinical, sonographic, and radiographic evidence; however, the definitive diagnosis is histological, with surgery being the principal treatment. Although most commonly observed in post- menopausal women, in this case report, we describe the rare incidence of a pre-menopausal woman who underwent laparoscopic surgery for a suspected ovarian fibroma, whilst the histology subsequently revealed corpus albicantia.
Case Report
A 32-year-old female presented initially in 2021 with right-sided lower abdominal pain associated with an offensive discharge. Her history involved one normal vaginal delivery followed by two surgical terminations of pregnancies, regular periods in a 28-day cycle and a normal cervical smear history. An intrauterine device (IUD) was in situ since 2012, which was removed during her attendance to emergency gynaecology due to the possibility of pelvic inflammatory disease (PID).
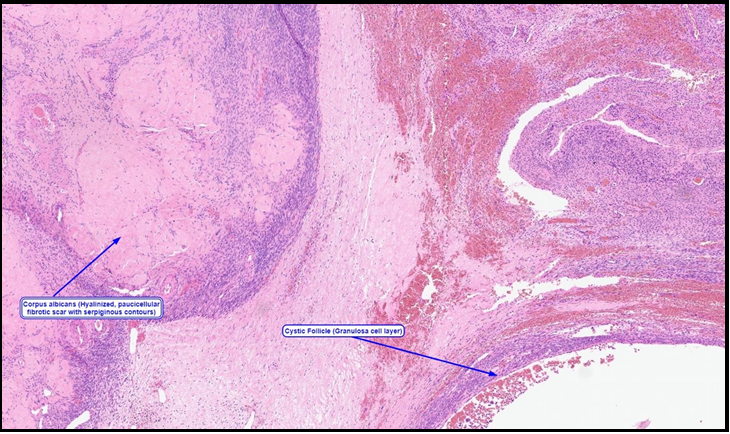
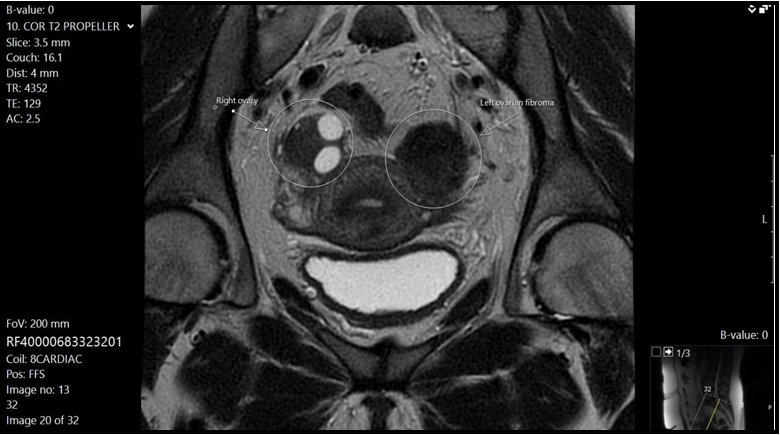
A CT Abdomen & Pelvis was performed which showed a large heterogeneous mass measuring 7.5 x 6.8 x 6cm, with a comment of a possible subserosal uterine fibroid or an ovarian fibroma as a differential diagnosis. Following on from this, the patient underwent an MRI pelvis with contrast which reported a 3 cm-sized low signal intensity area on T2-weighted imaging in the left ovary, suggestive of an ovarian fibroma. The pre-operative Ca-125 levels were normal at 12 besides normal carcino embryonic antigen (CEA), alpha feto protein, lactate dehydrogenase (LDH) and Beta Human chorionic gonadotrophin (Bhcg) Clinical case including all relevant investigations and imaging was discussed in gynae oncology multidisciplinary meeting. Outcome of the meeting was an ovarian fibroma to be excised surgically. Subsequently patient underwent an uneventful laparoscopic left ovarian cystectomy, which she recovered well from. However, her histopathological findings showed a few cystic follicles and large deposits of corpus albicans with focal calcification. The unresorbed corpus corpora albicantia was thought to account for the suspicious radiological findings and mimicking the appearance of a fibroid on imaging.
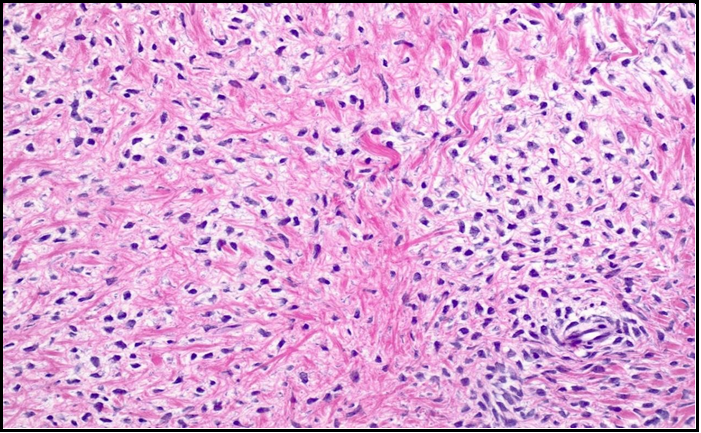
Figure 1: Histology slide of ovarian fibroma showing bland spindle cells lacking cytologic atypia or mitotic activity
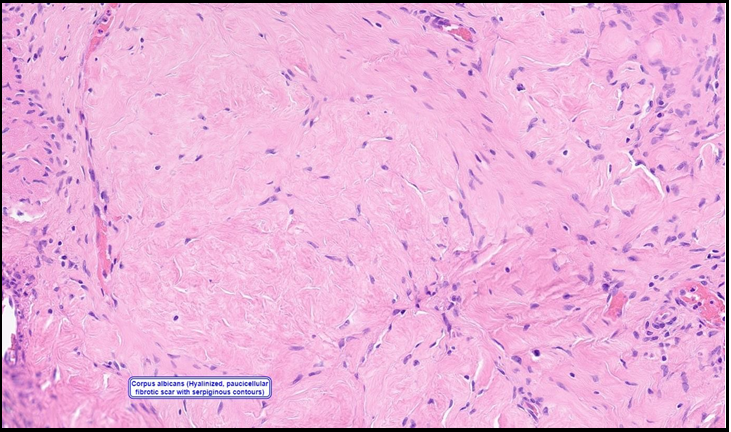
Figure 2: Histology slide of corpus albicantia
Figure 3: Histology slide of corpus albicans and adjacent cystic follicle
Figure 4: MRI T2 coronal image showing hypointensity area on left side suggestive of ovarian fibroma.
Discussion
Solid ovarian masses are of 2 types: sex-cord/stromal and Brenner tumours (otherwise known as transitional cell tumours). Ovarian fibromas fall into the former category, occurring most commonly in the elderly, post-menopausal women [2]. One study reported that above 80% of the women diagnosed with ovarian fibromas were above the age of 40, whilst almost 50% were menopausal [3]. Their discovery can vary in nature, often incidental with the most common symptom reported as pelvic pain. Additionally, it may unfold as part of a complication, such as ovarian torsion, or as part of a syndrome, e.g., Meig’s syndrome (a triad of ovarian fibroma, ascites, and pleural effusion) [2]. Radiographically, ovarian fibromas are found to show typically low signal intensity on T1-weight MR images and marked hypo-intensity on T2- weighted images [4], as described in this case, and can be difficult to distinguish from a uterine myoma [3]. As they develop from connective tissue and muscle fibres, they appear as a well-defined, encapsulated mass that are partly hyalinized [2]. Microscopically, they are solid tumours, comprised of spindly fibroblastic cells arranged in a whirlwind pattern. They may also combine with the lipid-laden theca cells that form thecomas, another form of benign ovarian tumours, to form fibrothecomas [1]. One of the main challenges that exist with the diagnosis of ovarian fibromas is the difficulty in distinguishing between other solid ovarian tumours. Malignant ovarian carcinomas are unlikely to be the cause of a completely solid ovarian mass, as they often contain both cystic and solid components that can be established radiographically. However, other differentials may include extraovarian masses that are mistakenly thought to arise from the ovary, a haemorrhagic ovarian cyst [5,6] or rarely, endometriomas [7]. The case of corpus albicantia appearing as an ovarian fibroma has rarely been described in literature, particularly in pre-menopausal women, but may occur due to calcium deposition such as in this case. Corpus albicans is the remnant of the corpus luteum, after it has been replaced with densely packed collagen fibres which hyalinize, leaving behind fibrous tissue [5]. It is most commonly observed in post-menopausal women due to hormone-related changes, primarily the reduction in oestrogen, in addition to the reduction in immune-mediated phagocytosis and fibroblastic activity.
Consequently, the corpus albicans may persist, as this leads to poor formation and regression of these structures. Furthermore, the deposition of haemosiderin and calcium deposits contributes to its appearance on sonographic and radiographic imaging. Microscopically, it appears as a dense aggregate of connective tissue [8]. In this patient, it is difficult to ascertain the reason for corpus albicantia persisting despite her pre-menopausal status. Previous studies have reported cases of corpus albicantia being mistaken for a fibromyoma [9], however even in retrospect, distinguishing between the two remains a challenge. Ultimately, surgery is the curative treatment for a fibroma due to its low risk of malignancy; most commonly a salpingo-oophorectomy in those who are peri- menopausal or post-menopausal, versus cystectomy in pre- menopausal women, as observed in this case [10].
Conclusion
Ovarian fibromas are an uncommon subtype of benign ovarian tumour, that are notoriously difficult to correctly identify on clinical or radiographical evidence alone. Surgery remains the curative treatment, whilst histology is used for the definitive diagnosis. Corpus albicantia may rarely present in a similar fashion to an ovarian fibroma on imaging, however this is rare in the pre-menopausal women, and the reasoning for this is yet to be explored.
References
- Chechia A, Attia L, Temime RB, Makhlouf T, Koubaa A (2008) Incidence, clinical analysis, and management of ovarian fibromas and fibrothecomas. Obstet Gynecol. 199(5): 473. e1-473. e4.
- Mahtate M, Slaoui A, Lakhdar K, Zeraidi N, Lakhdar A, et al. (2022) Ovarian fibroma in a postmenopausal woman: A case report. MOJ Clin Med Case Rep. 12(4): 56-58.
- Son CE, Choi JS, Lee JH, Jeon SW, Hong JH, et al. (2011) Laparoscopic surgical management and clinical characteristics of ovarian fibromas. JSLS: Journal of the Society of Laparoendoscopic Surgeons. 15(1): 16-20.
- Bouab M, Touimi AB, El Omri H, Boufettal H, Mahdaoui S, et al. (2022) Primary ovarian fibroma in a postmenopausal woman: A case report. International Journal of Surgery Case Reports. 92: 106842.
- Brown DL, Hirsch MS, Muto MG, Laing FC (2004) Unresorbed Corpora Albicantia Mimicking a Sonographically Solid Ovarian Mass in a Postmenopausal Woman. Journal of Ultrasound in Medicine. 23(11): 1523-1526.
- Bonde AA, Korngold EK, Foster BR, Fung AW, Sohaey R, et al. (2016) Radiological appearances of corpus luteum cysts and their imaging mimics. Abdominal Radiology. 41(11): 2270-2282.
- Callen PW (1988) Ultrasonography in obstetrics and gynecology.
- Kirkendoll SD, Bacha D. Histology, Corpus Albicans. StatPearls [Internet]: StatPearls Publishing; 2023.
- Puckette Jr SE, Williamson HO, Seymour EQ (1969) Calcification in an ovarian corpus albicans. Radiology. 92(5): 1105.
- Târcoveanu E, Dimofte G, Niculescu D, Vasilescu A, Moldovanu R, et al. (2007) Ovarian fibroma in the era of laparoscopic surgery: a general surgeon’s experience. Acta Chir Belg. 107(6): 664-669.