T. A. Solile*, B.T. Haonga
Department of Orthopaedics and Traumatology, School of medicine, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
*Corresponding Author: T. A. Solile, Department of Orthopaedics and Traumatology, School of medicine, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Abstract
Background
The evolution of treatment concepts regarding Pertrochanteric fractures is critical to advancing our treatment modalities. The SIGN Hip Construct (SHC) is an intramedullary device that treats stable and unstable intertrochanteric fractures in low and middle-income countries. The goal of this implant design was to enable operative stabilization of all intertrochanteric fractures without the aid of C-arm imaging in resource-limited countries. HV plates are used with standard or SHC hip nails whenever the fracture involves the greater trochanter, especially in highly unstable multifragmentary fractures (31A2 and 31A3). The study aimed to compare treatment outcomes of Trochanteric fractures treated by SIGN Hip Construct (SHC) with versus without High Versatility (HV) plate at Muhimbili Orthopaedic Institute (MOI).
Methods
A cohort prospective study looking into treatment outcomes of patients (18 years and above) with trochanteric fractures treated by SHC with an HV plate versus no HV plate at MOI. Patients were grouped into two groups (i.e., those treated by SHC with an HV Plate and those without an HV plate). Patients were operated on by senior orthopedics surgeons. The general criteria for applying HV plate with SHC was the presence of proximal femur lateral wall disruption. During admission, patients were examined, an Anteroposterior (AP) X-ray of the pelvis was taken, and the Singh index was used to evaluate the degree of osteoporosis. Immediately after surgery, the patients were assessed for any limb length discrepancy, malrotation, and adequacy of reduction. The follow-up intervals were 2 weeks, 6 weeks, and 12 weeks. In follow-up visits, the state of the wound, callus formation, varus deformity, and length discrepancy were assessed. Data analysis was managed by statistical software (SPSS version 20).
Results
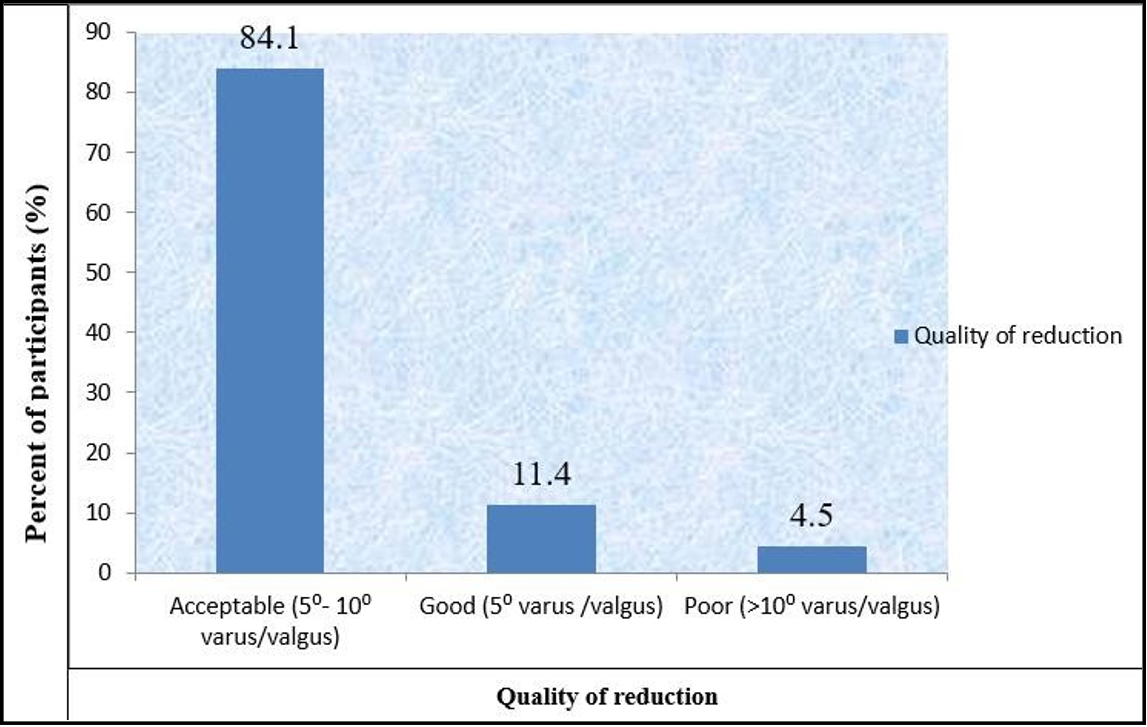
Forty-five patients were enrolled in the study. Thirty-one patients were in SHC without the HV plate group, and 14 were in SHC with the HV plate group. Of the enrolled patients, 31.1% (n=14) of study participants were aged 55-64 years with a mean age of 68 ±15.6 yrs. Males were 60% (n=27). Thirty participants (66.7%) had trochanteric fractures caused by falls from standing height, and two patients (4.4%) were caused by falls from height. The reduction quality was as follows: 11.4% had a sound reduction, 84.1% had an acceptable reduction, and only 4.5% had a poor reduction.
Varus collapse was statistically significant between the cohort groups. In the 12th week, varus failure of 5⁰-10⁰ was observed in 64.3% of patients treated with SHC with an HV plate, while 96.8% of patients treated with SHC only had varus collapse of the same range with a p-value of 0.008. The affected limb length observed was as follows: eighty percent of patients in both groups have limb shortening of (1-2cm). Limb shortening of > 2cm was observed in 3.2% (n=1) in those fixed with SHC only and 7.1% (n=1) in those specified by SHC with HV plates. The observed difference was not statistically significant. (p-value 0.262)
In most participants, >90% of patients had callus formation at 6 weeks in both groups (p-value 0.530).
Out of 45 participants, 12 (26.7%) had osteoporosis of grade 3 by the Singh index. Only one patient (2.2%) had implant loosening and had grade 4 bone density by Singh index. This shows there is no statistical relationship found between osteoporosis and implant loosening (p=0.706), which is against the knowledge that osteoporosis does accelerate implant loosening. This can be explained by the short study time; hence, several implant loosening was observed.
Conclusions
From this study, trochanteric fractures fixed with either SHC only or SHC with an HV plate had no difference in callus formation, limb length discrepancy, and infection. However, there is a statistical difference in varus collapse; patients who had been treated with SHC with an HV plate had less varus collapse compared to those treated with SHC only. Also, varus collapse is associated with unstable fracture patterns, inadequate reduction, and implant choice. In this study, osteoporosis seemed to have no relation with the loosening of the implant/ screw cut out. This can be due to the short time of reflection.
Introduction
Pertrochanteric fractures involve those occurring in the region extending from the extracapsular basilar neck region to the area along the lesser Trochanteric proximal to the development of the medullary canal. Intertrochanteric and Peritrochanteric are generic terms for Pertrochanteric fractures [1].
The incidence of intertrochanteric fractures is increasing. Currently, it is estimated that 250,000 hip fractures occur annually in the United States. Investigators predict the incidence to approach 500,000 by 2040 [2].
In 1990, 26% of all hip fractures in Asia were intertrochanteric fractures, whereas this figure could rise to 37% in 2025 and 45% in 2050 [3].
In Trochanteric fractures, stability refers to the capacity of the internally fixed fracture to resist muscle and gravitational forces around the hip that tend to force the fracture into a varus position. Intrinsic factors like osteoporosis and comminution of the fracture and extrinsic factors like choice of reduction, choice of implant, and technique of insertion contribute to internal fixation failure [4].
Patients and Methods
This was a Cohort prospective study looking into treatment outcomes of patients (aged 18 years and above) with trochanteric fractures treated by SHC with an HV plate versus no HV plate at MOI from May 2017 to April 2018. Patients were grouped into two groups (i.e., those treated by SHC with an HV Plate and those without an HV plate). Patients were operated on by senior orthopedics surgeons. The general criteria for applying HV plate with SHC was the presence of proximal femur lateral wall disruption. During admission, patients were examined, an Anteroposterior (AP) X-ray of the pelvis was taken, and the Singh index was used to evaluate the degree of osteoporosis. Immediately after surgery, the patients were assessed for any limb length discrepancy, malrotation, and adequacy of reduction. Physiotherapy was as follows: non-weight bearing with axillary crutches as soon as tolerable, partial weight bearing at 4 weeks postoperatively, and total weight bearing after the radiological and clinical union. The follow-up intervals were 2 weeks, 6 weeks, and 12 weeks. In follow-up visits, the state of the wound, callus formation, varus deformity, and length discrepancy were assessed. Data analysis was managed by statistical software (SPSS version 20). Ethical issues about informed consent, confidentiality, and the right to withdraw from the study were respected by the researcher.
Results
During the study period, surgery was performed on thirty-one patients with SIGN Hip Construct (SHC) only and fourteen patients by SHC with HV plate. Patients were prospectively followed in the 2nd week, 6th week, and 12th week. Of the enrolled patients, 60% (n=27) were male, and 40% (n=18) were female, with a female ratio of 1.5:1. Age group of the participants was between 32 to 95years. The average age was 68 years, and most participants, 31.1% (n=14), were from 55-64 years. (Table 1).
Table 1: Demographic characteristics of study participants
|
Characteristics |
Study participants |
|
|
N= 45 |
100% |
|
|
Age (yrs) mean ± S.D 68 ±15.6 yrs |
|
|
|
≤54 |
5 |
11.1 |
|
55-64 |
14 |
31.1 |
|
65-74 |
8 |
17.8 |
|
75-84 |
12 |
26.7 |
|
≥85 |
6 |
13.3 |
|
Sex |
|
|
|
Male |
27 |
60 |
|
Female |
18 |
40 |
Table 2: Age versus Varus collapse at 12th weeks among patients fixed with SHC only and with HV plate.
|
Age (yrs) |
Varus collapse |
Total N=45 (100%) |
X2 P value |
||
|
<5⁰ |
5⁰-10⁰ |
>10⁰ |
|||
|
≤54 |
0(0) |
5 (11.5) |
0(0) |
5 (11.1) |
0.183 |
|
55-64 |
2 (4.4) |
12 (26.7) |
0(0) |
14 (31.1) |
|
|
65-74 |
0(0) |
8 (17.9) |
0(0) |
8 (17.8) |
|
|
75-84 |
1 (2.2) |
10 (22.2) |
1 (2.2) |
12 (26.7) |
|
|
≥85 |
0(0) |
4 (8.9) |
2 (4.4) |
6 (13.3) |
|
|
Total |
3 (6.7) |
39 (86.2) |
3 (6.7) |
45 (100) |
|
It is evident from the above table that, at 12 weeks, varus collapse of <5⁰ and 5⁰-10⁰ were found among patients (n=27) aged less than 75 while those aged 75years and above, 15 patients had varus collapse of <5⁰ and 5⁰-10⁰ and 3patients (6.6%) had varus collapse more than 10⁰. The observed difference was not statistically significant (p- value 0.183)
Mechanism of injury in Trochanteric fractures participants.
Thirty participants (66.7%) sustained Trochanteric fractures due to a fall from standing height (trivial injury), 13 (28.9%) patients due to motor traffic crush, and 2 patients (4.4%) due to a fall from height.
A pattern of Trochanteric fractures
AO classification of Trochanteric fractures was used in this study. Fracture patterns 31A1 and 31A2:1 was considered stable, and those with fracture patterns 31A2:2, 31A2:3, and 31A3 were unstable. Twenty-five patients (56.7%) had stable Trochanteric fractures, and 20 patients (43.3%) had erratic fracture patterns.
Approximately sixty-five percent (64.5%, n=20) of stable fractures were treated by SHC only, and 64.3 %( n=9) of unstable fractures were treated by SHC with an HV plate; the observed difference was statistically significant ( P = 0.046) (Table 3)
All patients with stable fracture patterns had good/acceptable reduction, while those who had unstable fracture patterns, about 4.6 % (n=2), had poor reduction. (Table 4)
Also, all patients with stable fractures had varus collapse less than 10⁰ while those with unstable fracture pattern 17 had varus collapse less than 10⁰, and 3 patients had varus collapse more than 10⁰ (Table 4).
Table 3: Comparison of stability of fracture versus treatment done (SHC only and SHC with HV Plate)
|
Stability of fracture |
Treatment done |
P value |
|
|
SHC only |
SHC with HV Plate |
||
|
Stable |
20 (64.5%) |
5 (35.7%) |
0.046 |
|
Unstable |
11 (35.5%) |
9 (64.3%) |
|
|
Total |
31 (100%) |
14 (100%) |
|
Table 3: AO classification of Trochanteric fracture versus quality of reduction
|
AO Classification |
Quality of reduction |
Total |
X2 p value |
||
|
Good |
Acceptable |
Poor |
|||
|
31A1.1 |
2 (4.4) |
2 (4.4) |
0(0) |
4 (8.9) |
0.004 |
|
31A1.2 |
0(0) |
8 (18.2) |
0(0) |
8 (18.2) |
|
|
31A1.3 |
0(0) |
9 (20.5) |
0(0) |
9 (20.5) |
|
|
31A2.1 |
1 (2.3) |
3 (6.8) |
0(0) |
4 (9.1) |
|
|
31A2.2 |
1 (2.3) |
4 (9.1) |
0(0) |
5 (11.4) |
|
|
31A2.3 |
2 (4.4) |
9 (20.0) |
1 (2.3) |
12 (26.7) |
|
|
31A3.1 |
0(0) |
2 (4.5) |
0(0) |
2 (4.5) |
|
|
31A3.2 |
0(0) |
0(0) |
1 (2.3) |
1 (2.3) |
|
|
Total |
6 (11.4) |
37 (84.1) |
2 (4.5) |
45 (100) |
|
Table 4: Varus collapse at 12th weeks versus AO classification of Trochanteric fracture, quality of reduction and Singh osteoporosis index.
|
|
Varus collapse |
Total |
X2 p value |
||
|
<5⁰ |
5-10⁰ |
>10⁰ |
|||
|
AO Classification |
|
|
|
|
|
|
31A1.1 |
0(0) |
4 (8.9) |
0 (0) |
4 (8.9) |
0.010 |
|
31A1.2 |
0(0) |
8 (17.8) |
0(0) |
8 (17.8) |
|
|
31A1.3 |
0(0) |
9 (20) |
0(0) |
9 (20) |
|
|
31A2.1 |
0(0) |
4 (8.9) |
0(0) |
4 (8.9) |
|
|
31A2.2 |
2 (4.4) |
3 (6.7) |
0(0) |
5 (11.1) |
|
|
31A2.3 |
1 (2.2) |
9 (20) |
2 (4.4) |
12 (26.7) |
|
|
31A3.1 |
0(0) |
2 (4.4) |
0(0) |
2 (4.4) |
|
|
31A3.2 |
0(0) |
0(0) |
1 (2.2) |
1 (2.2) |
|
|
Quality of reduction |
|
|
|
|
0.001 |
|
Good |
2 (4.4) |
4 (8.9) |
0(0) |
6 (13.3) |
|
|
Acceptable |
1 (2.2) |
35 (77.8) |
1 (2.2) |
37 (82.2) |
|
|
Poor |
0(0) |
0(0) |
2 (4.4) |
2 (4.4) |
|
|
Singh Osteoporosis index |
|
|
|
|
|
|
Grade 1 |
0(0) |
0(0) |
0(0) |
0(0) |
0.551 |
|
Grade 2 |
0(0) |
0(0) |
0(0) |
0(0) |
|
|
Grade 3 |
0(0) |
11 (24.4) |
1(2.2) |
12 (26.7) |
|
|
Grade 4 |
2 (4.4) |
15 (33.3) |
2 (4.4) |
19 (42.2) |
|
|
Grade 5 |
1 (2.2) |
4 (8.9) |
0 (0) |
5 (11.1) |
|
|
Grade 6 |
0(0) |
9 (20) |
0(0) |
9 (20) |
|
|
It is clear from above table that, 4.4% of patients with fracture class 31A2.2 have varus collapse of <5⁰, varus collapse of 5⁰-10⁰ was observed in 20% of patients with fracture class 31A1.3 and 31A2.3, varus collapse of >10⁰ was observed in 4.4% of patient with fracture class 31A2.3. Varus collapse of >10⁰ was observed in 4.4% of patients with poor reduction. Varus collapse of 5-10⁰ was observed in 33.3% of patients with Grade 4 Singh index and varus collapse of >10⁰ were observed in three patients (two in grade 4 and one in grade 3). |
|||||
Quality of reduction among participants with Trochanteric fractures.
All participants recruited in this study were immediately taken to do a control anteroposterior pelvic x-ray and full-length femur x-ray post-operative. The reduction status was assessed radiologically and documented. Among 45participants, 84.1% had acceptable reduction (i.e., 5⁰- 10⁰ varus/valgus), 11.4% had sound reduction (<5⁰varus/valgus), and only 4.5% had poor reduction (>10⁰ varus/valgus) (Figure 1).
Varus collapse of >10⁰ was observed in 4.4% of patient with poor reduction (Table 5).
Figure 1: Quality of reduction among participants with Trochanteric fractures.
Varus collapse and limb length measurements.
Table 6 shows that at 12th week varus collapse was significant between the two groups (i.e there were 64.3% of patients with varus collapse of 5⁰-10⁰ in patients treated with SHC with HV plate while 96.8% of patients treated with SHC only had varus collapse of same range were observed. This was statistically significant with p value of 0.008.
Majority of patients (>80%) in both groups have limb shortening of 1-2cm. Limb shortening of > 2cm was observed in 3.2% in those with SHC only and 7.1% in those with SHC with HV plate.
Table 5: Varus collapse, callus formation on control X- ray of Pelvic and affected limb length.
|
|
SHC only n =31 (100%) |
SHC with HV plate n= 14 (100%) |
Total N=45 (100%) |
X2 p value |
|
Varus collapse |
|
|
|
|
|
6th week |
|
|
|
<0.001 |
|
<5⁰ |
0 (0) |
5 (35.7) |
5 (11.1) |
|
|
5⁰-10⁰ |
30 (96.8) |
7 (50) |
37 (82.2) |
|
|
>10⁰ |
1 (3.2) |
2 (14.3) |
3 (6.7) |
|
|
12th week |
|
|
|
0.008 |
|
<5⁰ |
0(0) |
3 (21.4) |
3 (6.7) |
|
|
5⁰-10⁰ |
30 (96.8) |
9 (64.3) |
39 (86.7) |
|
|
>10⁰ |
1 (3.2) |
2 (14.0) |
3 (6.7) |
|
|
Affected limb length |
|
|||
|
Normal length |
0 (0) |
1 (7.1) |
1 (2.2) |
0.262 |
|
Shortening (1-2cm) |
30 (96.8) |
12 (85.7) |
42 (93.3) |
|
|
Shortening (>2cm) |
1 (3.2) |
1 (7.1) |
2 (4.4) |
|
|
Callus formation |
|
|
|
0.530 |
|
Present |
30 (96.8) |
13 (92.9) |
|
|
|
Absent |
1 (3.2) |
1 (7.1) |
|
|
Pre-operative x-ray.
Immediately post-operative x-ray.
12th week post operative x-ray.
Figure 2: Pre- and post-operative radiograph of stable intertrochanteric fracture.
Pre-operative x-ray
Immediately post-operative
12th week post-operative
Figure 3: Pre and post-operative radiograph of unstable Trochanteric fracture.
Infection.
In all study groups there were no infections that occurred to participants during the study period.
Implant loosening in relation to the degree of osteoporosis.
Out of 45 participants, 12 (26.7%) had osteoporosis of grade 3 by Singh index.
Only one patient (2.2%) had implant loosening and had grade 4 bone density by Singh index. (Table 7)
Table 6: Implant loosening in relation to osteoporosis.
|
Bone Density by Singh index |
Loosening of implant |
Total |
X2 p value |
|
|
|
Present |
Absent |
|
0.706 |
|
Grade 3 |
0(0) |
12 (26.7) |
12 (26.7) |
|
|
Grade 4 |
1 (2.2) |
18 (40.0) |
19 (42.2) |
|
|
Grade 5 |
0 (0) |
5 (11.1) |
5 (11.1) |
|
|
Grade 6 |
0(0) |
9 (20.0) |
9 (20.0) |
|
|
Total |
1 (2.2) |
44 (97.8) |
45 (100) |
|
Discussion
Peritrochanteric fractures of the femur have consistently been recognized as a significant challenge by the orthopedics community, not only for achieving fracture union but also for restoration of optimal function in the shortest possible time and with minimal complications. [4]
This study reports the outcome of 45 patients with Trochanteric fractures fixed with SHC only versus SHC with an HV plate. Thirty-one- patients were treated with SHC only, and 14 patients by using SHC with an HV plate.
In this study, the majority of patients were male, 60% (n=27) and 40% (n=18) female, with male to female ratio of 1.5:1. Age group of the participants was between 32 to 95years. The average age was 68 years, and most participants were 55-64 years old. These results show that Trochanteric fractures are common in the elderly population. These were comparable with other studies [9,13,14].
The most common mechanism of injury was fall from standing height (i.e., trivial damage) (67%) in the elderly. In the young age group, fracture was due to motor traffic crush. This can be explained by the poor bone density in older people. These findings are similar to observations in other studies [3,6].
AO classification of Trochanteric fracture was used. Twenty-five patients (56.7%) had stable Trochanteric fractures, and 20 patients (43.3%) had unstable fracture patterns. This is comparable with other studies [6,13]. Approximately sixty-five percent ( 64.5%, n=20) of stable fractures were treated by SHC only, and 64.3%(n=9) of unstable fractures were treated by SHC with an HV plate; this explains that unstable fractures that involve the lateral wall of the proximal part of femur do not have any lateral osseous buttress hence they need a buttress such as HV plate to increase stability. All patients with stable fracture patterns had good/acceptable reduction, while those who had unstable fracture patterns, about 4.6 % (n=2), had poor reduction. The difference in reduction quality was statistically significant (p = 0.004). (Table 4)
Also, all patients with stable fractures had varus collapse less than 10⁰ while those with unstable fracture pattern 17 had varus collapse less than 10⁰, and 3 patients had varus collapse more than 10⁰. This observation was statistically significant (p= 0.010) (Table 5).
Achieving adequate reduction is vital in attaining good outcomes. In this study, about 11.4% had a sound reduction, 84.1% had an acceptable reduction, and only 4.5 % had a poor reduction. Nearly equivalent results were obtained by Justin R. et al., who reported that the quality reduction of good/acceptable was 76% and poor was 24% [15].
However, the reduction quality was higher in this study, i.e., good/acceptable was 95.5%. Figure 2 shows the preoperative and postoperative radiographs of one participant who had a stable fracture pattern, and reduction was adequate.
Varus collapse was statistically significant between the cohort groups. In the 12th week, the varus collapse of 5⁰-10⁰ was observed in 64.3% of patients treated with SHC with an HV plate, while 96.8% of patients treated with SHC only had varus collapse of the same range. This was statistically significant, with a value of 0.008 (Table 6). This observation shows that the addition of an HV plate on SHC has the impact of decreasing the varus collapse deformity. This might be due to the solid stability of fixation of the SHC with the HV plate.
Varus collapse of 5-10⁰ was observed in 33.3% of patients with Grade 4 Singh index, and varus collapse of >10⁰ was observed in three patients (two in grade 4 and one in grade 3). The observed difference was not statistically significant (p=0.551). (Table 5)
Most participants (>80%) in both groups have limb shortening of 1- 2cm. Limb shortening of > 2cm was observed in 3.2% (n=1)in those fixed with SHC only and 7.1%(n=1) in those specified by SHC with HV plates. The observed difference was not statistically significant (p-value 0.262).
In most participants, >90% of patients had callus formation at 6 weeks in both groups (i.e., SHC only and those fixed by SHC with HV plate). There is no statistically significant difference in callus formation among the two groups (p-value 0.530).
Out of 45 participants, 12 (26.7%) had osteoporosis of grade 3 by the Singh index. Only one patient (2.2%) with Singh index grade 4 had implant loosening. This shows there is no statistical relationship found between osteoporosis and implant loosening (p=0.706), which is against the knowledge that osteoporosis does accelerate implant loosening. This can be explained by the short time of the study; hence, several implant loosening was observed.
In this study, implant loosening occurred in one patient with an unstable fracture pattern and inadequate reduction; Figure 3 shows preoperative and postoperative radiographs with screw cut out/implant loosening.
Conclusions
Trochanteric fractures fixed with either SHC only or SHC with an HV plate had no difference in callus formation, limb length discrepancy, or infection. However, there is a statistical difference in varus collapse among the cohort groups. Patients who had been treated by SHC with an HV plate had less varus collapse compared to those treated with SHC only.
Varus collapse is associated with unstable fracture patterns, inadequate reduction, and implant choice.
In this study, osteoporosis seemed to have no relation with the loosening of the implant/ screw cut out; this can be due to short study duration.
Acknowledgments
I wish to express my sincere gratitude to my supervisor, Dr. Billy Haonga, Dr. Goodluck R. Maro, for statistical support and to all members of staff in the Department of Orthopaedic and Traumatology MUHAS and MOI for their input during the development, patient follow-up and analysis of this research. Lastly, my appreciation goes to the MOI administrative department for permission to conduct this study.
References
- Charles M, Jamesn D, Margaret M, William M PT (2015) Rockwood and Green’s Fractures in Aldults,8th Edition. 2075- 2126 p.
- Browner B, JupiterJ, Levine A, Trafton P KC (2009) Browner : Skeletal Trauma , 4th ed . Chapter 49 – Intertrochanteric. 1987- 1988 p.
- Jonnes C, Sm S, Najimudeen S (2016) Type II Intertrochanteric Fractures : Proximal Femoral Nailing versus Dynamic Hip Screw. Arch Bone Jt Surgery. 4(1): 23–28.
- Sinha U, Ishtiaque S (2016) A Randomized Comparative Study On Functional Outcome Of Pertrochanteric Femoral Fractures Treated With A Dynamic Hip Screw Or A Proximal Femoral Nail. IOSR J Dent Med Sci. 15(4): 5–21.
- Justin R, Shearer D, Zirkle LG, Johnson A, Labarre P (2009) Development and Biomechanical Testing of the SIGN Hip Construct. Tech Orthop. 24(4): 265–272.
- Haonga BT, Eliezer EN, Makupa JE, Shearer D, Liu MB, et al. (2016) SIGN Hip Construct: Achieving Hip fracture Fixation without using an image intensifier. East African Orthopaeic J. 10(1): 7–10.
- Lorich DG, Geller DS, Nielson JH (2004) Osteoporotic Pertrochanteric Hip Fractures. Instr Course Lect. 53: 441-54.
- Heckman JD (2008) Campbell’s Operative Orthopaedics. 11th ed. Vol. 90, J Bone Joint Surg Am. 2008. 943-944 p.
- Nargesh A, Ashok T, Muhammad S MA (2013) Comparative study of the management of inter-trochanteric fractures in the elderly : short proximal femoral nail vs dynamic hip screw. Sri Lanka J Surg. 30(2):13–7.
- Rüedi TP, Murphy WM, Colton CL, Fernandez A, Oca D, et al. (2001) AO Principles of Fracture Management. October. 445- 448.
- Haidukewych GJ (2009) Intertrochanteric Fractures : Ten Tips to Improve Results. J Bone Jt Surg Am. 91(3): 712–9.
- Jhamnani R, Ronald JM, Harsharaj K (2015) Functional Outcome of Comminuted Intertrochanteric Fracture of Femur Internally Fixed Using Proximal Femoral Nail. I nternational J Heal Sci. 3(1): 417–425.
- Endigeri P, Pattanashetty O, Banapatti D, Pillai A, Ullas T (2015) Outcome of intertrochanteric fractures treated with proximal femoral nail: A prospective study. J Orthop Traumatol Rehabil. 8(1): 25–9.
- Kenyunko KM (2013) Profile of Trochanteric Fractures at MOI: Treatment and Short-term outcome 2012.
- Justin R, Brian G, John S, Zirkle L Dave S (2009) Early Clinical Experience with the SHC. Tech Orthop. 24: 265–272.
- Akan K, Cift H, Ozkan K, Eceviz E, Tasyikan L, et al. (2011) Effect of Osteoporosis on Clinical Outcomes in Intertrochanteric Hip Fractures Treated with a Proximal Femoral Nail. J Int Med Res. 39(3): 857–65.
- Reider B (2023) The Orthopedic Physical Examination, 2nd edition.
- Das S (2000) A manual in clinical surgery icluding special investigation and differencial diagnosis- 5th Edition. chapter 13: 147-52.
- McRae R (2006) Pocketbook of orthopaedics and fractures Second edition; Chapter 9: 116-9.