Dr. M. Amri*, Dr. S. Anwar, Dr. B. Abdalani, Pr. M. Bouziane, Pr. G. Bennouna, Pr. R. Habbal
Cardiology Department, CHU Ibn Rochd, Casablanca
*Corresponding Author: Dr. M. Amri, Cardiology Department, CHU Ibn Rochd, Casablanca.
Abstract
We present the case of a 68-year-old man who arrived at the emergency department with acute thoracic pain and respiratory distress. Initial clinical examination revealed hypertension, tachycardia, and mild hypoxemia. Chest CT angiography demonstrated a Type B aortic dissection with retrograde extension to the left subclavian artery and thrombosis of the left renal artery originating from the false lumen. This rare combination led to impaired renal perfusion and subsequent nephrotic syndrome, presenting as mild renal dysfunction and low-volume bilateral pleural effusions. Management involved stabilizing the patient with intravenous antihypertensive medications and initiating anticoagulation therapy. Due to the complexity of the case, a multidisciplinary team, including cardiothoracic surgeons and vascular specialists, was consulted. The patient subsequently underwent successful surgical intervention to repair the aortic dissection and manage the renal artery thrombosis. This case underscores the importance of timely diagnosis and a comprehensive multidisciplinary approach in managing complex aortic dissection cases with rare complications, such as renal artery thrombosis, to improve patient outcomes.
Keywords: Aortic dissection, Type B, retrograde extension, renal artery thrombosis
Introduction
Aortic dissection is a critical condition characterized by a tear in the aortic wall that creates a false lumen for blood flow. This condition can lead to severe complications depending on its location and progression [1].
Type B aortic dissection, as classified by the Stanford system, occurs beyond the left subclavian artery and primarily affects the descending aorta [2]. Complications such as retrograde extension to the left subclavian artery and renal artery thrombosis can complicate the management of Type B dissection [3]. The retrograde extension involves the dissection moving back towards the aortic arch, potentially impacting vital branches. [4] Renal artery thrombosis, arising from the false lumen, can result in impaired kidney function and other systemic issues [5].
This report discusses a case of Type B aortic dissection with retrograde extension and associated renal artery thrombosis, highlighting the challenges in diagnosis and management.
Case Presentation
A 68-year-old male patient with a medical history of hypertension and cardiovascular disease presented to the emergency department with acute thoracic pain and difficulty breathing. On examination, his blood pressure was 160/100 mmHg, heart rate was 95 beats per minute, respiratory rate was 20 breaths per minute, and temperature was 37.2°C. His oxygen saturation was 93% on room air. A cardiovascular examination revealed regular heart sounds without any notable murmurs. Respiratory examination showed bilateral basal crackles, and there was mild tenderness in the left lumbar region upon abdominal examination.
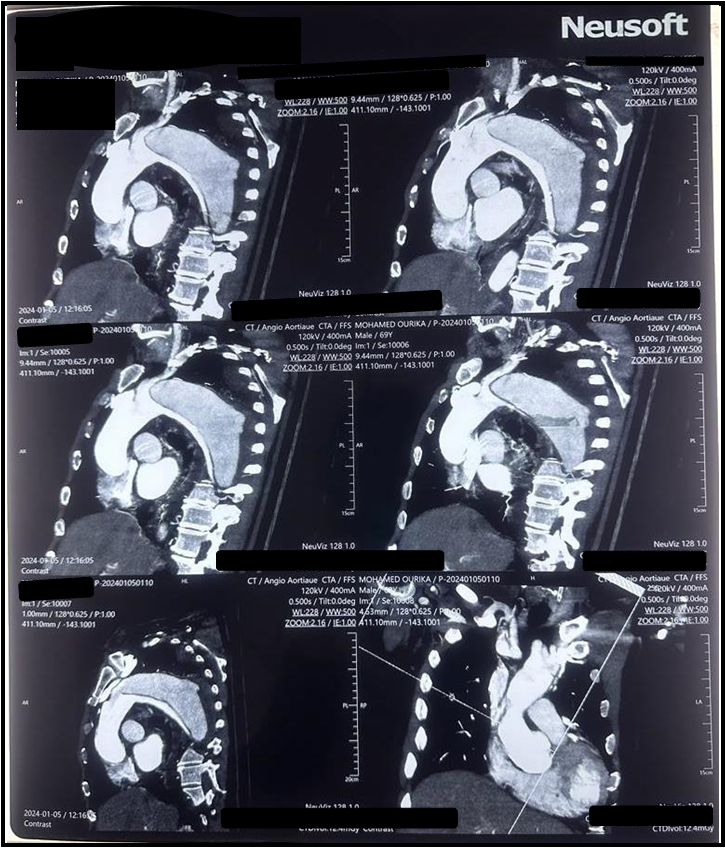
Chest CT angiography revealed a Type B aortic dissection with retrograde extension to the left subclavian artery. (Figure 1) There was also thrombosis of the left renal artery originating from the false lumen, which was associated with a nephrotic kidney. Additionally, low-volume bilateral pleural effusions were observed.
The patient was stabilized initially with intravenous antihypertensive therapy, including labetalol and nitroprusside, to control blood pressure and reduce stress on the aortic wall. Anticoagulation therapy with heparin was initiated to manage the renal artery thrombosis. Given the complexity of the dissection and the associated renal complications, a multidisciplinary team, including cardiothoracic surgeons and vascular specialists, was consulted.
Surgical intervention involved an open surgical repair of the aortic dissection. The procedure included the resection of the affected segment of the aorta and reconstruction using a synthetic graft. Additionally, the left renal artery thrombosis was addressed through thrombectomy and stenting to restore adequate blood flow to the kidney. The surgery aimed to repair the dissection, prevent further retrograde extension, and manage renal perfusion issues.
Postoperatively, the patient was closely monitored in the intensive care unit. His antihypertensive regimen was continued with oral medications, including angiotensin-converting enzyme (ACE) inhibitors and beta-blockers, to maintain blood pressure control. Anticoagulation therapy was adjusted as per the patient’s renal function and response. The patient’s recovery was closely followed, with improvement in his symptoms and resolution of the pleural effusions. The surgical and medical interventions effectively managed the complex dissection and associated renal complication.
Figure 1: Thoracic CT scan showing type B dissection
Discussion
This case underscores several critical aspects of managing Type B aortic dissection, particularly with complications such as retrograde extension and renal artery thrombosis.
Type B aortic dissection, as classified by the Stanford system, involves the descending aorta and is associated with a high risk of complications, particularly when there is a retrograde extension. Retrograde extension can lead to the involvement of branch vessels, such as the left subclavian artery, complicating the clinical management and increasing the risk of adverse outcomes, including end-organ ischemia and mortality [6].
In this case, the retrograde extension to the left subclavian artery presented diagnostic and therapeutic challenges. This phenomenon is significant as it may lead to compromised blood flow to critical branches and can exacerbate symptoms or contribute to further systemic complications [7]. The identification of retrograde extension through imaging is essential for guiding appropriate management strategies and for planning possible surgical interventions.
Additionally, the presence of renal artery thrombosis originating from the false lumen adds another layer of complexity. Renal artery thrombosis can result in renal ischemia, elevated blood pressure, and worsening renal function, which necessitates prompt intervention. The management of renal artery thrombosis involves anticoagulation therapy to prevent further thrombus formation and, in some cases, surgical intervention to restore adequate renal perfusion [8].
The successful management of this case highlights the importance of a multidisciplinary approach, including the use of antihypertensive medications to control blood pressure and reduce stress on the aortic wall, along with anticoagulation to address thrombotic complications. Surgical repair of the aortic dissection and renal artery thrombosis, as performed in this case, remains a critical component of treatment for complex dissections [9].
This case reinforces the need for clinicians to remain vigilant for complications associated with Type B aortic dissection. Early diagnosis, comprehensive management, and appropriate surgical intervention are essential for improving patient outcomes and reducing the risk of serious complications.
Conclusion
Type B aortic dissection with retrograde extension and associated renal artery thrombosis presents considerable diagnostic and management challenges. The complexity of this condition necessitates a thorough and timely diagnostic approach to identify complications such as retrograde extension and renal artery involvement. Effective management requires a multidisciplinary approach, incorporating both medical and surgical strategies to address the diverse aspects of the dissection and its complications. Prompt and coordinated intervention is crucial for optimizing patient outcomes, reducing the risk of severe complications, and improving overall prognosis. This case highlights the importance of early recognition and comprehensive treatment strategies in managing complex aortic dissection cases and underscores the need for ongoing vigilance and expertise in handling such critical conditions.
Patient consent was obtained prior to the study. Conflict of Interest: None.
Acknowledgments: None.
References
- Ince H, Nienaber CA (2007) Diagnosis and management of patients with aortic dissection. Heart. 93(2): 266-70.
- Yuan X, Mitsis A, Nienaber CA (2022) Current Understanding of Aortic Dissection. Life (Basel). 12(10): 1606.
- Eidt JF, Vasquez J (2023) Changing Management of Type B Aortic Dissections. Methodist Debakey Cardiovasc J. 19(2): 59- 69.
- Nauta FJ, Tolenaar JL, Patel HJ, Appoo JJ, Tsai TT, et al. (2016) International Registry of Acute Aortic Dissection (IRAD) Investigators. Impact of Retrograde Arch Extension in Acute Type B Aortic Dissection on Management and Outcomes. Ann Thorac Surg. 102(6): 2036-2043.
- Li A, Mohetaer D, Zhao Q, Ma X, Ma Y (2019) The Relationship Between Renal Artery Involvement in Stanford B-Type Aortic Dissection and the Short-Term Prognosis: A Single-Centre Retrospective Cohort Study. Heart Lung Circ. 28(8): 1261-1266.
- Nienaber CA, Clough RE (2015) Management of acute aortic dissection. Lancet. 385(9970): 800-11.
- Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, et al. (2000) The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 283(7): 897-903.
- Goodyear WE, Beard DE (1947) Diagnosis and management of renal-artery thrombosis; report of a case. N Engl J Med. 237(10): 355-8.
- Mazzolai L, Teixido-Tura G, Lanzi S, Boc V, Bossone E, et al. (2024) 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 30: ehae179.