Alan Janbey*
Department of Health and Applied Biology, The London College UCK, London, United Kingdom
*Corresponding Author: Alan Janbey, Department of Health and Applied Biology, The London College UCK, London, United Kingdom.
Abstract
Sleep is a fundamental yet enigmatic physiological process essential for human health and function. This paper explores the recent advances in biopsychological research within behavioural neuroscience that shed light on the complexities of sleep. A comprehensive understanding of sleep mechanisms is appearing by integrating genetics, neurobiology, and psychology findings.
Key topics covered include:
The neural circuits governing sleep-wake transitions.
Neurotransmitters such as serotonin and dopamine play a crucial role in regulating sleep.
Sleep has an impact on cognitive processes like memory consolidation and emotional regulation.
Furthermore, we review the influence of external factors like stress, ageing, and environmental cues on sleep quality and quantity. We also examine the interplay between sleep and mental health disorders like insomnia, depression, and anxiety, highlighting bidirectional relationships and potential therapeutic implications. Moreover, the developmental aspects of sleep across the lifespan, from infancy to old age, underscore the evolving nature of sleep architecture and its adaptive functions. Emerging technologies like functional neuroimaging and optogenetics are revolutionising our ability to probe sleep mechanisms with unprecedented precision, offering novel insights into sleep disorders and their underlying pathophysiology. In summary, this abstract provides an overview of how contemporary biopsychological research in behavioural neuroscience unravels the mysteries of sleep, with profound implications for health, cognition, and well-being.
Keywords: Neuroanatomy, Sleep Biopsychology, Clinical Neurology
Introduction
Biopsychological theories highlight the interdependence of biological, psychological, and social elements in influencing human behavior and cognitive processes. Biopsychological theories, such as the one put forth by von Bertalanffy, suggest that biological, psychological, and social elements mutually impact one another and cannot be comprehended in isolation. Hammond (2019) [19] analyses Von Bertalanffy's General Systems Theory and other psychological theories proposed by Sigmund Freud. The field of psychology covers a wide range of theoretical viewpoints and ongoing disputes that have developed throughout time, reflecting shifts in paradigms, societal changes, and advancements in scientific knowledge. In 1895, Freud aimed to merge the fields of psychology and neurology via his Project for Scientific Psychology, with the goal of establishing a new science called neuroscientific psychology. It is essential to thoroughly analyses psychology's primary theoretical views and disputes, taking into account their historical origins and current significance [41].
Cieri & Esposito (2019) explore the historical development of psychology from the 1880s onward, revealing a parallel underlying framework. Freud proposed an inherently interconnected relationship between psychology and physiology, as the physiology of the brain fundamentally underpins mental well-being. Nevertheless, he gradually acknowledged the constraints of technology and the need to priorities psychoanalysis as a more appropriate therapeutic approach, given his inability to pursue his grandiose goals in neuroscience. During his time, Freud was skeptical of the phrenology tendency, which aimed to pinpoint psychological functions in particular neuroanatomical locations [33].
Although there is doubt about it, progress in neuroscience, namely in neuroimaging, has enabled a productive exchange between neuroscience and psychoanalysis, providing fresh insights into the relationship between the mind and brain as well as psychoanalytical hypotheses. The combination of advancements in neural network research and the use of the free energy concept has significantly accelerated the development of psychodynamic neuroscience. The advancement in understanding the Default Mode Network and its complex connection with the notion of self is especially apparent. The paper provides a concise overview of significant advancements in the field of psychodynamic neuroscience, with a particular focus on the connection between psychoanalysis and neuroscience. Wilfred Ruprecht Bion, a psychotherapist, established the notion of alpha function, which this book also aims to address, proposing its deeper integration with neuroscience. Hammond (2019) underlines Ludwig von Bertalanffy's general system theory as a fundamental framework for comprehending these intricate relationships.
Exploring Mental Health and Human Behaviour
According to Sinnott-Armstrong & Summers (2020), various mental health issues may be influenced by biological factors such as heredity and neurochemistry. On the other hand, psychological variables such as cognitive processes and emotional control may worsen or improve these situations. Furthermore, mental health outcomes are substantially impacted by social variables such as family dynamics, cultural influences, and socioeconomic position [28]. The researchers argue for a deep understanding of ideas that recognise the complex interplay of biological, psychological, and social elements rather than oversimplifying these phenomena. This knowledge empowers us to comprehend and tackle mental health difficulties, especially in their application. Additionally, they suggest further refining these ideas to enhance our comprehension of the mind and learning processes, further empowering us in our pursuit of mental health understanding. Sleep, as Sinnott-Armstrong & Summers (2020) suggest, is not just a restful state, but a pivotal element in neurological development. It plays a fundamental role in shaping the structure and function of the brain. From a developmental psychology perspective, sleep is not just a time of rest, but a crucial period in enhancing learning, regulating emotions, and promoting cognitive development in babies, children, and adolescents. The synaptic pruning theory proposes that the brain optimises neural circuits for effective information processing and storage by systematically removing superfluous neuronal connections during sleep. The brain's glymphatic system, most active during sleep, aids in the removal of metabolic waste products, supporting the health and integrity of neural tissue. Psychodynamic theories highlight the role of sleep in emotional regulation, suggesting that dreams serve as a method for assimilating everyday events and resolving internal conflicts, crucial for psychosocial development. These intriguing aspects of sleep in neurological development and emotional regulation pique our curiosity and urge us to delve deeper into this fascinating field.
In addition, cognitive theories highlight the significance of sleep in memory consolidation. These theories suggest that newly learned information is reactivated and reorganised during sleep, leading to improved learning and problem-solving skills. Together, these ideas provide light on the complex relationship between sleep and brain development, highlighting its essential role in moulding the course of human cognition, emotion, and behavior from infancy to maturity. However, an alarming trend is the increasing number of individuals suffering from sleep deprivation, which is not just a minor inconvenience, but a serious threat to their overall health and happiness.
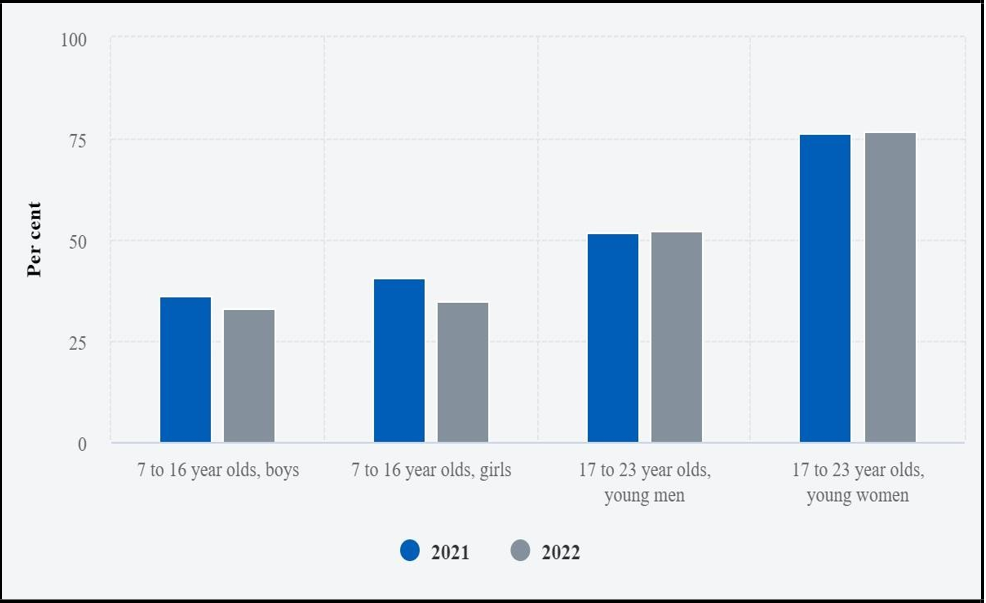
Figure 1: [36] Depicts the prevalence of sleep deprivation among individuals aged 7 to 23 in the United Kingdom, serving as a stark reminder of the urgent need to address this issue for the sake of our collective well-being.
Figure 1: Note: Adapted from the National Institute of Health
Pinel & Barnes (2021) state that neuroscience has not yet developed a comprehensive theory that explains the functioning of the human brain and mind. Psychoanalysis has had difficulties establishing a biological foundation for its theoretical frameworks, emphasising the contrasting methodologies and instruments used by both disciplines. Freud's original goal was to clarify the neurophysiological mechanisms that underlie psychic processes. However, he encountered obstacles due to technical constraints and cynicism regarding the idea of localizationism [32]. His notion of expansive cerebral networks anticipated contemporary neural network theories in opposition to reductionism. Likewise, he stressed that the involvement of the body in cognitive processes suggests an ongoing interplay between physical sensations, emotions, and cognition. The technique utilises a comprehensive and holistic method to comprehend the intricacies of the mind-brain system in accordance with principles derived from General Systems Theory [32].
Structuralism has lost popularity since it relies on subjective introspection and lacks empirical validity. However, functionalism has provided the foundation for modern techniques like evolutionary psychology and cognitive neuroscience. The ongoing discussion on the relationship between the organisation and purpose of mental processes continues to be significant in contemporary psychology. Researchers are actively working to combine both viewpoints in order to better comprehend the intricate nature of human cognition and behaviour.
However, there is an ongoing dispute over the merits of behaviourism compared to psychoanalysis [9]. Prominent personalities like John B. Watson and B.F. Skinner led behaviourism in the early 20th century, while Sigmund Freud pioneered psychoanalysis. Behaviourism dismissed the examination of subjective mental processes and instead emphasised only observable behaviour and environmental variables. On the other hand, psychoanalysis explores the profound aspects of the unconscious mind, emphasising the significance of early childhood experiences and hidden conflicts in influencing an individual's personality and behaviour. Although behaviourism was the dominant force in American psychology for a significant portion of the 20th century, its impact has diminished as cognitive psychology and neuroscience have gained prominence.
Despite facing criticism for its lack of factual evidence and focus on subjective interpretation, psychoanalytic theory continues to have a significant impact on clinical practice and psychotherapy. The continuous discourse between behaviourism and psychoanalysis has broadened to include a more complete investigation of how cognition, biology, and culture influence human behaviour. The ongoing discourse on the interplay between genetics (nature) and environment (nurture) in shaping human development and conduct has been a prominent topic in psychology since its origin. Early scholars like Francis Galton and Charles Darwin underlined the significance of genetics in producing individual variations, but environmentalists like John Locke and B.F. Skinner underscored the importance of learning and environmental factors. The argument's focus has now shifted to understanding the interplay between genes and the environment, epigenetic mechanisms, and the ever-changing nature of developmental processes. [27] Philip & Cherian (2020) state that modern viewpoints, such as the biopsychosocial model, recognise the many variables that affect human conduct, including genetics, biology, psychology, and social effects.
In the cognitive revolution of the 1950s and 1960s, there was a focus on the connection between cognitive psychology and neuroscience. This led to a challenge to behaviourism's dominating emphasis on externally visible activities. This movement emphasised the significance of exploring cognitive processes such as perception, memory, language, and problem-solving. Concurrently, advancements in neuroscience provide insight into the molecular basis of cognition. Donald Hebb and Eric Kandel played a crucial role in explaining the brain processes that govern learning and memory [22].
Cognitive psychology and neuroscience have become the prevailing frameworks in modern psychology, with researchers using various methods to study the intricacies of the connection between the mind and the brain.
Cognitive neuroscience combines the study of cognitive psychology with neuroscientific methods. Magnetic Resonance Imaging (MRI) has examined the complex mechanisms of sleep and awakening in the human brain. During sleep, MRI studies have observed certain brain activity patterns characterised by synchronised neuronal oscillations and decreased metabolic activity in some areas. These patterns indicate the important restorative processes that are essential for memory consolidation and cognitive functioning. Conversely, MRI scans reveal heightened activity in specific brain regions associated with focus, decision-making, and sensory experiences during awake periods. This demonstrates how the brain actively interacts with the outside world. The use of MRI reveals the intricate relationship between sleep and awakening, which involves complex interactions across brain circuits and chemical signals. This interplay is crucial for sustaining optimum cognitive and physiological well-being.
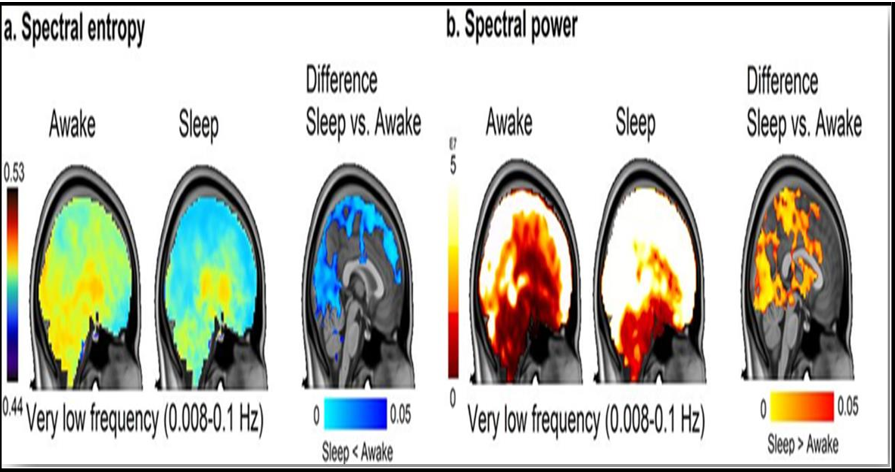
Figure 2: [23] Displays functional magnetic resonance imaging (fMRI) scans taken during both sleep and wakefulness.
Figure 2: Note: Adopted from [18]. Gosseries O, Laureys S, Schnakers C (2019). Between Theory and Clinic: The Contribution of Neuroimaging in the Field of Consciousness Disorders. Frontiers Media SA.
Consistent patterns arise throughout periods of sleep and awakeness, indicating differences in brain activity. During periods of awakeness, functional magnetic resonance imaging (fMRI) scans show increased activity in several areas of the brain that are important for processing sensory information, coordinating movement, and carrying out cognitive tasks. The prefrontal cortex, which is responsible for decision-making and attention, often shows elevated blood flow and oxygenation, suggesting heightened neuronal activity. Similarly, areas linked to sensory perception, such as the visual, auditory, and somatosensory cortices, may exhibit increased activity during sleep as they handle incoming sensory information.
In contrast, fMRI pictures obtained during sleep show significant variations, indicating alterations in brain activity that are specific to the various sleep phases. During non-REM sleep, fMRI scans usually show lower brain activity relative to when a person is awake. The cortical regions of the brain, responsible for conscious awareness and higher-level cognitive functions, exhibit this drop in activity. Nevertheless, key brain regions responsible for crucial activities like memory consolidation, such as the hippocampus and particular cortical areas, may still display activity during non-REM sleep, albeit at a reduced level.
Functional magnetic resonance imaging (fMRI) scans show a clear pattern during rapid eye movement (REM) sleep. This pattern is marked by increased neural activity in areas related to controlling emotions, improving memories, and visualising mental images. Structures such as the amygdala and hippocampus in the limbic system often exhibit increased activity during REM sleep, indicating the brain's involvement in processing emotional events and strengthening memories. In addition, the visual association regions may also show heightened activity, which corresponds to the vivid dream imagery that occurs during this period of sleep.
The integration of cognitive and neurological views has greatly enhanced our comprehension of the connections between the brain and behaviour, the consolidation of memory, processes related to attention, and mental diseases [20]. Schwartz & Kilduff (2015) [33] examine the process of reflecting on the primary theoretical views and disputes in the field of psychology. The field is characterised by a diverse range of ideas, approaches, and debates. Historical disagreements have influenced the direction of psychological research. However, modern psychology now adopts a pluralistic approach that combines several viewpoints and approaches to tackle intricate problems about the mind, brain, and behaviour. Psychologists have the task of carefully assessing theoretical frameworks, collaborating across different disciplines, and being aware of the many sociocultural settings that impact human cognition and behaviour as the profession continues to develop.
Schwartz & Kilduff (2015) emphasise that sleep may fulfil a homeostatic function. Despite thorough investigation, the precise function of sleep remains obscure, giving rise to various significant hypotheses, such as the ideas of inactivity, energy conservation, restoration, and brain plasticity. The inactivity hypothesis proposes that during evolution, individuals tended to engage in less activity at night to reduce their vulnerability to predators. The concept of energy conservation posits that sleep reduces the amount of energy required for foraging during less efficient times. The restoration hypothesis posits that sleep plays a crucial role in promoting cellular repair and replenishment. The hypothesis of brain plasticity posits that sleep plays a critical role in the reorganisation of neuronal connections and the development of the brain. These ideas are not comprehensive, indicating that it may be crucial to integrate them in order to comprehend sleep [17].
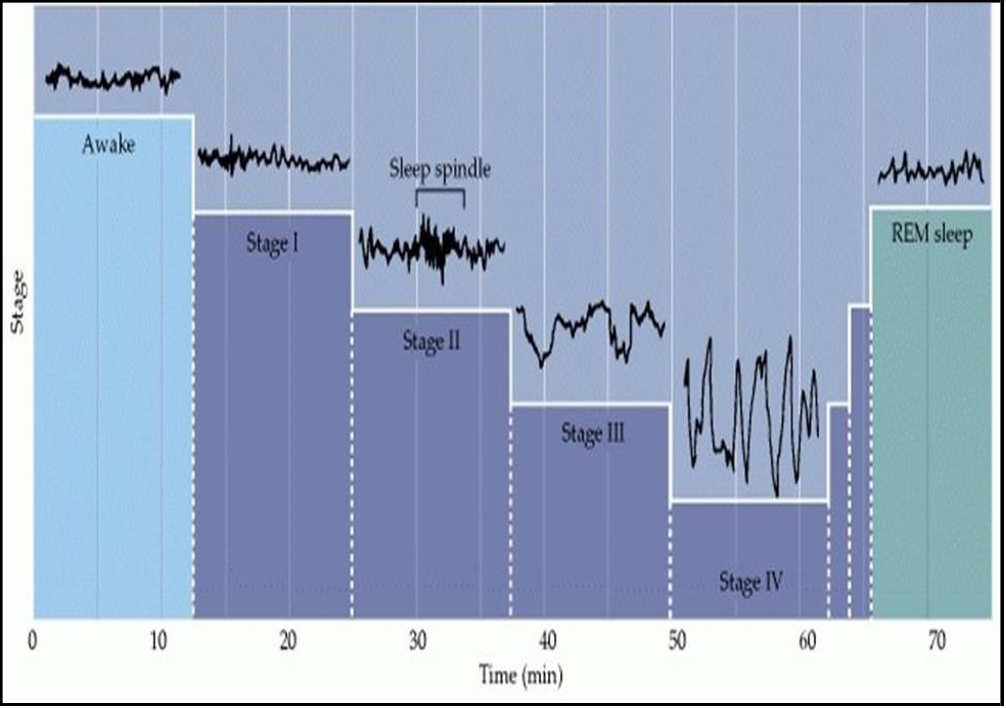
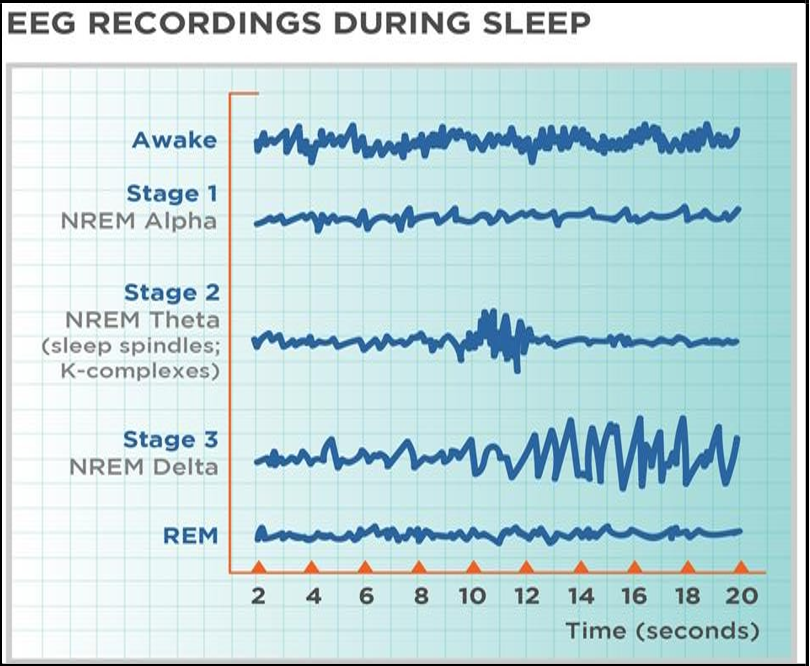
Figure 3 Note: Adopted from Neuroscience. 2nd edition. Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Sunderland (MA): Sinauer Associates; 2001 Displays an EEG that illustrates different sleep stages.
Polysomnography is the main method used to investigate sleep, which involves the use of many parameters such as EEG, EOG, EMG, and oxygen saturation. Sleep is a crucial physiological activity that has long fascinated scientists because of its significant influence on cognitive performance, emotional control, and general well-being. Sleep, an essential element of human biology, continues to be a topic of significant interest and investigation in several scientific fields, especially in the field of biopsychology[39]. The integration of psychological and biological approaches or measurements in biopsychological research has enhanced our understanding of the sleep phenomena. This study examines the complex connection between biopsychology and sleep, specifically focusing on how recent research has shed light on the neurological basis of sleep using modern methods like fMRI, tDCS, and EEG [23].
EEG has yielded useful insights into the rhythmic patterns of brain activity during sleep, differentiating between REM sleep and NREM sleep (He et al., 2021). Synchronized slow-wave oscillations, indicative of deep sleep and restorative activities, distinguish NREM sleep. On the other hand, REM sleep has unsynchronized brain activity that is similar to being awake, which promotes dreaming and memory storage.
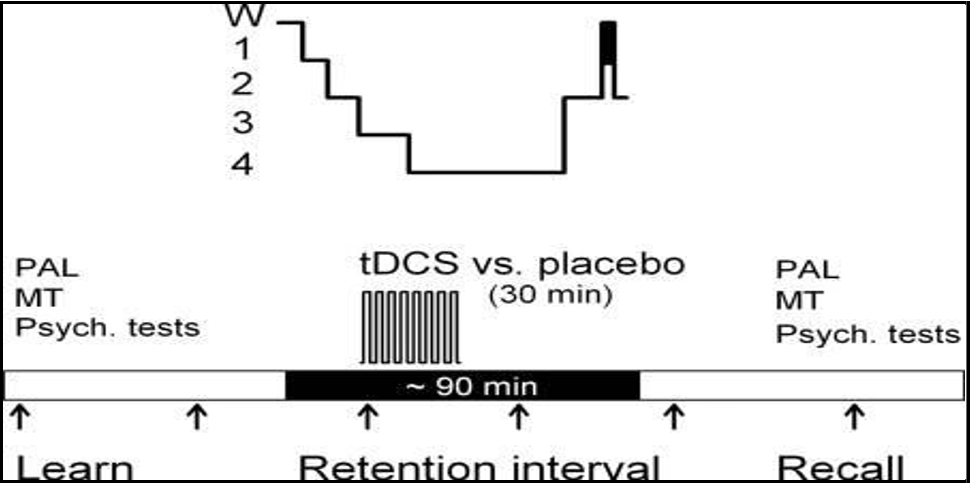
Thair et al. (2017)describe transcranial direct current stimulation (tDCS) as a non-invasive method for controlling brain activity in specific regions. It provides a reversible way to affect different cognitive, physical, social, and emotional processes. In sleep trials with tDCS, scientists often apply electrical currents to particular areas of the brain before or during certain sleep phases, such as slow-wave sleep (SWS) or rapid eye movement (REM) sleep.
The results of these investigations might fluctuate based on variables such as the stimulation settings (e.g., strength, duration), electrode location, and individual variations among participants.
Research indicates that the use of transcranial direct current stimulation (tDCS) during sleep has the potential to improve certain cognitive functions and boost the process of memory consolidation. For instance, some studies have linked enhancements in memory performance and learning tasks to the application of transcranial direct current stimulation (tDCS) to the prefrontal cortex or hippocampus during sleep. Researchers have investigated the potential therapeutic benefits of using transcranial direct current stimulation (tDCS) during sleep to treat illnesses like insomnia, depression, and other sleep disorders.
Figure 4: [40] Depicts the DCS outcome obtained during the sleep experiment.
Figure 4: Note: Adoped from Thair et al., 2017
Neuromodulation methods, including tDCS, have provided new opportunities for studying the causal influence of certain brain areas on sleep regulation and cognitive performance. It has shown the capacity to augment learning, boost task performance, and alter behaviour in people who are in good health. The use of tDCS may transiently modify neuronal excitability. The device's user-friendly interface, cost-effectiveness, and capacity for home management make it attractive for therapeutic applications, such as facilitating rehabilitation and improving cognitive and motor skills.
Furthermore, transcranial direct current stimulation (tDCS) has potential for mitigating symptoms of depression, diminishing hallucinations in schizophrenia, and enhancing language learning in individuals with autism spectrum disorder. While further study is required to completely confirm its clinical uses, tDCS has great potential as a tool for both neuroscientific exploration and therapeutic intervention. tDCS, or transcranial direct current stimulation, may modify the excitability of certain regions of the brain by administering weak electrical currents. This can have an impact on sleep characteristics and potentially provide therapeutic treatments for sleep-related problems.
Sleep is a crucial aspect that has received much focus in the fields of biopsychology and emotional processing [39]. Research using functional magnetic resonance imaging (fMRI) has uncovered brain circuits that play a role in the formation of dreams and the emotional response during rapid eye movement (REM) sleep. This research sheds light on the integration of emotional experiences into long-term memory storage. In addition, EEG research has shown that REM sleep is important for synaptic plasticity and the consolidation of memory. These studies have pinpointed specific oscillatory patterns, like theta and gamma oscillations, present in hippocampus-dependent memories. The interaction between REM sleep and the processing of emotional memory has significant consequences for comprehending the causes and management of mood disorders and trauma-related diseases [34].
Biopsychology's empirical research has expanded our understanding of the brain factors linked to sleep and how medications can affect them. Neuropharmacological methods that focus on specific neurotransmitter pathways, such as serotonin, dopamine, and GABA, have shown potential for regulating sleep parameters and improving sleep quality in patients with sleep disorders. Researchers who looked into how hypnotic drugs affect sleep and the brain pathways linked to insomnia found that networks of neurotransmitters and the control of sleep-wake cycles interact in complex ways.
This study examines the impact of recent studies on our comprehension of sleep patterns, as well as the brain areas responsible for regulating wakefulness and sleep. It also discusses the potential consequences for health and illness. To understand the intricacies of sleep, we analyze the combination of biological and psychological viewpoints, emphasizing the need for interdisciplinary methods to improve the field of sleep research.
Sleep architecture refers to the organization and structure of different sleep stages that occur throughout a typical sleep cycle.
Sleep architecture refers to the process of mapping and organising the many phases of sleep, which include transitions between waking, REM sleep, and NREM sleep. Changes in sleep structure may disrupt the equilibrium of different sleep phases and lead to the development of sleep disorders. Biopsychological studies have clarified the several stages of sleep, characterised by distinct brain activity patterns and physiological changes. The integration of psychological and biological approaches in biopsychological research has greatly enhanced our understanding of the brain systems that govern sleep. Scientists have investigated the connection between biopsychology and sleep by using advanced techniques like functional magnetic resonance imaging (fMRI), electroencephalography (EEG), and transcranial direct-current stimulation (tDCS). These methods have helped shed light on the brain mechanisms involved in sleep.
Biopsychological research has been crucial in elucidating the neurological underpinnings of sleep architecture and the regulatory mechanisms that control sleep-wake cycles. Functional neuroimaging methods, such as fMRI, allow researchers to observe variations in brain activity throughout various sleep phases. This helps show the dynamic patterns of neural activation and connectivity in important brain areas involved in regulating sleep [23]. In addition, [2]Antelmi et al. (2019) conducted EEG investigations that revealed synaptic plasticity and memory consolidation. These studies identified certain oscillatory patterns, such as theta and gamma oscillations, that were shown to be involved in the reactivation and consolidation processes. of hippocampal-dependent memories.
Figure 5, Shows EEG Recordings During Sleep.
Figure 5- Note: https://s3-us-west-2.amazonaws.com/courses-images/wp content/uploads/sites/855/2015/02/26123807/EEG-Graphic-1.jpg
EEG has yielded useful insights into the rhythmic patterns of brain activity during sleep, differentiating between rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. Coordinated slow-wave oscillations distinguish NREM sleep, indicating profound slumber and healing mechanisms. Research using functional magnetic resonance imaging (fMRI) has discovered brain circuits associated with the formation of dreams and the emotional response during rapid eye movement (REM) sleep. This research provides insight into the processes involved in integrating emotional events into long-term memory storage. The interaction between REM sleep and emotional memory processing has significant implications for understanding the causes and management of mood disorders and trauma-related diseases.
Biopsychology's empirical research has shed light on the brain factors linked to sleep and their potential drug influence. Scientists have discovered intricate connections between neurotransmitter systems and the regulation of sleep and wakefulness. Neuropharmacological methods that focus on specific neurotransmitter pathways, such as serotonin, dopamine, and GABA, have shown potential for regulating sleep parameters and improving sleep quality in patients with sleep disorders.
Biopsychological research has greatly enhanced our understanding of the neurological systems that underlie sleep. Scientists have combined psychological and scientific techniques to better understand the intricate details of sleep patterns, the influence of neurotransmitters, and the specific brain areas responsible for regulating sleep [14]. The findings from this study have significant implications for the diagnosis, treatment, and prevention of sleep- related illnesses, emphasizing the critical role of multidisciplinary methods in the field of sleep science. Advancements in biopsychological research will continue to improve our knowledge of the neurological basis of sleep. This progress will also facilitate the development of new treatment approaches to boost sleep quality and overall well-being.
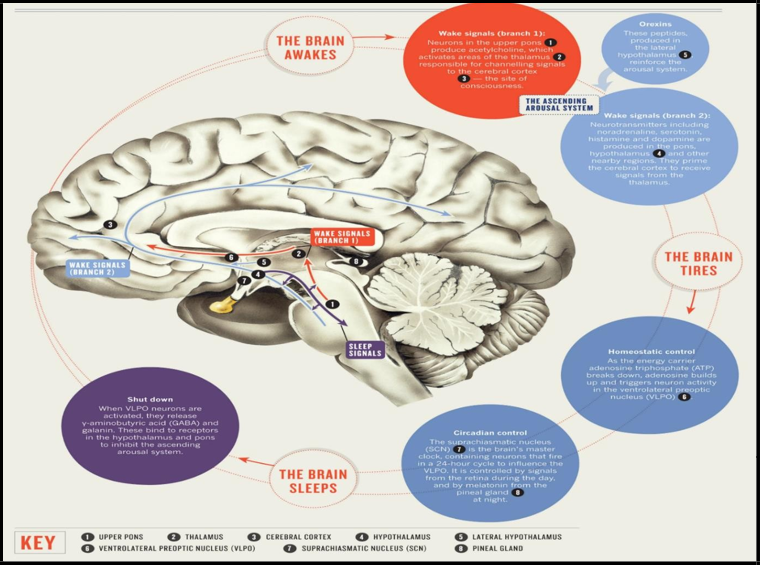
Brain regions responsible for sleep regulation include the hypothalamus, which plays a crucial role in controlling sleep patterns.
The hypothalamus serves as the primary control center for sleep regulation. It contains important structures such as the suprachiasmatic nucleus (SCN) and ventrolateral preoptic nucleus (VLPO), which work together to regulate circadian rhythms and sleep-wake cycles, respectively. The hypothalamus, located inside the intricate network of neural connections in the brain, serves as a vital centre for regulating sleep [37]. Key regulators called SCN and VLPO control the complicated process of going from sleep to alertness. This process takes place in a system of nuclei and neuronal populations.
The suprachiasmatic nucleus (SCN) is a small region located in the brain.
The suprachiasmatic nucleus (SCN) serves as the primary circadian pacemaker inside the hypothalamus. Located in the anterior hypothalamus, this compact group of neurons beats in sync with the sun, regulating our internal circadian rhythms. As the amount of sunshine decreases, specialised cells in the eye called retinal ganglion cells send signals to the suprachiasmatic nucleus (SCN) via a pathway called the retinohypothalamic tract. In this situation, the suprachiasmatic nucleus (SCN) interprets the changing light of neural signals and makes sure that our internal biological cycles are in sync with the rhythm of the outside world. The suprachiasmatic nucleus (SCN) orchestrates the interaction between sleep and awakeness by establishing intricate connections with the pineal gland and other brain areas. It regulates melatonin production and guides us through the sleep process throughout the night. However, shift work, jet lag, or the intense brightness of artificial light can disturb the precise equilibrium of circadian rhythms, weakening the SCN and leading to sleep problems [4].
The Ventrolateral Preoptic Nucleus (VLPO)
Delving deeper into the hypothalamus, we encounter the ventrolateral preoptic nucleus (VLPO), a peaceful sanctuary amidst the tumultuous wakefulness associated with dreams. Here, in the middle of the communication between GABAergic neurons, the process of transitioning from being awake to falling asleep occurs smoothly and elegantly. When night comes, the ventrolateral preoptic nucleus (VLPO) has a hypnotic effect on the brainstem and basal forebrain that are in charge of keeping you awake, which makes you feel calm. With each inhalation and pulsation of the heart, the state of being awake gradually dissipates, allowing the entrance to the domain of dreams to unfold. Inside the VLPO, inhibitory projections move in a coordinated manner, creating a pattern of synchronised neurons that leads to the start of sleep. GABAergic neurotransmission induces a state of tranquility, reducing the distinction between awareness and unconsciousness and initiating the process of entering deep sleep.
However, beneath the quietness of the VLPO, there is the presence of insomnia, a mysterious entity that haunts the realm of slumber. The VLPO (ventrolateral preoptic nucleus) has trouble keeping wakefulness under control when stress, anxiety, or neurochemical imbalances upset the delicate balance of inhibitory signalling. As a result, individuals experience insomnia and restlessness [11].
The Hypothalamic Odyssey
As we explore the intricate network of the hypothalamus, we come into contact with the complex challenges of sleep disorders. These disruptive forces pose a significant risk to our ability to achieve restful sleep. Within the realm of sleep disorders, the intricate nature of regulating sleep and wakefulness becomes apparent in the presence of insomnia and hypersomnia. The VLPO serves as a source of hope in the middle of insomnia, providing a refuge for troubled individuals who are unable to sleep [13]. However, when we hinder the natural process of falling asleep and the inhibitory effects of GABA are ineffective, it becomes difficult to achieve a peaceful sleep.
In contrast, in hypersomnia, the suprachiasmatic nucleus (SCN) serves as a prominent source of guidance amongst the darkness—a signal of circadian rhythm coordination in a world overwhelmed by excessive drowsiness. However, when disruptions disrupt the fragile equilibrium of internal circadian rhythms and disrupt the regular patterns of day and night, the experience of being awake becomes fraught with danger. As we near the end of our exploration of the hypothalamus, we gain a deep understanding and admiration for the complex patterns of neuronal activity that control sleep and awakeness. The SCN is the master circadian pacemaker, and the VLPO is the calm sanctuary. Each nucleus and neuronal population plays a key role in coordinating the control of sleep-wake cycles [39]. However, within the exquisite scenery of the hypothalamic landscape, there is a presence of sleep disorders—a stark reminder of the vulnerability of the intricate equilibrium that regulates our nocturnal journey. To effectively manage insomnia and hypersomnia, it is crucial to understand and follow the patterns of sleep and wakefulness dictated by the hypothalamus, as emphasised by Song et al. (2021). The continuous interplay between the states of sleep and alertness forms the fundamental essence of our vitality, well-being, and basic life. Our hypothalamus guides us as we fall asleep, reminding us that during sleep, we experience rejuvenation, recovery, and the hope of a fresh start.
Thalamic and cortical networks
Thalamocortical circuits facilitate the processing of sensory information and the state of consciousness when awake and experience dynamic alterations during sleep. During non-rapid eye movement (NREM) sleep, the thalamic relay nuclei display rhythmic activity patterns. In contrast, during rapid eye movement (REM) sleep, cortical areas are involved in memory consolidation and synaptic pruning. Thalamocortical circuits have a crucial role in sensory processing, awareness, and cognitive activities within the complex structure of the brain [21]. The circuits formed by connecting pathways between the thalamus and cortex have a crucial function in facilitating sensory perception, integrating incoming information, and coordinating neuronal activity across different parts of the brain. The thalamocortical circuits have a crucial and ever- changing function in controlling sensory processing and awareness when a person is awake. The transformational changes that occur during sleep influence sleep patterns, impacting memory consolidation and synaptic pruning.
Thalamocortical networks serve as portals to both awareness and sensory processing. Thalamocortical circuits provide an intricate network of connections between the thalamus and cortex, allowing for two-way communication and information exchange between sensory modalities and more advanced parts of the brain. These circuits regulate and integrate sensory perception, attention, and cognitive activities, influencing our conscious experience of the world. The thalamocortical circuits serve as the primary pathways, transporting sensory information from peripheral receptors to the neocortex for fusion and analysis. The thalamus contains sensory relay centres such as the lateral geniculate nucleus (LGN) for vision, the medial geniculate nucleus (MGN) for hearing, and the ventral posterior nucleus (VPN) for somatic sensations. These centres receive signals from peripheral sensory organs and send them to the corresponding sensory cortices. Specialised sections within the cortex, such as the primary visual cortex (V1), primary auditory cortex (A1), and primary somatosensory cortex (S1), analyse and interpret sensory input to help create perceptual events. Thalamocortical networks are essential for controlling consciousness by combining sensory input, sustaining cortical alertness, and facilitating advanced cognitive processes.
The thalamus acts as a central hub, sorting and giving priority to sensory inputs depending on their importance and relevance to current cognitive processes. Cortical feedback loops between sensory regions and association areas improve sensory information processing and understanding, allowing for flexible attention and conscious awareness. During sleep, the thalamocortical circuits experience dynamic modifications in their activity and connectivity, which indicate the shifts between various sleep phases and the resulting changes in brain processing and cognitive performance. The thalamus, hypothalamus, and brainstem have essential functions in coordinating various sleep phases throughout the sleep cycle. The primary function of the cerebral cortex is to regulate the flow of information, whereas the hypothalamus governs the state of wakefulness and sleep by releasing neurotransmitters such as orexin and hypocretin, which promote alertness, and melatonin, which promotes sleep. In addition, the brainstem has nuclei that are important for controlling both REM and non-REM sleep periods.
On the other hand, the process of transitioning to wakefulness is characterised by the activation of the ascending reticular activating system (ARAS). This system delivers stimulating impulses to the thalamus and brain, which in turn promote arousal and conscious awareness. Acetylcholine, serotonin, norepinephrine, and dopamine play a crucial role in sustaining sleep by regulating brain activity and increasing attentiveness. In summary, the intricate equilibrium between neural circuits that promote sleep and those that promote alertness in the central nervous system is responsible for the cyclical nature of sleep and wakefulness. This ensures that the brain functions optimally and behaves appropriately throughout the day.
Figure 6 Depicts the structure and components of the sleep process.
Figure 6: Note: Adopted from [26] Peplow, M. (2013). Structure: The anatomy of sleep. Nature, 497(7450), S2–S3.
https://doi.org/10.1038/497s2a
The thalamocortical circuits show rhythmic activity patterns during non-rapid eye movement (NREM) sleep. These patterns are made up of synchronised slow-wave oscillations (<1 Hz) and spindle oscillations (8–14 Hz). Some thalamic nuclei, like the thalamic reticular nucleus (TRN) and others, have higher rhythmicity and synchronisation, which means that the brain is less active and processing sensory information.
The hippocampus and prefrontal cortex, which are cortical areas involved in memory consolidation, exhibit slow-wave activity and replay of neuronal firing patterns. This process facilitates the offline processing of recent events and the integration of new memories. During REM sleep, there are significant alterations in the activity of thalamocortical circuits, characterized by unsynchronized cortical activity and increased involvement of the limbic system. The thalamic relay nuclei have slower rhythmicity and tonic firing rates, but the amygdala and hippocampus, which are in the cortex and are involved in memory consolidation and emotional processing, are more active. Intense dreaming and increased limbic system activity distinguish REM sleep, signifying the merging of emotional memories and the adjustment of memory pathways. It is during sleep that the thalamocortical circuits go through dynamic changes that help with things like memory consolidation, synaptic plasticity, and keeping cognitive function [13].
During NREM sleep, thalamocortical oscillations and slow-wave activity strengthen declarative and procedural memories, facilitating the transfer of information from short-term to long-term storage. During slow-wave sleep, there is a reoccurrence of the firing patterns of neurons in the cortex. This process helps reactivate memories and strengthen the connections between synapses, which in turn aid in the encoding and retrieval of learned information. REM sleep triggers heightened synaptic pruning and structural remodelling in thalamocortical circuits, thereby enhancing brain connectivity and eliminating superfluous or unwanted synaptic connections during synaptic pruning.
Selective elimination of synapses during REM sleep may enhance the efficiency of information processing and the dynamics of brain networks. This process promotes cognitive flexibility and adaptive behaviour.
The study into the function of thalamocortical connections has important implications for understanding the underlying causes of sleep problems and developing new and effective treatments. Thalamocortical dynamics disruption has been associated with many sleep disorders, including insomnia, narcolepsy, and REM sleep behaviour disorder. Studying the brain processes that cause sleep disorders might help us develop specific therapies to improve the function of the thalamocortical system and encourage healthy sleep patterns. Pharmacological and neuromodulator methods that focus on thalamocortical circuits show potential for treating sleep problems and cognitive impairments.
According to Song et al. (2021), non-invasive brain stimulation techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) might change the activity of the thalamocortical network, which could lead to better sleep quality and cognitive performance.
Thalamocortical circuits are crucial for sensory processing, awareness, and cognitive function while we are awake. However, during sleep, these circuits undergo alterations that help enhance memory and improve synaptic connections. Comprehending the complex interactions of thalamocortical circuits during sleep provides valuable knowledge about the brain processes that govern cognitive performance and the control of sleep-wake cycles. This knowledge may lead to the development of novel strategies for addressing sleep disorders and improving cognitive abilities. Through our exploration of thalamocortical interactions, we gain insight into the intricate relationship between different areas of the brain and their influence on our conscious perception of the surrounding world.
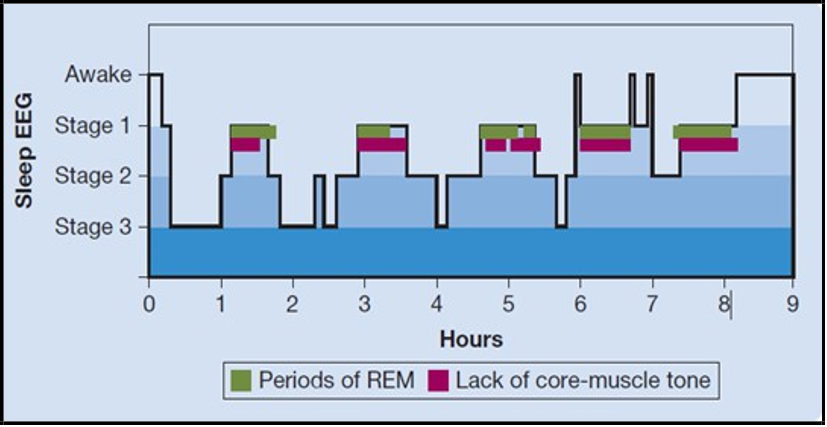
Stages of Sleep
Figure 7: Note: Adopted from Pinel & Barnes (2021).
People often categorize the sleep phenomenon into two main states: REM sleep and NREM sleep. We subdivide NREM sleep into three stages: N1, N2, and N3, each exhibiting unique patterns of brain activity and physiological alterations. The progression through the different phases of sleep starts with non-rapid eye movement (NREM) sleep. N1, sometimes referred to as the first stage of sleep, signifies the shift from being awake to entering a state of sleep. During this phase, the frequency of brain waves lowers and the level of muscular tension reduces, facilitating the process of falling asleep. Research in biopsychology using electroencephalography (EEG) has discovered distinct theta waves during N1 sleep, which indicate a state of tiredness and relaxation. Figure 7 depicts the many stages of sleep.
During the progression of sleep, people transition into N2 sleep, which makes up the majority of a regular night's sleep. N2 sleep is characterised by the presence of sleep spindles and K-complexes in EEG recordings. The process of memory consolidation and sensory gating describes episodes of neuronal activity. Research in the field of biopsychosocial studies has clarified the function of neurotransmitters like acetylcholine and serotonin in regulating sleep spindles and K complexes. This emphasises the interaction between biological variables and cognitive processes that occur during sleep. Also, studies using brain imaging techniques like functional magnetic resonance imaging (fMRI) have shown that areas of the brain that make you alert, like the prefrontal cortex, are less active, while areas that make you sleepy, like the thalamus and hypothalamus, are more active [16]. The most profound phase of NREM sleep is N3, which is often referred to as slow-wave sleep (SWS) or deep sleep. Large delta waves on EEG recordings distinguish SWS, indicating coordinated neuronal activity and rejuvenating processes [13]. During N3 sleep, the body experiences physiological alterations such as muscle regeneration, hormone secretion, and immune system upkeep. Biopsychological research has shown a connection between slow- wave sleep (SWS) and the processes of memory consolidation, emotional regulation, and total physical rejuvenation. This highlights the crucial role of deep sleep in cognitive and physiological performance.
NREM sleep cycles intertwine with REM sleep, also known as paradoxical sleep. This is because it closely resembles alertness, despite having significant physiological distinctions. Research in the field of biopsychosocial science has emphasized the role of several neurotransmitter systems, including acetylcholine, serotonin, and noradrenaline, in REM sleep regulation and the creation of dreams [28]. Malfunction in these neurotransmitter systems can lead to sleep disorders such as REM sleep behaviour disorder (RBD) and nightmares.
The biopsychosocial approach to comprehending the phases of sleep highlights the complex interaction of biological, psychological, and social elements that affect the structure and quality of sleep.
Biological factors refer to the neurobiological processes that control sleep, such as specific areas of the brain, neurotransmitter systems, and hereditary tendencies. Brain activity during sleep regulates cognitive processes such as memory consolidation, emotional control, and dream content, which are known as psychological variables. Social variables refer to the many impacts of the environment, cultural norms, and socioeconomic factors that shape sleep patterns and behaviours in different populations.
Research using biopsychosocial methods has yielded useful knowledge about the many phases of sleep and how they affect our health and well-being. Research examining the neurological connections of sleep using brain imaging methods has shown certain areas and networks in the brain that play a role in regulating sleep- wake cycles, consolidating memories, and processing emotions [13]. Behavioural research has investigated the effects of sleep deprivation and sleep disorders on cognitive performance, emotional stability, and social functioning. Epidemiological studies have investigated the impact of sociodemographic characteristics, including age, gender, employment, and socioeconomic level, on sleep habits.
The stages of sleep include a complex interaction between biological, psychological, and social elements, all of which contribute to the control and preservation of normal sleep patterns. Scientists have comprehensively understood the intricacies of sleep structure and its impact on cognitive, emotional, and physical abilities. By incorporating knowledge from neuroscience, psychology, and sociology, we may enhance our understanding of sleep as a key element of human biology and behaviour. This, in turn, enables us to develop creative methods for conducting sleep research and improving clinical practice.
Electrophysiological recordings, such as electroencephalography (EEG), have shown the fluctuating alterations in brain wave activity that occur during sleep. Slow-wave activity (SWA), a sign of deep sleep and therapeutic mechanisms, is associated with NREM sleep. Conversely, unsynchronized brain activity, akin to awake, distinguishes REM sleep and aids in dreaming and memory consolidation. The complex interaction between brain waves and sleep stages is essential to human physiology and psychology. Sleep is a multifaceted phenomenon that goes beyond just resting. It is a dynamic process that encompasses many phases and involves diverse brain activity. The interaction between brain waves during sleep has a significant effect on cognitive processes, emotional control, and general well-being.
Neurons classify brain waves, the synchronised electrical patterns they generate, into several frequencies, each associated with specific mental states and activities. The main categories of brain waves consist of delta, theta, alpha, beta, and gamma waves. Delta waves, which have frequencies between 0.5 and 4 Hz, are most noticeable during periods of deep sleep, especially during slow-wave sleep (SWS) [17]. Therapeutic procedures, including physical health restoration, immune system enhancement, and memory consolidation, are associated with them. Delta activity indicates the brain's capacity to disengage from external stimuli and concentrate on internal processes of rejuvenation and repair.
The first phases of sleep and REM (rapid eye movement) sleep are when we most frequently see theta waves, which have frequencies ranging from 4 to 8 Hz. They have a vital function in the development of creativity, intuition, and emotional processing. Theta oscillations are associated with the consolidation of experiences, modulation of emotions, and encoding of memories. A person in a state of calm alertness or light slumber may detect alpha waves, which have a frequency range of 8 to 12 Hz. They represent a condition of alert relaxation, often linked with a serene and contemplative frame of mind. Alpha activity encompasses techniques that promote relaxation, enhance focus, and encourage reflective thinking. Active wakefulness and heightened cognitive activity most often reveal beta waves, which have frequencies between 12 and 30 Hz. They exhibit qualities such as vigilance, concentration, and analytical reasoning skills. Beta activity is critical for problem-solving, decision-making, and goal-oriented behavior. Advanced cognitive abilities and information processing are associated with gamma waves, oscillating at frequencies above 30 Hz. They contribute to the processes of perception, awareness, and the synthesis of sensory information [22]. Gamma oscillations are associated with increased alertness, cognitive processing, and brain cell synchronisation.
Sleep States and their Impact on Biopsychological Well- Being
Each phase of sleep, characterized by specific brain wave patterns and physiological alterations, is a dynamic phenomenon. SWS primarily facilitates the consolidation of memories, physical recuperation, and hormonal balance. Researchers have linked disruptions in slow-wave sleep (SWS) to reduced cognitive performance, mood disorders, and a weakened immune system, highlighting its importance for overall physical, mental, and social well-being. Rapid Eye Movement (REM) sleep is characterised by asynchronous brain activity, suggesting awareness despite muscular atonia. During REM sleep, theta and beta waves are the predominant brain waves, reflecting increased brain activity and intense dreaming. REM sleep has a vital role in regulating emotions, consolidating memories, and facilitating creative problem- solving. Depriving oneself of REM sleep has been associated with mood problems, cognitive impairments, and changes in social behavior, highlighting its significance for overall biopsychosocial well-being.
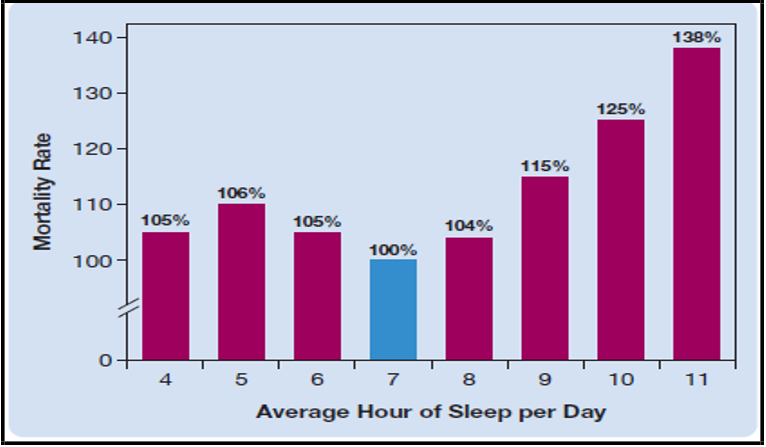
Biopsychosocial well-being refers to the comprehensive integration of biological, psychological, and social variables, emphasizing the interdependence of physical health, mental moods, and social connections. Sleep has a crucial role in affecting several facets of biopsychosocial well-being. [24] Liu et al. (2017) found a correlation between sleep and mortality. The study clearly established a correlation between inadequate or low-quality sleep and a higher likelihood of death from several causes. Consistently getting less sleep than advised, known as chronic sleep deprivation, has been associated with an increased risk of acquiring chronic illnesses, including cardiovascular disease, diabetes, obesity, and hypertension. These disorders are major contributors to death rates. Furthermore, studies have linked sleep problems like sleep apnea, insomnia, and restless legs syndrome to an increased risk of death. In contrast, placing imporContrarily, consistent data indicates that both the length and quality of sleep are crucial for maintaining excellent health and a long life, highlighting the importance of obtaining sufficient and rejuvenating sleep as a safeguard against death. e crucial significance of sleep in general health and the need to encourage regular sleep habits as a preventative intervention against early death.
Figure 8 Point up the correlation between sleep and mortality.
Figure 8- Note: adoped from [24] Liu, T. Z., Xu, C., Rota, M., Cai, H., Zhang, C., Shi, M. J., & Sun, X. (2017).
Sufficient sleep is crucial for maintaining physiological balance, which includes immune function, hormone control, and cellular repair processes. Disturbances in sleep patterns, such as insomnia or sleep disorders, may result in systemic inflammation, metabolic dysregulation, and heightened vulnerability to infections. Sleep is crucial for cognitive performance, emotional control, and mood stability from a psychological perspective. Sleep deprivation hampers cognitive functions such as attention, memory, and decision-making, which negatively impact academic and vocational performance. Sleep difficulties frequently worsen emotional disorders, such as anger, anxiety, and sadness, leading to psychological anguish. Sleep patterns and the quality of sleep significantly impact interpersonal connections, social interactions, and communication abilities. Persistent sleep deprivation may result in social isolation, anger, and interpersonal disputes, causing disruptions in social support systems. Shift employment, inconsistent sleep patterns, and societal demands might weaken sleep hygiene, intensifying social stresses and decreasing social well-being.
Brain waves and sleep states have a crucial role in controlling a wide range of physiological, cognitive, and emotional processes, which have a significant influence on overall biopsychosocial well-being. Understanding the complex relationship between sleep and biopsychosocial variables is critical for enhancing overall well-being and developing the ability to cope with the difficulties posed by contemporary lifestyles. Individuals may develop a well-rounded approach to well-being by giving importance to good sleep habits, treating sleep disorders, and acknowledging the many ways in which sleep affects human functioning, including biological, psychological, and social aspects.
Neurotransmitters and Sleep Regulation
GABAergic inhibition is the process in which gamma-aminobutyric acid (GABA), the principal inhibitory neurotransmitter in the brain, plays a vital role in initiating and sustaining sleep. GABAergic neurons in the hypothalamus and brainstem help with non-rapid eye movement (NREM) sleep by blocking areas that make you awake and making neurons work together better. Gamma-aminobutyric acid (GABA) is the main neurotransmitter that reduces activity in the central nervous system, helping to maintain a careful equilibrium between neuronal stimulation and suppression. The crucial function of controlling neuronal activity extends to a range of physiological activities, including sleep regulation. GABAergic inhibition, facilitated by GABAergic neurons and receptors, has a significant impact on the initiation, continuity, and structure of sleep.
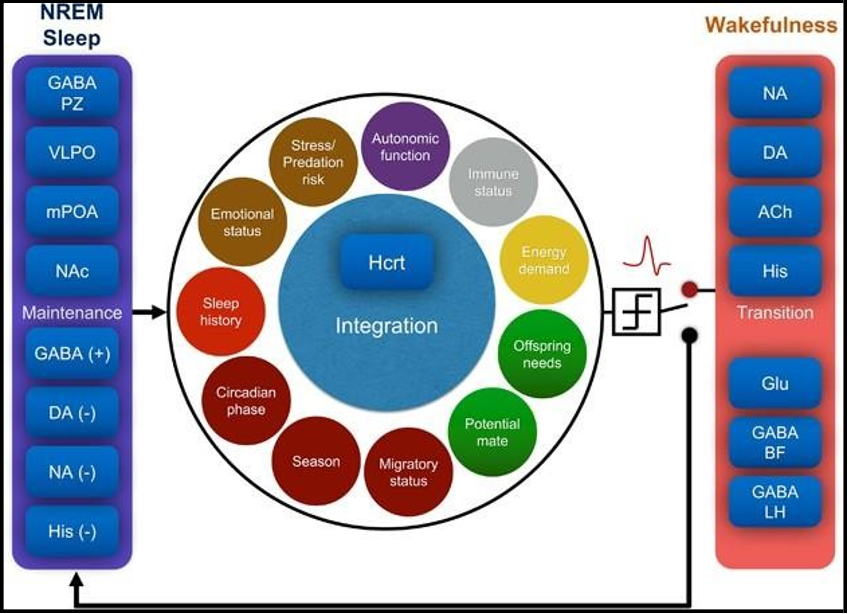
Figure 9: illustrates the role of neurotransmitters in regulating sleep.
Figure 9- Note: Adopted from Eban-Rothschild, A., Appelbaum, L. & de Lecea, L. Neuronal Mechanisms for Sleep/Wake Regulation and Modulatory Drive. Neuropsychopharmacol. 43, 937–952 (2018). https://doi.org/10.1038/npp.2017.294
Understanding GABAergic Inhibition
The enzyme glutamic acid decarboxylase (GAD) produces GABA from glutamate. It exerts its effects by interacting with two main kinds of receptors: GABA-A and GABA-B receptors. GABA-A Ligands activate receptors, which are chloride channels primarily found at synapses throughout the brain. When GABA binds to these receptors, it causes the receptors to alter shape, which results in the entry of chloride ions into the neuron and the neuron being more negatively charged. There are many different subunit combinations in GABA-A receptors, which change how they work, where they are found in cells, and how they pharmacologically behave. Activation of GABA- A receptors leads to neural inhibition, which reduces excitatory impulses and enhances relaxation and serenity.
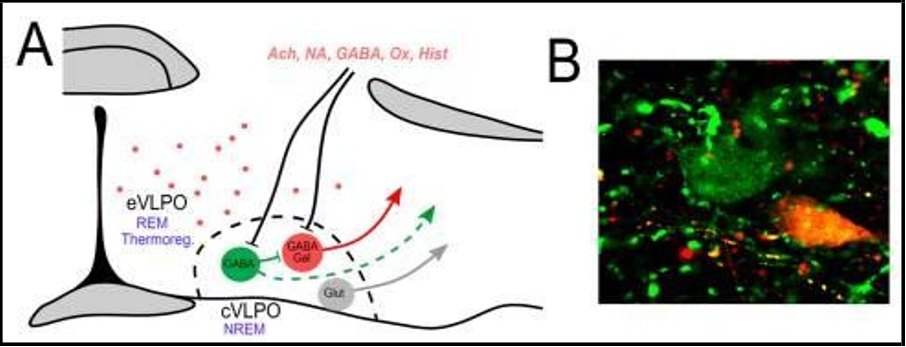
GABA-B receptors are located both pre- and postsynaptically in the central nervous system and belong to the class of metabotropic G- protein-coupled receptors. When GABA-B receptors are activated, they shut down presynaptic calcium channels and change postsynaptic potassium channels. This makes neurons more hyperpolarized and less excitable. GABA-B receptors have a greater influence on neuronal activity than GABA-A receptors, resulting in longer-lasting and modulating effects. This contributes to synaptic plasticity and neural network synchronization. The complex system of GABAergic neurons and receptors controls the shift from being awake to being asleep, with GABAergic inhibition playing a vital role in promoting NREM sleep. Hypothalamic GABAergic neurons located in the ventrolateral preoptic region (VLPO) of the hypothalamus play a crucial role in regulating sleep [14]. Figure 10 depicts the sleep-promoting hub.
Figure 10: Note: Adopted from Pinel, J. P. J., Barnes, S. (2021). Biopsychology. Brazil: Pearson.
As a central hub, the ventrolateral preoptic nucleus (VLPO) helps people fall asleep by sending signals that make them less alert to parts of the brain that make people awake, like the arousal nuclei in the brainstem and hypothalamus. Sleep heightened the activity of GABAergic neurons in the VLPO, suppressing circuits that promote awakeness and triggering the onset of NREM sleep. Researchers have linked sleep disorders like insomnia and narcolepsy to the malfunction of GABAergic neurons in the hypothalamus, underscoring their crucial role in regulating sleep patterns. Luppi & Fort (2019) [25] investigate theories about the processes that govern the shifts between the three stages of vigilance: wakefulness, nonrapid eye movement (non-REM) or slow-wave sleep (SWS), and rapid eye movement (REM) sleep, commonly referred to as paradoxical sleep (P.S.). The functioning of several waking systems, including the serotonergic, noradrenergic, cholinergic, and hypocretin systems, triggers the start of waking. Both the circadian clock and adenosine, a sleep-inducing substance that accumulates while awake, activate SWS-active neurons during the onset of sleep [28]. Research suggests that the stimulation of GABAergic neurons in the ventrolateral preoptic nucleus, along with other GABAergic systems in other brain areas, may cause slow-wave sleep (SWS). Extensive empirical data supports the interplay of several populations of neurons in the posterior hypothalamus and brainstem that release the neurotransmitters glutamate and GABA, facilitating the shift from slow-wave sleep (SWS) to paradoxical sleep (P.S).
There are GABAergic neurons in the brainstem, specifically in the pontine tegmentum and medullary reticular formation. These neurons control REM sleep and the changes between sleep and wakefulness. The ventral periaqueductal grey (vPAG), which is made up of a lot of GABAergic neurons, manages REM sleep by making connections with parts of the brain that stop REM sleep, like the locus coeruleus. By turning off REM-off cells, stimulating GABAergic neurons in the vPAG leads to REM sleep. This makes REM-related motor activities and intense dreams more likely to happen. Researchers have linked REM sleep behavior disorder (RBD) and other parasomnias to disruptions in the transmission of GABAergic neurotransmitters in the brainstem, highlighting the complex role of GABAergic inhibition in regulating REM sleep.
It's possible for neurons to synchronize and oscillate when GABAergic neurons help to coordinate neuronal activity and make rhythmic patterns that are linked to different stages of sleep. If you go into non-rapid eye movement (NREM) sleep, your brain waves are slow. During this type of sleep, GABAergic interneurons help make slow oscillations (less than 1 Hz) and sleep spindles (12–15 Hz). These neuronal activities encourage brain activity synchronization and memory consolidation. The inhibitory effects of GABA disrupt the regularity of sleep-related oscillations, resulting in fragmented sleep patterns and reduced cognitive performance.
Sleep Disorders and Therapeutics
Researchers have extensively studied several sleep problems throughout the years, most of which are associated with higher rates of illness and death.
Insomnia
Van der Zweerde et al. (2019) suggest that understanding the function of GABAergic inhibition in sleep regulation will help us better understand the underlying causes of sleep disorders and create drugs that target GABAergic neurotransmission. Researchers have linked the disruption of GABAergic neurotransmission, specifically in the VLPO and thalamus, to insomnia. Insomnia is characterized by changes in sleep structure, which may lead to problems falling or staying asleep. This can disrupt sleep and reduce its effectiveness. Insomniacs may have a longer time to fall asleep, more arousal after falling asleep, and less deep sleep and REM sleep.
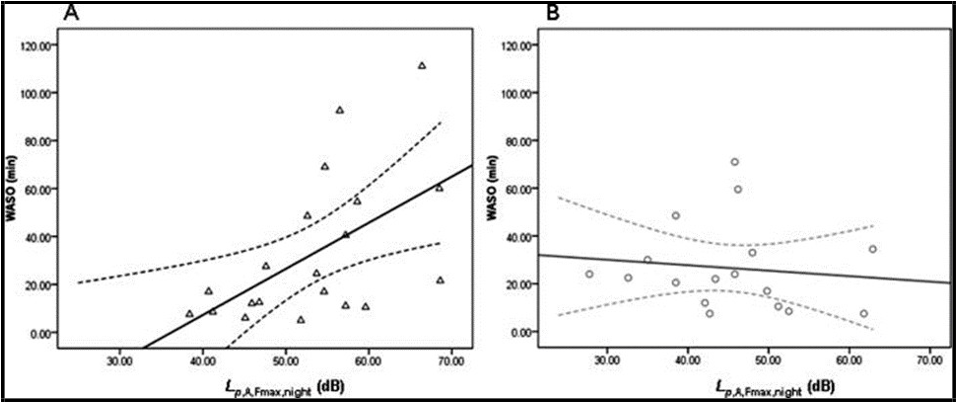
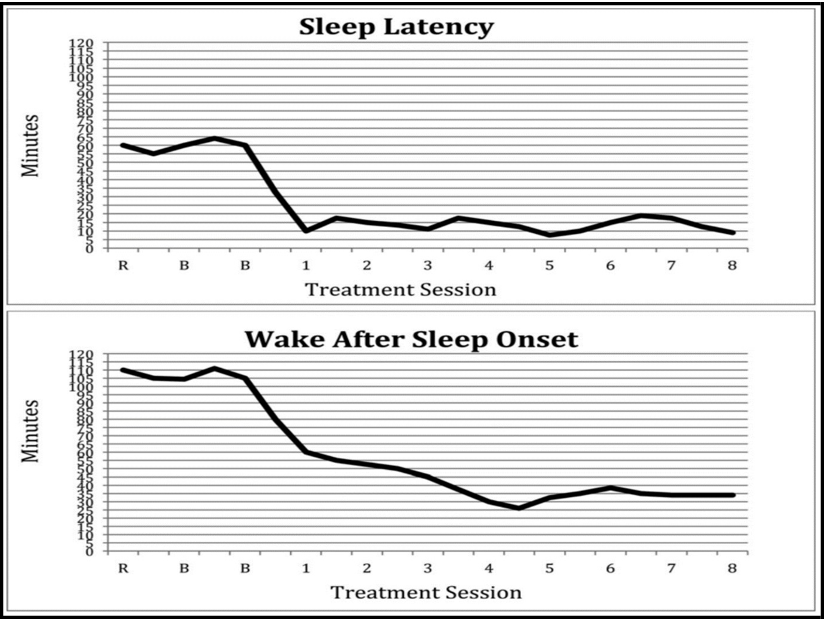
Figure 11: displays the state of wakefulness after the onset of sleep.
Figure 11- Note: Adopted from van der Zweerde, T., Bisdounis, L., Kyle, S. D., Lancee, J., & van Straten, A. (2019).
The state of wakefulness after sleep onset (WASO) is defined as the amount of time spent awake after first falling asleep during the sleep phase. WASO, or wake after sleep onset, is a common and critical feature of the insomnia condition. These people may have challenges sustaining uninterrupted sleep throughout the night, often waking up and facing difficulties falling back asleep. Individuals with insomnia have increased levels of alertness, intrusive thoughts, stress, discomfort, and disruptions in their surroundings, which contribute to wake-after-sleep onset (WASO). In addition, sleep patterns and behaviours that are not well-suited to one's needs may continue the pattern of being awake, such as spending too much time in bed while not sleeping or participating in stimulating activities just before going to bed.
In individuals with insomnia, WASO, or wake after sleep onset, not only interrupts sleep but also leads to daytime tiredness, reduced cognitive abilities, and a general decline in quality of life [42]. Changes in sleep structure may indicate increased alertness and heightened mental activity during sleep, which may contribute to the ongoing problem of insomnia and negatively impact daily performance. GABAergic agonists, such as benzodiazepines and non-benzodiazepine hypnotics, increase GABA inhibitory effects and facilitate sleep initiation and continuation in insomnia. Nevertheless, prolonged use of GABAergic medications might result in the development of tolerance, dependency, and rebound insomnia. Consequently, it is crucial to closely monitor patients and provide further behavioural therapy as necessary.
Narcolepsy is a neurological disorder characterised by excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep.
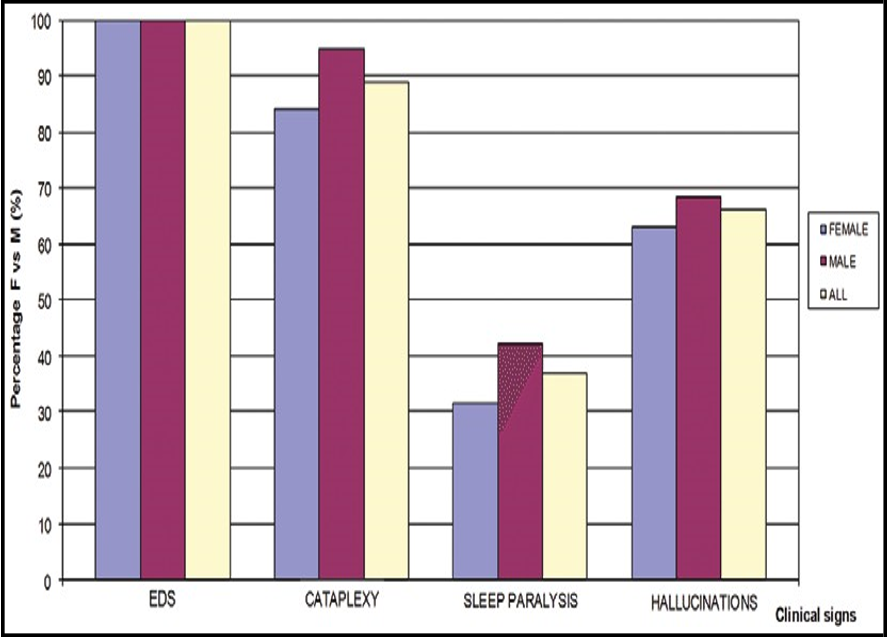
Deficits in GABAergic tone in the VLPO and orexinergic neurons in the hypothalamus cause the symptoms of narcolepsy, including excessive daytime drowsiness and cataplexy. Narcolepsy an abundance of tiredness throughout the day, rapid loss of muscular tone known as cataplexy, an inability to move during sleep paralysis, and hallucinations that occur while falling asleep, known as hypnagogic hallucinations, distinguish Narcolepsy is characterized by changes in sleep structure, such as quick shifts from being awake to entering REM sleep, irregular sleep patterns, and disturbances in REM sleep control.
Figure 12: shows Clinical Signs of Narcolepsy.
Figure 12- Note: Adopted from Antelmi, E., Pizza, F., Donadio, V., Filardi, M., Sosero, Y., Incensi, A., Vandi, S., Moresco, M., Ferri, R., Marelli, S., Ferini-Strambi, L., Liguori, R., & Plazzi, G. (2019). Biomarkers for REM sleep behavior disorder in idiopathic and narcoleptic patients. Annals of Clinical and Translational Neurology, 6, 1872 - 1876.
https://doi.org/10.1002/acn3.50833
The dysregulation of neurotransmitter systems, specifically hypocretin/orexin insufficiency, may cause the disturbance of sleep- wake transitions and REM sleep control in narcolepsy. When GABAergic drugs are mixed with wake-promoting drugs or specific orexin receptor antagonists, they may help people with narcolepsy feel better and sleep better [1]. Precisely adjusting the activity of GABAergic neurotransmission shows potential for developing new treatments that may improve the structure of sleep and reduce the negative effects of narcolepsy on everyday activities.
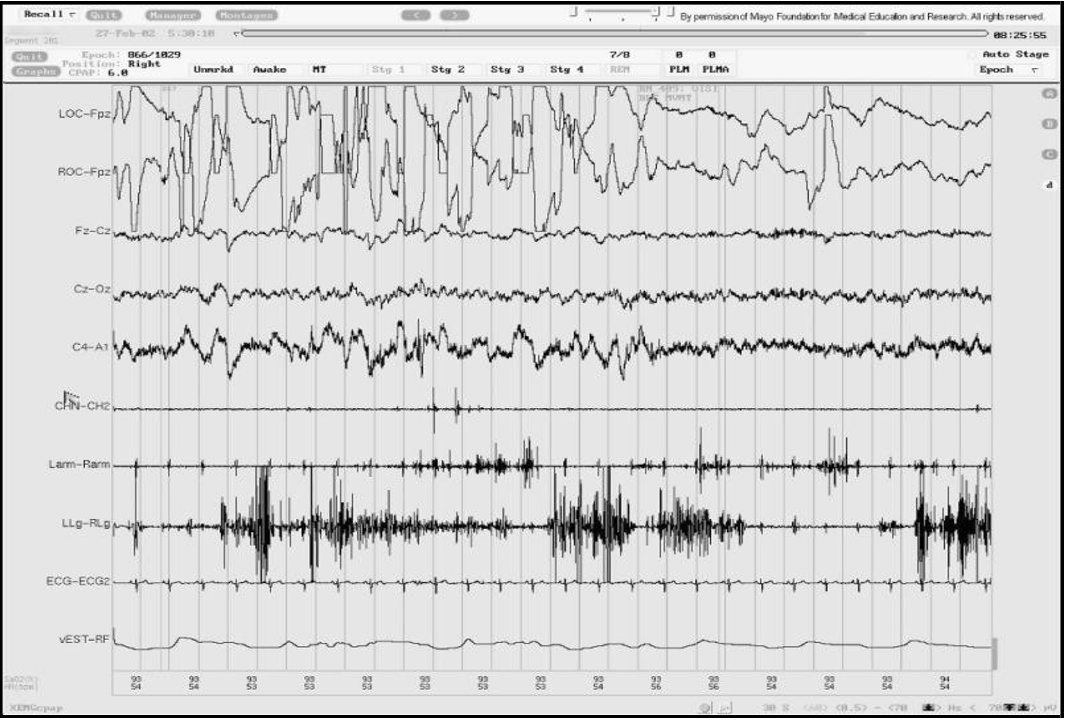
A malfunction of GABAergic neurons in certain areas of the brainstem, such as the vPAG and pontine tegmentum, causes REM Sleep Behavior Disorder (RBD). This malfunction leads to the loss of muscular paralysis during REM sleep and the acting out of dream material. Clonazepam, a type of GABAergic agonist, efficiently inhibits REM sleep motor behaviors and decreases the occurrence of RBD episodes, thereby improving the safety and overall quality of life for those afflicted. We can use cognitive-behavioral therapy and environmental adjustments in conjunction with medicine to manage the symptoms of RBD and minimize the risk of damage during sleep disruptions. The EEG picture of REM sleep behavior disorder (RBD) often shows clear patterns that suggest aberrant brain activity during rapid eye movement (REM) sleep.
Individuals with RBD may have EEG recordings that display heightened muscular tone during REM sleep episodes, often accompanied by periodic bursts of phasic muscle activity. These bursts of muscular activity are atypical and might seem like abrupt spasms or contractions in the limbs or other regions of the body. The absence of atonia, the typical inhibition of muscular activity during this sleep period, distinguishes REM sleep in RBD. This results in physical movements that mimic the content of dreams. The abnormal EEG results in RBD show that the condition is caused by problems in the brain and body's neurophysiology, such as problems with motor control during REM sleep. This disruption leads to potentially disruptive behaviors and an increased risk of damage during sleep.
Figure 13 displays an image of an EEG depicting REM sleep behavior disorder (RBD).
Figure 13- Note: Adopted from [38] St. Louis, E. K., Frey, L. C., Britton, J. W., Frey, L. C., Hopp, J. L., Korb, P., Koubeissi, M. Z., Lievens, W. E., Pestana-Knight, E. M., & St. Louis, E. K. (Eds.). (2016). Electroencephalography (EEG): An Introductory Text and Atlas of Normal and Abnormal Findings in Adults, Children, and Infants. American Epilepsy Society.
GABAergic inhibition plays a fundamental role in regulating sleep by having broad impacts on neuronal excitability, synchronization, and oscillations. GABAergic neurons and receptors in the hypothalamus, brainstem, and cortical circuits work together in a complex way to control the change between awake and sleep states. This makes sure that the structure and quality of sleep are maintained. The disruption of GABAergic neurotransmission is the root cause of different sleep disorders. This requires specific drug treatments and comprehensive management strategies to restore the balance of sleep regulation and improve overall health. Through the exploration of the intricate mechanisms of GABAergic inhibition in sleep regulation, scientists and medical professionals are creating opportunities for groundbreaking approaches to enhance sleep quality and tackle the many difficulties associated with sleep disorders in modern society.
Monoaminergic Modulation
Neuromodulatory systems are changed by the serotoninergic, noradrenergic, and dopaminergic pathways, which help control when you sleep or wake up and your level of alertness. Serotonin and norepinephrine improve alertness, but dopamine governs the state of being awake and the processing of pleasurable experiences, thereby controlling the structure of sleep and the body's natural cycles. Neuronal circuits and neurotransmitter systems intricately interact to regulate sleep and wakefulness. Of these, the serotonergic, noradrenergic, and dopaminergic pathways are responsible for monoaminergic regulation, which is crucial for regulating arousal states and transitions between sleep and wakefulness. Serotonin and norepinephrine enhance alertness, but dopamine governs the state of being awake and the processing of pleasurable experiences, affecting the structure of sleep and the control of the body's internal clock. Scientists have investigated the ways in which monoaminergic modulation affects the regulation of sleep and wakefulness. They have specifically focused on understanding the role of each neurotransmitter system, how it contributes to sleep disorders, and potential treatments.
Serotonergic Modulation
Tryptophan produces serotonin, or 5-hydroxytryptamine (5-HT), which serves as a neurotransmitter in the central nervous system. Serotonergic neurons typically originate from the raphe nuclei located in the brainstem. These neurons have extensive projections to various locations in the cortex and subcortex. Serotonin promotes wakefulness by stimulating the thalamus, hypothalamus, and basal forebrain, thus activating the ascending arousal pathways. When awake, activation of serotonergic pathways increases cortical excitability and alertness, which improves the processing of sensory information and cognitive activities. Pharmacological substances that enhance serotonin levels, such as selective serotonin reuptake inhibitors (SSRIs), have the ability to promote wakefulness and are used in the treatment of sleep disorders characterised by excessive daytime drowsiness, such as narcolepsy and idiopathic hypersomnia. In addition to its ability to promote wakefulness, serotonin also plays a role in regulating the structure of sleep by influencing both REM sleep and NREM sleep. During REM sleep, serotonergic neurons have higher firing rates, indicating their involvement in regulating both the beginning and maintenance of REM sleep. Disruption of the normal functioning of serotonin neurotransmission has been linked to sleep disorders such as insomnia, sleep problems associated with depression, and REM sleep behaviour disorder (RBD).
Adrenergic Modulation
Dopamine produces norepinephrine, also known as noradrenaline, which serves as a neurotransmitter and stress hormone. Neural transmission begins at the locus coeruleus in the brainstem and then spreads extensively across the brain. Norepinephrine plays a vital role in enhancing alertness and sustaining a state of being awake by sending signals to the thalamus, cortex, and basal forebrain. Activation of the noradrenergic system increases cortical excitability and attention, thereby improving cognitive functioning and responsiveness to environmental cues. Noradrenergic system dysfunction has been linked to sleep disorders characterised by excessive daytime drowsiness, such as narcolepsy and obstructive sleep apnea (OSA) [31]. Norepinephrine controls the change from sleeping to being awake by making you more alert and turning off parts of your brain that make you sleepy, like the ventrolateral preoptic nucleus (VLPO) in the hypothalamus.
Although a person is awake, noradrenaline stops neurons in the ventrolateral preoptic nucleus (VLPO) from working that make you sleepy. This keeps you awake and alert [6]. People treat sleep disorders characterised by excessive daytime drowsiness and exhaustion with pharmacological substances that enhance noradrenergic activity, such as stimulants and wake-promoting drugs.
Dopaminergic Modulation
Tyrosine produces the neurotransmitter dopamine, which plays a crucial role in reward processing, motivation, and motor control. Numerous nuclei, including the substantia nigra and ventral tegmental area (VTA), produce dopaminergic neurons. Dopamine regulates wakefulness and the processing of pleasurable experiences, influencing motivation, enjoyment, and reinforced behaviors. The VTA sends dopaminergic projections to the nucleus accumbens and prefrontal cortex, which regulate arousal states as well as cognitive processes related to motivation and goal-directed behavior. Siddarth et al. (2021) found a strong correlation between sleep quality and many elements of cognitive performance, both objectively and subjectively, in middle-aged and older persons who had minor memory complaints. The research revealed a correlation between worse sleep quality, increased sleep disruption, and less sustained attention. Conversely, a longer time to fall asleep and feeling sleepy throughout the day were associated with a higher incidence and severity of memory lapses. These results indicate that therapies aimed at enhancing sleep quality may increase the capacity to concentrate on activities and reduce memory issues in this group.
Disruption in the transmission of dopamine neurotransmitters may cause interruptions in the continuity of sleep and result in changes in the structure of sleep, which can contribute to sleep disorders and related health conditions.
Gaining a comprehensive understanding of how monoaminergic modulation affects the regulation of sleep and wakefulness is crucial for effectively treating sleep disorders and creating specific pharmaceutical treatments. The management of sleep disorders often involves the use of pharmaceuticals that specifically affect the transmission of monoaminergic neurotransmitters, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and dopamine agonists. These drugs regulate alertness levels, improve sleep quality, and relieve symptoms associated with sleep disorders such as insomnia, excessive sleepiness, and abnormal sleep behaviours. Nevertheless, the effectiveness and capacity to tolerate pharmaceutical therapies differ across people, emphasising the need for tailored treatment methods and vigilant observation of adverse reactions.
Aside from medication, making adjustments to activities of daily living (ADL) is essential for maximising sleep health and enhancing general well-being. Approaches such as implementing sleep hygiene habits, using stress management approaches, and utilising cognitive- behavioural therapy for insomnia (CBT-I) target the root causes of sleep disruptions and enhance the effectiveness of medication-based treatments. Providing information on the significance of sleep and the effects of lifestyle variables, such as coffee use, alcohol intake, and electronic device usage, may enable people to make knowledgeable decisions and give priority to maintaining good sleep habits.
Monoaminergic regulation, facilitated by the serotonergic, noradrenergic, and dopaminergic pathways, controls the shifts between sleep and wakefulness, as well as the levels of alertness. Serotonin and norepinephrine enhance alertness, but dopamine controls both wakefulness and reward processing, affecting sleep structure and the body's natural sleep-wake cycle. The disruption of monoaminergic neurotransmission has a role in the development of different sleep disorders, highlighting the need for specific drug treatments and comprehensive management strategies. Researchers and clinicians aim to enhance therapy options and improve outcomes for people with sleep problems by clarifying the processes of monoaminergic modulation in sleep-wake regulation.
Research in the field of biopsychology has revealed the fundamental processes involved in several sleep disorders, such as insomnia, sleep apnea, narcolepsy, and parasomnias. Dysregulation of neurotransmitter systems, changes in sleep architecture, and genetic predispositions influence the pathophysiology of these illnesses. Sleep, a vital physiological function, is crucial for general health and well-being. Nevertheless, the emergence of sleep problems often disrupts sleep, making it difficult for many people to get enough sleep. These disorders include a wide variety of illnesses, ranging from difficulty sleeping and excessive sleeping to abnormal sleep behaviors and disruptions in the body's natural sleep-wake cycle. This research focuses on the complex interplay of several variables that contribute to the development of sleep disorders. These factors include dysregulation of neurotransmitter systems, changes in the structure of sleep patterns, and genetic predispositions.
Neurotransmitters work as chemical messengers in the brain, coordinating the intricate interaction of neuronal activity that controls the sleep-wake cycle. Imbalances in neurotransmitter systems may significantly affect sleep structure and lead to the emergence of different sleep disorders.
Serotonin, a neurotransmitter derived from tryptophan, plays a crucial role in the regulation of mood, cognition, and sleep-wake cycles. The disruption of serotonin sign Researchers have linked the underlying mechanisms of insomnia, characterised by difficulties in either initiating or maintaining sleep, to the disruption of serotonin signalling. transporters, and metabolising enzymes may upset the equilibrium between pathways that promote wakefulness and those that promote sleep, leading to sleep disorders.
The locus coeruleus and other brainstem nuclei release norepinephrine, a neurotransmitter that regulates the state of wakefulness, focus, and alertness. Disruption of noradrenergic signalling has been associated with sleep disorders such as narcolepsy and obstructive sleep apnea (OSA). Excessive levels of noradrenergic activity may interrupt the continuity of sleep and result in daytime drowsiness, while a lack of noradrenergic tone can interfere with the systems that keep us awake and cause fragmented sleep patterns [15]. Dopamine, a neurotransmitter responsible for modulating reward processing, motivation, and motor control, plays a crucial role in regulating sleep-wake cycles. Researchers have linked restless legs syndrome (RLS) and periodic limb movement disorder (PLMD), characterised by involuntary movements during sleep, to the dysregulation of dopaminergic signalling. Changes in dopamine receptors and transporter function may cause the sensory pain and sleep disturbance reported in RLS and PLMD.
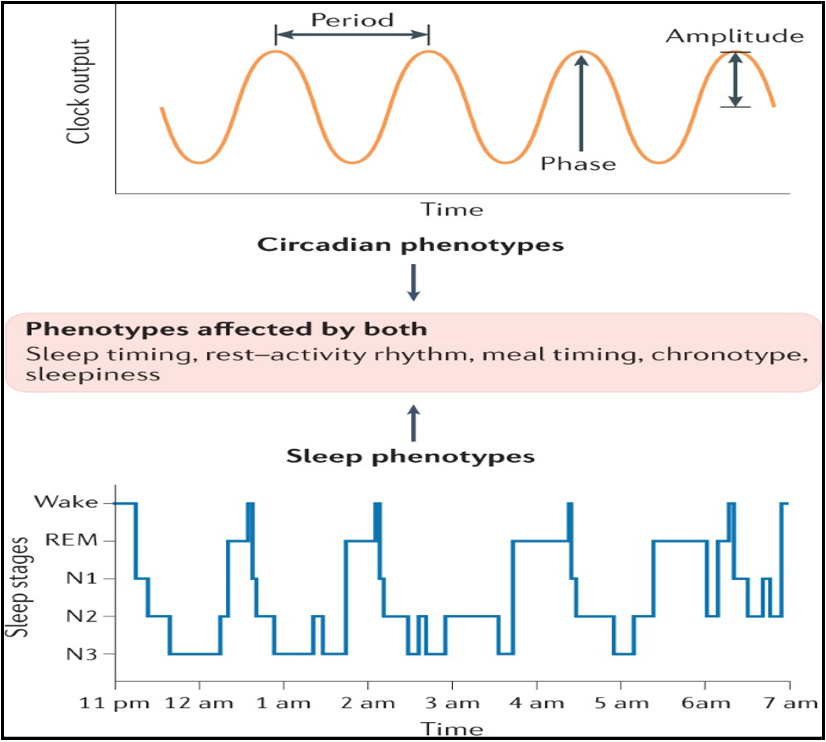
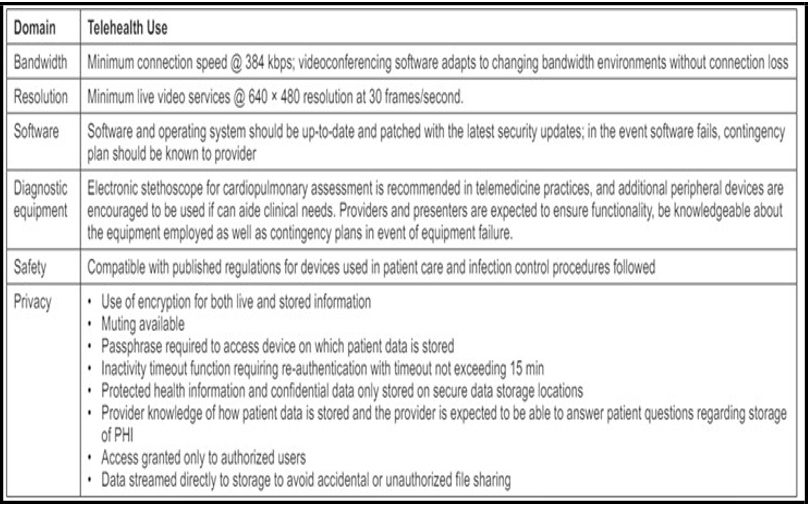
Genetic Predisposition to Sleep
Identifying genetic predispositions may provide valuable insights into the fundamental processes of sleep disorders and guide personalised treatment strategies. Sleep disorders often demonstrate familial clustering, with a greater occurrence seen among persons who have family members afflicted by the condition. Genetic variability has a significant impact on the regulation of sleep and wakefulness patterns in people, via circadian phenotypes. Alterations in the circadian rhythm, which governs the time and length of sleep-wake cycles, may occur due to genetic differences in clock genes such PERIOD, CLOCK, and BMAL1 [36]. These variances might appear as disparities in preferred sleep schedules, vulnerability to sleep disorders, and reactions to environmental stimuli like exposure to light. Moreover, variations in genes linked to neurotransmitter systems, such as serotonin and dopamine, may regulate sleep regulation and impact circadian characteristics. The variability in sleep and wakefulness patterns across people is a result of the complex interaction between hereditary determinants and environmental effects. This emphasises the delicate link between genetics and the circadian control of sleep. Figure 14 depicts the genetic basis of circadian rhythms.
Figure 14: Note: Adopted from Sinnott-Armstrong, W., & Summers, J. (2020). Which biopsychosocial view of mental illness? , 82-96.
https://doi.org/10.1093/MED/9780198789697.003.0006.
Researchers in genetics have identified specific genes associated with sleep disorders. These genes include circadian rhythm genes like CLOCK and PER3, neurotransmitter receptor genes like 5-HT2A and DRD2, and genes implicated in sleep regulation like DEC2 and ADA [37]. Genetic variations in these genes may make individuals more prone to sleep problems by interfering with the transmission of neurotransmitters, disturbing the natural sleep-wake cycle, or affecting the regulation of sleep intensity. Genome-wide Association Studies (GWAS) have found specific genetic changes that make people more likely to have sleep disorders. This tells us a lot about how these conditions are caused by genes. GWAS has found particular genomic areas that are associated with insomnia, narcolepsy, restless legs syndrome, and other sleep disorders. These results highlight the intricate genetic complexity of these disorders and emphasise the involvement of several biological processes. Gaining a comprehensive understanding of the intricate relationship between dysregulation of neurotransmitters, changes in sleep patterns, and genetic predispositions in sleep disorders is crucial for the development of effective treatment and preventative strategies.
Progress iAdvancements in genetics and neuroscience offer the possibility of developing tailored strategies to tackle sleep issues, tailored to each individual's genetic composition and neurobiological functions. sting and biomarker analysis may assist in identifying people who have a higher likelihood of developing sleep problems. We can then use this information to guide specific therapies that aim to restore the balance of neurotransmitters and improve the structure of sleep. Understanding the genetic factors behind sleep problems might help in the discovery of new targets for pharmaceutical treatment. Efforts to create drugs that specifically target neurotransmitter systems, regulate circadian rhythms, and improve sleep homeostasis may provide alternative therapeutic choices for patients with sleep disorders that do not respond to traditional therapy.
Sleep disorders are a variety of illnesses that involve disruptions in neurotransmitter systems, changes in sleep structure, and hereditary tendencies. Gaining a comprehensive understanding of the intricate interaction between these elements is crucial for deciphering the underlying mechanisms of sleep disorders and devising efficient approaches for their diagnosis, treatment, and prevention. Researchers and clinicians aim to improve general sleep health and psychological well-being by clarifying the neurobiological pathways that cause sleep disorders.
Disturbances in the structure and uninterrupted nature of sleep may negatively affect cognitive abilities, emotional control, and mental well-being, underscoring the need for maintaining good sleep habits and using behavioural therapies. Researchers have used a combination of scientific and psychological approaches to understand the complex details of sleep structure, the modulation of neurotransmitters, and the specific brain areas that play a role in regulating sleep. The findings from this study have significant consequences for health and illness, highlighting the need to prioritize sleep health and encourage cooperation across different fields to tackle the intricacies of sleep-related problems.
To better understand sleep and find innovative ways to improve its quality and overall impact on well-being, it is crucial to use interdisciplinary methods. Sleep problems, which include various illnesses such as insomnia, sleep apnea, and circadian rhythm disturbances, provide considerable obstacles to people's health and overall well-being. Treatments should target the biological, psychological, and social variables that contribute to the development and persistence of these illnesses, acknowledging their complex character. Researchers are studying the concepts and efficacy of biopsychosocial therapies for treating sleep disorders. They highlight the importance of a holistic approach to therapy, which has the potential to enhance results and improve the quality of life for those with sleep disorders. Interventions aimed at biological determinants may include pharmaceutical therapies, dietary and lifestyle changes, and the control of concurrent medical disorders [15].
Stress, worry, sadness, and unhelpful thoughts about sleep are important factors in causing and maintaining sleep disturbances. Cognitive-behavioral treatments (CBT) for insomnia, relaxation methods, mindfulness-based interventions, and stress management strategies target psychological factors that contribute to sleep disruptions and promote the development of effective coping mechanisms. Social determinants of health, such as socioeconomic position, occupational circumstances, family dynamics, and social support networks, influence sleep quality and patterns.
Interventions aimed at social variables may include addressing environmental issues that interrupt sleep, enhancing sleep hygiene behaviours, and offering information and support to people and their families. Cognitive-behavioural treatment for insomnia (CBT-I) encompasses several interventions such as sleep restriction therapy, stimuli control methods, relaxation training, cognitive restructuring, and sleep hygiene education. Pharmacological therapies, like sedative-hypnotic medicines, complement behavioural approaches or serve as temporary supplements for severe cases of insomnia.
The main treatment for obstructive sleep apnea (OSA) is CPAP therapy, which involves delivering pressurised air via a mask to maintain an open airway during sleep. Behavioural therapies aimed at reducing body weight, positioning therapy, refraining from consuming alcohol and sedatives before going to bed, and consistent use of CPAP therapy improve the results for patients with obstructive sleep apnea (OSA). Individuals with structural anomalies that contribute to sleep apnea may be candidates for surgical procedures such as uvulopalatopharyngoplasty (UPPP) or mandibular advancement devices (MADs) [15].
Light therapy is an effective treatment for circadian rhythm disorders, such as delayed sleep-wake phase disorder (DSPD) and shift work sleep disorder (SWSD). It involves timed exposure to bright light in order to reset circadian rhythms. Behavioral therapies that focus on regulating sleep patterns, supplementing melatonin, and making environmental changes, such as reducing exposure to blue light at night, help to align the circadian rhythm with the desired sleep-wake schedule.
Effectiveness and Challenges of Biopsychological Interventions
Effectiveness
Biopsychosocial therapies for sleep disorders have been well recognised in the healthcare community for their efficacy in improving sleep outcomes, reducing symptoms, and boosting the general well-being of those struggling with these problems. Chronic sleep problems such as insomnia, sleep apnea, and circadian rhythm abnormalities present intricate difficulties that often need a thorough treatment strategy. Meta-analyses and systematic reviews consistently confirm the effectiveness of different treatments within the biopsychosocial paradigm, providing strong evidence for their practical use in clinical settings.
Out of all these treatments, cognitive behavioural therapy for insomnia (CBT-I) stands out as a fundamental approach for controlling long-term insomnia. It offers a systematic and research- supported approach to dealing with the cognitive and behavioural elements that contribute to sleep disturbances. CBT-I uses strategies such as sleep restriction, stimulus control, and cognitive restructuring to address and modify unhelpful beliefs and behaviours related to sleep. The goal is to promote better sleep patterns and improve overall sleep quality. Figure 15 depicts the impact of cognitive behavioural therapy for insomnia (CBT-I) on the amount of time it takes patients with insomnia to fall asleep, also known as sleep latency.
Figure 15: Note: Adopted from van der Zweerde, T., Bisdounis, L., Kyle, S. D., Lancee, J., & van Straten, A. (2019). Cognitive behavioral therapy for insomnia: A meta-analysis of long-term effects in controlled studies. Sleep medicine reviews 48, 101208.
https://doi.org/10.1016/j.smrv.2019.08.002
Van der et al. (2019) have shown that many trials consistently demonstrate the enduring efficacy of cognitive behavioural therapy for insomnia (CBT-I) in treating diverse sleep problems. This encompasses shortening sleep onset latency, prolonging total sleep time, and improving subjective evaluations of sleep quality. The results conclusively indicate cognitive behavioural therapy for insomnia (CBT-I) as the foremost therapy choice for those struggling with persistent insomnia [10]. Obstructive sleep apnea, a common but potentially serious sleep disease characterised by recurrent occurrences of partial or total obstruction of the upper airway during sleep, now widely recognises Continuous Positive Airway Pressure (CPAP) therapy as the primary treatment. CPAP treatment operates by continuously providing a pressurised airflow via a mask placed over the nose or mouth, successfully avoiding episodes of apnea and hypopnea while restoring regular breathing patterns [15]. CPAP therapy has been consistently proven effective in clinical trials for reducing symptoms of sleep apnea, such as excessive daytime sleepiness, cognitive impairment, and cardiovascular comorbidities. These findings emphasise the crucial role of CPAP therapy in improving both sleep-related and overall health outcomes for individuals with sleep apnea.
Light therapy has become a useful additional therapeutic method for circadian rhythm disorders, which are diseases that include disturbances in the body's internal biological clock. We use this therapy in conjunction with CBT-I and CPAP therapy. Light therapy helps to align the body's internal clock with the external environment by exposing individuals to bright light, usually in the morning or evening, depending on their specific circadian rhythm disturbance. This therapy supports the regulation of sleep-wake cycles and promotes better alignment of the overall circadian rhythm. Multiple research studies have shown the efficacy of light treatment in mitigating symptoms associated with circadian rhythm abnormalities, including delayed sleep phase disorder, shift work disorder, and seasonal affective disorder. Therefore, light therapy provides a non- pharmacological approach to dealing with these difficult situations. The effectiveness of biopsychosocial therapies for sleep disorders extends beyond their individual components. It encompasses the combined effects of biological, psychological, and social aspects that, together, impact sleep health. By incorporating various treatment methods within a biopsychosocial framework, healthcare providers can take a comprehensive and patient-focused approach to managing sleep disorders. This approach takes into account the underlying physiological processes as well as the psychological and social factors that contribute to sleep disturbances.
Furthermore, individualised treatment planning is crucial in maximising therapeutic results, as it enables healthcare professionals to customise therapies to the specific requirements, preferences, and circumstances of each patient. Healthcare practitioners may create customised treatment programmes that maximise adherence, effectiveness, and long-term success by taking into account aspects such as comorbid medical illnesses, medication use, lifestyle choices, and psychosocial stresses. Biopsychosocial therapies are essential in the treatment of sleep disorders because they provide a thorough and individualized approach to the intricate interaction of biological, psychological, and social components that contribute to these illnesses.
Within the biopsychosocial paradigm, there are several therapeutic methods available for those experiencing sleep problems. These include cognitive-behavioural therapies, CPAP therapy, light therapy, and more. Each of these approaches has distinct advantages and factors to consider while seeking relief. Healthcare practitioners may empower patients to attain restful sleep, improve overall health and well-being, and increase their quality of life by adopting a comprehensive and patient-focused approach to managing sleep disorders.
Challenges
Van der et al. (2019) have shown that many trials consistently demonstrate the enduring efficacy of cognitive behavioural therapy for insomnia (CBT-I) in treating diverse sleep problems. This encompasses shortening sleep onset latency, prolonging total sleep time, and improving subjective evaluations of sleep quality. The results conclusively indicate cognitive behavioural therapy for insomnia (CBT-I) as the foremost therapy choice for those struggling with persistent insomnia [10]. Obstructive sleep apnea, a common but potentially serious sleep disease characterised by recurrent occurrences of partial or total obstruction of the upper airway during sleep, now widely recognises Continuous Positive Airway Pressure (CPAP) therapy as the primary treatment. CPAP treatment operates by continuously providing a pressurised airflow via a mask placed over the nose or mouth, successfully avoiding episodes of apnea and hypopnea while restoring regular breathing patterns [15]. CPAP therapy has been consistently proven effective in clinical trials for reducing symptoms of sleep apnea, such as excessive daytime sleepiness, cognitive impairment, and cardiovascular comorbidities. These findings emphasise the crucial role of CPAP therapy in improving both sleep-related and overall health outcomes for individuals with sleep apnea.
Light therapy has become a useful additional therapeutic method for circadian rhythm disorders, which are diseases that include disturbances in the body's internal biological clock. We use this therapy in conjunction with CBT-I and CPAP therapy. Light therapy helps to align the body's internal clock with the external environment by exposing individuals to bright light, usually in the morning or evening, depending on their specific circadian rhythm disturbance. This therapy supports the regulation of sleep-wake cycles and promotes better alignment of the overall circadian rhythm. Multiple research studies have shown the efficacy of light treatment in mitigating symptoms associated with circadian rhythm abnormalities, including delayed sleep phase disorder, shift work disorder, and seasonal affective disorder. Therefore, light therapy provides a non- pharmacological approach to dealing with these difficult situations. The effectiveness of biopsychosocial therapies for sleep disorders extends beyond their individual components. It encompasses the combined effects of biological, psychological, and social aspects that, together, impact sleep health. By incorporating various treatment methods within a biopsychosocial framework, healthcare providers can take a comprehensive and patient-focused approach to managing sleep disorders. This approach takes into account the underlying physiological processes as well as the psychological and social factors that contribute to sleep disturbances.
Furthermore, individualised treatment planning is crucial in maximising therapeutic results, as it enables healthcare professionals to customise therapies to the specific requirements, preferences, and circumstances of each patient. Healthcare practitioners may create customised treatment programmes that maximise adherence, effectiveness, and long-term success by taking into account aspects such as comorbid medical illnesses, medication use, lifestyle choices, and psychosocial stresses. Biopsychosocial therapies are essential in the treatment of sleep disorders because they provide a thorough and individualized approach to the intricate interaction of biological, psychological, and social components that contribute to these illnesses.
Within the biopsychosocial paradigm, there are several therapeutic methods available for those experiencing sleep problems. These include cognitive-behavioural therapies, CPAP therapy, light therapy, and more. Each of these approaches has distinct advantages and factors to consider while seeking relief. Healthcare practitioners may empower patients to attain restful sleep, improve overall health and well-being, and increase their quality of life by adopting a comprehensive and patient-focused approach to managing sleep disorders.
Future Directions in Biopsychological Interventions
Recent technological progress, including smartphone apps, online cognitive-behavioural treatment (CBT) programmes, and wearable sleep monitoring devices, enables people to proactively take charge of their sleep health without leaving their homes [42]. Telehealth systems enable users to conveniently and easily monitor their sleep patterns, access educational materials, and participate in personalised treatment interventions.
Furthermore, the integration of sleep medicine services into primary care settings and the implementation of collaborative care models that include multidisciplinary teams show potential for improving sleep problem detection and treatment. These integrated care approaches improve the efficiency of diagnosing and arranging personalized treatments by incorporating sleep exams into regular general care visits and enabling communication among primary care doctors, sleep experts, psychologists, and sleep technologists. Coordinated care pathways and shared decision-making methods improve treatment engagement and continuity of care, especially for patients with complicated sleep-related comorbidities.
Biopsychosocial therapies are a comprehensive strategy for dealing with sleep disorders, acknowledging the complex interaction between biological, psychological, and social components that contribute to these illnesses. These treatments aim to improve sleep outcomes, quality of life, and general well-being by targeting the physiological mechanisms of sleep regulation as well as the psychological and social factors that influence sleep health [30]. Healthcare practitioners can improve the effectiveness of therapy and lessen the impact of sleep disruptions on people, families, and communities by customizing therapies to suit individual requirements and preferences within a complete biopsychosocial framework.
Although telehealth and digital health solutions have great potential, there are still obstacles to overcome in order to provide fair and equal access to these resources, especially for underprivileged populations and marginalised groups. The existence of disparities in digital literacy, internet connection, and technological access may impede the acceptance of telehealth platforms among certain demographic groups, thereby worsening inequalities in healthcare access and outcomes. It is crucial to implement community-based initiatives, public-private partnerships, and legislative interventions in order to tackle these gaps. This will ensure that everyone has an equal opportunity to take advantage of telehealth and digital health advancements.
Moreover, while collaborative care models have the potential to enhance the provision of sleep medicine services, it is crucial to overcome obstacles to multidisciplinary cooperation and communication in order to maximize care coordination and improve patient outcomes. The fragmentation of care, lack of standardised procedures for interdisciplinary cooperation, and funding hurdles for multidisciplinary services hinder the deployment of integrated care models [30]. To fully use the benefits of collaborative treatment for sleep disorders, healthcare organisations should cultivate a collaborative culture, develop effective communication channels, and provide incentives for team-based care.
Telehealth platforms, digital health treatments, and collaborative care models provide effective ways to address the difficulties of accessing, reducing stigma, and managing multiple health conditions in the treatment of sleep disorders. Healthcare providers can enhance the well-being of individuals with sleep disorders by using technology to increase access to evidence-based treatments, incorporating sleep medicine services into primary care, and implementing collaborative care approaches [39]. Effective telehealth for the management of sleep disorders necessitates the use of strong digital platforms, secure electronic health records, dependable internet access, and remote monitoring technologies. To provide comprehensive care and encourage patients to follow treatment and lifestyle changes, it is critical to have interdisciplinary teamwork and patient engagement initiatives in place. Telehealth improves the availability of high- quality healthcare, maximizing the effectiveness of treating sleep disorders and improving patient outcomes.
Table 1 presents the necessary conditions for using telehealth to manage sleep-related issues. Disorders.
Table 1: Note: Adapted from Singh, J., Badr, M. S., Diebert, W., Epstein, L. J., Hwang, D., Karres, V., Khosla, S., Mims, K. N., Shamim-Uzzaman, A., Kirsch, D. B., Heald, J. L., & McCann, K. M. (2015). American Academy of Sleep Medicine (AASM) Position Paper for the Use of Telemedicine for the Diagnosis and Treatment of Sleep Disorders. Journal of Clinical Sleep Medicine, 11(10), 1187–1198.
https://doi.org/10.5664/jcsm.5098
According to [35], telehealth only applies when specific qualifications are met to be effective. However, it has shown promising results in managing sleep disorders. Embracing a An essential aspect of improving the field of sleep medicine and achieving health equality for all is the use of a biopsychosocial framework that recognises the interconnectedness of sleep health and caters to the varied requirements of patients.
Potential future developments in sleep treatments may include the use of cutting-edge technology, such as artificial intelligence (AI) and machine learning algorithms, to tailor therapy methods and improve treatment results. AI-powered predictive analytics might empower physicians to detect patients with a high likelihood of developing sleep problems by analysing demographic, clinical, and behavioural data. This would allow for early intervention and the implementation of preventative measures.
Furthermore, advances in wearable sensor technology and home- based sleep monitoring devices may enable immediate evaluation of sleep patterns and therapy effectiveness, allowing people to actively participate in self-management tactics. Moreover, incorporating the concepts of behavioral sleep medicine into digital health treatments, such as providing information on sleep hygiene, teaching relaxation methods, and implementing stress management strategies, shows potential for treating the psychological and behavioral variables that contribute to sleep disruptions. Future biopsychosocial sleep interventions have the potential to revolutionise the field of sleep medicine and improve outcomes for individuals with sleep disorders. These interventions leverage a multidisciplinary approach that integrates cutting-edge technology with evidence-based behavioural interventions.
Current research and clinical investigation in biopsychosocial sleep therapies includes a range of techniques aimed at addressing the intricate interaction of biological, psychological, and social components that impact sleep health. Researchers are currently studying new drugs that target specific neurotransmitter systems involved in sleep regulation, such as orexin antagonists and melatonin agonists. Researchers are investigating the potential effectiveness of these drugs in treating various sleep disorders, such as insomnia and circadian rhythm disorders [14]. In addition, advancements in neuroimaging methods, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), have provided insights into the neural processes that cause sleep disruptions. This has aided in the development of specific interventions that manipulate brain activity to improve sleep quality. Cognitive-behavioral treatments in psychology are constantly developing. Researchers are developing new interventions that specifically target and address unhelpful thinking patterns, dysfunctional beliefs, and behavioural habits that lead to sleep disorders. Researchers have investigated many cutting-edge methods, such as internet-based cognitive behavioural therapy (CBT) programmes, virtual reality exposure therapy for insomnia, and mindfulness-based therapies, to boost the effectiveness of sleep treatments and make them more accessible. Primary care settings and community-based programmes are also incorporating psychoeducational therapies that enhance sleep hygiene, implement relaxation methods, and use stress management strategies. The goal is to improve sleep health and reduce the number of sleep disorders. From a social perspective, the recognition of therapies that target social determinants of sleep health, such as socioeconomic position, working circumstances, and social support networks, is growing. Supportive settings prioritise sleep as a fundamental aspect of general health and well-being. These efforts include community-based initiatives, workplace wellness programmes, and social prescribing schemes. Furthermore, initiatives aimed at diminishing social prejudice associated with sleep disorders and mental health problems are increasing awareness and approval, motivating people to actively seek assistance and participate in scientifically supported therapies without fear of criticism or bias.
Conclusion
To summarise, the field of biopsychosocial sleep therapies includes a diverse range of techniques that attempt to address the complex and numerous aspects of sleep health. Modern sleep medicine takes a broad and unified approach. It includes cutting-edge biological research on the neurochemical mechanisms that control sleep, new psychological therapies that target unhealthy thought patterns and behaviours, community-based interventions that deal with social factors that affect sleep, and individualised treatment plans that are made to fit each person's needs. Healthcare providers and researchers are developing new methods to intervene and prevent sleep patterns and disturbances by understanding how biological, psychological, and social factors interact. Their goal is to improve sleep outcomes and overall well-being. They are making significant progress in understanding the intricate interplay between sleep and health by fostering interdisciplinary cooperation among sleep specialists, psychologists, neuroscientists, and public health professionals. In addition, players in the field are striving to create social change by increasing knowledge about the significance of sleep health and lobbying for policies that support good sleep settings and behaviours. This aims to establish sleep as a basic aspect of overall well-being. Research, clinical innovation, and public health initiatives are actively shaping the field of sleep medicine. These efforts aim to improve the quality of sleep for everyone, enabling them to experience restorative and rejuvenating sleep. This, in turn, has the potential to enhance human health and well-being.
Acknowledgements
The author expresses sincere gratitude to LCUCK, located in London, United Kingdom, for providing the necessary platform to carry out this work. Additionally, I would like to thank Ms. W. Tewdores and Ms. A. Al-Janaby for meticulously reviewing the whole manuscript draft and offering valuable feedback.
Competing interests: The author reiterates that there are no conflicting interests that could potentially compromise the integrity of this research.
Funding: This work did not get any financial support.
Ethical Approval: This research does not include the participation of any human or animal participants.
Ethical compliance: The methods carried out in the studies involving human participants followed the moral standards set by the institutional and national research committee, the 1964 Helsinki Declaration and its subsequent revisions or similar ethical standards.
References
- Albqoor MA, Shaheen AM (2021) Sleep quality, sleep latency, and sleep duration: a national comparative study of university students in Jordan. Sleep breathing. 25(2): 1147–1154.
- Antelmi E, Pizza F, Donadio V, Filardi M, Sosero YL, et al. (2019) Biomarkers for REM sleep behavior disorder in idiopathic and narcoleptic patients. Annals of Clinical and Translational Neurology. 6(9): 1872 - 1876.
- Bainaboina G (2020) A Note on Biopsychology. Clinical and Experimental Psychology. 6(3): 01.
- Barone I, Hawks-Mayer H, Lipton JO (2019) Mechanisms of sleep and circadian ontogeny through the lens of neurodevelopmental disorders. Neurobiology of Learning and Memory. 160: 160-172.
- Breedlove SM, Watson NV (2013) Biological psychology: An introduction to behavioral, cognitive, and clinical neuroscience. Yale J Biol Med. 86(3): 435–6.
- Bringmann H (2018) Sleep-Active Neurons: Conserved Motors of Sleep. Genetics. 208(4): 1279 - 1289.
- Bubbico G, Iorio A, Lauriola M, Sepede G, Salice S, et al. (2019) Subjective Cognitive Decline and Nighttime Sleep Alterations, a Longitudinal Analysis. Frontiers in Aging Neuroscience. 11: 142
- Campbell LM, Kohli M, Lee EE, Kaufmann CN, Higgins M, et al. (2022) Objective and subjective sleep measures are associated with neurocognition in aging adults with and without HIV. Clin Neuropsychol. 36(6) : 1352–1371.
- Cieri F, Esposito R (2019) Psychoanalysis and Neuroscience: The Bridge Between Mind and Brain. Front Psychol. 10: 1790.
- Costa AN, McCrae CS, Cowan N, Curtis AF (2022) Paradoxical relationship between subjective and objective cognition: the role of sleep. J Clin Sleep Med. 18(8): 2009–2022.
- Cox RC, Olatunji BO (2020) Sleep in anxiety-related disorders: A meta-analysis of subjective and objective research. Sleep Med Rev. 51: 101282.
- Curtis AF, Costa AN, Musich M, Schmiedeler A, Jagannathan S, et al. (2024) Sex as a moderator of the sleep and cognition relationship in middle-aged and older adults: A preliminary investigation. Behavioral sleep medicine. 22(1): 14–27.
- Dzierzewski JM, Dautovich N, Ravyts S (2018) Sleep and Cognition in Older Adults. Sleep Med Clin. 13(1): 93–106.
- Eban-Rothschild A, Appelbaum L, de Lecea L (2018) Neuronal Mechanisms for Sleep/Wake Regulation and Modulatory Drive. Neuropsychopharmacology. 43(5): 937-952.
- Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea - New pathways for targeted therapy. Sleep Med Rev. 37: 45–59.
- Gent TC, Bassetti C, Adamantidis AR (2018) Sleep-wake control and the thalamus. Curr Opin Neurobiol. 52: 188-197.
- Girardeau G, Lopes-Dos-Santos V (2021) Brain neural patterns and the memory function of sleep. Science. 374(6567): 560 - 564.
- Gosseries O, Schnakers C, Laureys S (2019) Between Theory and Clinic: The Contribution of Neuroimaging in the Field of Consciousness Disorders. Front Neurol. 10: 165.
- Hammond D (2019) The legacy of Ludwig von Bertalanffy and its relevance for our time. Systems Research and Behavioral Science.36(3): 301-307.
- He C, Chikara RK, Yeh CL, Ko LW (2021) Neural dynamics of target detection via wireless EEG in embodied cognition. Sensors. 21(15): 5213.
- Jun WH, Kim HJ, Hong YS (2022) Sleep Pattern Analysis in Unconstrained and Unconscious State. Sensors (Basel). 22(23): 9296.
- Langille JJ, Brown RE (2018) The Synaptic Theory of Memory: A Historical Survey and Reconciliation of Recent Opposition. Frontiers In Systems Neuroscience. 12: 52.
- Linhartová P, Látalová A, Kóša B, Kašpárek T, Schmahl C, et al. (2019) fMRI neurofeedback in emotion regulation: A literature review. NeuroImage. 193: 75-92.
- Liu TZ, Xu C, Rota M, Cai H, Zhang C, et al. (2017) Sleep duration and risk of all-cause mortality : a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. 32: 28-36.
- Luppi PH, Fort P (2019) Sleep-wake physiology. Handbook of Clinical Neurology. 160: 359–370.
- Peplow M (2013) Structure: The anatomy of sleep. Nature: 497(7450): S2–S3.
- Philip J, Cherian V (2020) Validity of the biopsychosocial model in contemporary psychiatry. Annals of Indian Psychiatry. 4(2): 219 - 222.
- Pinel, J. P. J., Barnes, S. (2021). Biopsychology. Brazil: Pearson.
- Rezaei M, Mohammadi H, Khazaie H (2017) EEG/EOG/EMG data from a cross sectional study on psychophysiological insomnia and normal sleep subjects. Data in brief. 15: 314–319.
- Saxena A, Paredes-Echeverri S, Michaelis R, Popkirov S, Perez DL (2022) Using the Biopsychosocial Model to Guide Patient- Centered Neurological Treatments. Seminars in neurology. 42(2): 80-87.
- Scarinci F, Patacchioli FR, Parravano M (2021) Exploring the Biopsychosocial Pathways Shared by Obstructive Sleep Apnea (OSA) and Central Serous Chorioretinopathy (CSC): A Literature Overview. Journal of Clinical Medicine. 10(7): 1521.
- Schillmeier M (2019) Thinking with the living body: The Biopsychosocial Model and The Cosmopolitics Of Existence. Medical Humanities, 45(2): 141 - 151.
- Schwartz MD, Kilduff TS (2015) The Neurobiology of Sleep and Wakefulness. The Psychiatric Clinics of North America. 38(4): 615–44.
- Siddarth P, Thana-Udom K, Ojha R, Merrill D, Dzierzewski JM, et al. (2021) Sleep quality, neurocognitive performance, and memory self-appraisal in middle-aged and older adults with memory complaints. International psychogeriatrics. 33(7): 703–713.
- Singh J, Badr MS, Diebert W, Epstein L, Hwang D, et al. (2015) American Academy of Sleep Medicine (AASM) Position Paper for the Use of Telemedicine for the Diagnosis and Treatment of Sleep Disorders. Journal of Clinical Sleep Medicine, 11(10): 1187–98.
- Sinnott-Armstrong W, Summers J (2020) Which biopsychosocial view of mental illness. 82–C6.
- Song Y, Campbell LM, Moore RC (2021) Future directions for sleep and cognition research in at-risk older adults. International psychogeriatrics. 33(7): 655–658.
- St. Louis EK, Frey LC, Britton JW, Frey LC, Hopp JL, et al. (2016) Electroencephalography (EEG): An Introductory Text and Atlas of Normal and Abnormal Findings in Adults, Children, and Infants. American Epilepsy Society.
- Stefani A, Heidbreder A, Brandauer E, Guaita M, Neier LM, et al. (2018) Screening for idiopathic REM sleep behavior disorder: usefulness of actigraphy. Sleep. 41(6): zsy053.
- Thair H, Holloway AL, Newport R, Smith AD (2017) Transcranial Direct Current Stimulation (tDCS): A Beginner's Guide for Design and Implementation. Frontiers in neuroscience. 11: 641.
- Tramonti F, Giorgi F, Fanali A (2019) General system theory as a framework for biopsychosocial research and practice in mental health. Systems Research and Behavioral Science. 36(3): 332- 341.
- van der Zweerde T, Bisdounis L, Kyle SD, Lancee J, van Straten A (2019) Cognitive behavioral therapy for insomnia: A meta- analysis of long-term effects in controlled studies. Sleep medicine reviews. 48: 101208.