Zahoor Ahmed1*, Amr Mohamed Abdelsalam Elmahdy2, Syed Nabir3, Umais Momin4, Mohamed Nadeem Ahmed5, Usman Nabi6
1Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0001-9486-7526 2Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0001-7944-1527 3Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0001-8092-9757 4Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0003-3336-8648 5Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0003-4797-8420 6Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0001-6896-7646
*Corresponding Author: Zahoor Ahmed, Clinical Imaging Department, Hamad General Hospital, P.O. Box 3050, Doha, Qatar. https://orcid.org/0000-0001-9486-7526.
Abstract
Aim: Early diagnosis of the extent and severity of injury in Priority-1 trauma patients can not only be a life saver but also aid in delivery of prompt and effective definitive care, thereby significantly reducing the patient morbidity. The aim of our study was to improve the average time for vetting Pan CT scan requests of Priority-1 trauma Patients.
Methods:
Retrospective analysis of vetting time by the Emergency radiologists in the preceding six months was undertaken to determine the mean baseline vetting time. A cause-effect analysis was undertaken to study the potential causes contributing to the delay in vetting. A monitoring tool was devised and incorporated into the system to minimize the vetting time. Results from implementation were sequentially tracked over the 2-month prospective study duration.
Results: The study achieved 30.3% decrease in vetting time, from a mean baseline duration of 14.93 minutes to a mean post implementation duration of 10.4 minutes.
Conclusion: A simple yet effective monitoring tool with special emphasis on active and prompt communication between the Trauma team and the Emergency radiology team can be a crucial cog in the wheel to significantly reduce the vetting time in any hospital that caters to trauma patients.
Introduction
Time is of the utmost essence in the care of severely traumatized patients and the ‘Golden hour’ is a well-established concept in their management. It refers to the first 60 minutes after a traumatic event within which the patient requires to receive definitive care, after which morbidity and mortality increase significantly [1,2].
After the preliminary in-hospital care of stabilizing the severely traumatized patients as per the Advanced Trauma Life Support (ATLS) guidelines, the definitive care commences with a rapid radiological diagnosis of the extent and severity of the injury, rigorous injury assessment, and defining a therapeutic strategy [3,4]. Every precious minute delayed in this process could have serious detrimental consequences including prolonged hospitalization, debility, and even loss of life.
CT scan is an indispensable component in the evaluation of trauma patients, especially those who are hemodynamically stable [5].
Radiological assessment of a patient in the Trauma and Emergency department begins with an electronic order/ request for a CT scan, replete with the patient history, clinical data, and the desired investigation. In a regular shift, the on-call radiologist is inundated with numerous requests for imaging and has to undertake the process of vetting these requests. Vetting enables the radiologist to either approve, reject or refer the imaging request for a discussion.
The Ionising Radiation (Medical Exposure) Regulations 2017 (IR(ME)R)1, imposes responsibility upon the Clinical Imaging Department to justify all examinations using ionizing radiation, but all imaging examinations require vetting to ensure the request is appropriate for the clinical question and the individual patient. Vetting is a triaging process of the imaging requests that are required to justify the investigation e.g., appropriate use of imaging modalities, radiation safety, and judicious use of resources. Vetting also serves to authorize the request, once justified, and will enable exam protocolling, especially for cross-sectional imaging [6]. This is essential to ensure compliance with the IR(ME)R1.
In a typical Clinical Imaging setup, the reporting radiologist is required to vet the imaging requests simultaneously whilst involved in reporting and discharging other administrative duties in the department. Vetting in itself is a time-consuming process that requires the radiologist to review the clinical records, past medical history, prior investigations if available, etc. to arrive at a decision. All these factors may contribute to a potential delay in vetting and approving the imaging requests, which in the case of patients with severe trauma may impede timely dispensation of medical care. Hence there is a pressing requirement to expedite the vetting process of patients with Priority-1 trauma.
In the busy environment of the emergency setting for emergency radiologists, trauma surgeons, and emergency physicians, every care should be taken to ensure that the medical service delivered to Priority-1 trauma cases is efficient and on time; to reduce harm and achieve maximal patient safety.
According to the Royal College of Radiology (RCR) “Standards of Practice and Guidance for Trauma Radiology in Severely Injured Patients”, there are 18 standards required to achieve this goal [7]. Standard number “7” highlights the need of existence for clear protocols notifying the CT department of the need for urgent imaging and how the department will respond. It must be clear who is responsible for that at both ends.
In line with one of the RESPECT core values of our corporation which is Teamwork [8], and with the International Patient Safety Goals (IPSGs) set by Joint Commission International (J.C.I.) [9] to improve effective communication, the need for the development of a proper communication tool to hand off these cases is crucial. This will ensure the achievement of the shared corporate vision to deliver the safest, most effective, and most compassionate care to every patient [10].
Materials and Methods
This study was undertaken at the Emergency Radiology Department of a tertiary care hospital. This 603-bedded facility has a highly specialized Emergency and Trauma Department which provides primary treatment to patients suffering from life-threatening illnesses and injuries. The division of Emergency Radiology has consultants with expertise in a full range of diagnostic imaging like CT, MR, ultrasound, and radiography.
This study was approved by the Healthcare Quality Institute of the facility and met the exemption criteria of Institutional ethical review because the work was considered service improvement and not human subject research.
The study population comprised Priority-1 trauma patients, who arrived at the Emergency Radiology department.
The inclusion criteria for Priority-1 Trauma patients were as follows:
- Traumatic Arrest
- Systolic Blood Pressure <90 mmHg. BP < Age-specific normal in children. BP < 110 if age > 65 years
- GCS < 8 related to trauma
- Intubated, compromised airway, need for ventilator support or respiratory rate < 10 or > 29 BPM (< 20 in infant <1 y/o)
- Amputation proximal to wrist or ankle
- Burn with trauma with any of the above (1-4)
- Hanging with any of the above (1-4)
- Major Vascular Injury.
- Neurologic deficit or paralysis.
- Penetrating injury to the head, neck, torso, or extremity proximal to the elbow or knee.
- Crushed, degloved, mangled, or pulseless extremity.
- Inter-hospital transfer of trauma patients receiving blood to maintain vital signs.
- Trauma surgeon or emergency physician discretion.
All the male and female patients of all ages meeting the above criteria were included in the study.
The following patients were excluded from the study:
- Priority-1 trauma patients with no CT examinations e.g., Patient demise before CT scan or patients were taken to the operating theatre before a CT scan.
- Automatically approved cases e.g., requests for CT head alone, requests for CT angiography.
- CT studies of Priority-1 trauma patients done without electronic requests e.g., CT scan done during the RIS downtime using paper requests.
- Priority-1 trauma patients with incomplete data on the Radiology Information system (RIS).
- Priority-1 trauma patients with duplicate values/records.
Vetting time was defined as the time from electronic request placement by the trauma physician in the trauma room to the time of acceptance of the request by the reporting radiologist in the Emergency Radiology Department.
Baseline measurement:
Baseline data for the Pan CT scan vetting time of 155 Priority-1 trauma patients in the preceding six months were retrospectively retrieved from the Trauma Room Registry and the RIS (Radiology Information System). A total of 155 cases met the inclusion criteria. However, 48 cases were excluded from the analysis based on the predefined exclusion criteria.
Design:
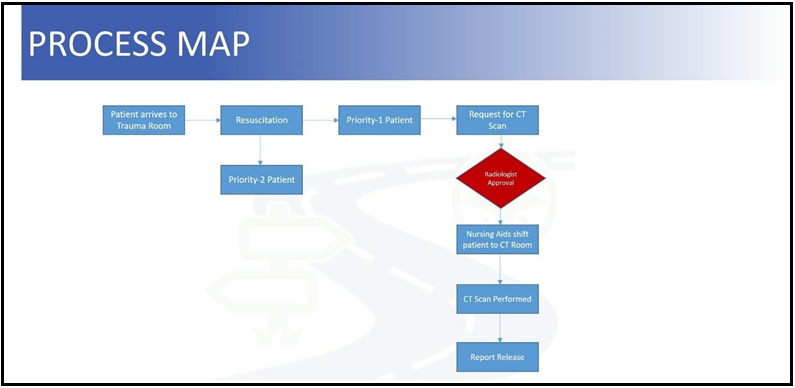
A process map was first formulated to depict the existing pathway from the time a patient arrives at the trauma room, to the time when the report is released (Figure no 1).
Figure 1: Process map of existing pathway from the time a patient arrives at the trauma room, to the time when the report is released.
A cause-effect analysis was undertaken to study the potential causes contributing to the delay in the vetting process. The potential causative factors for the vetting delay were subdivided into four main categories i.e., factors related to Process, People, Policy, and the Environment. The subcategories in each of these factors were enlisted to analyze various elements in play and to arrive at possible solutions to overcome the stumbling blocks (Figure no 2).
Figure 2: Potential causes contributing to the delay in vetting process.
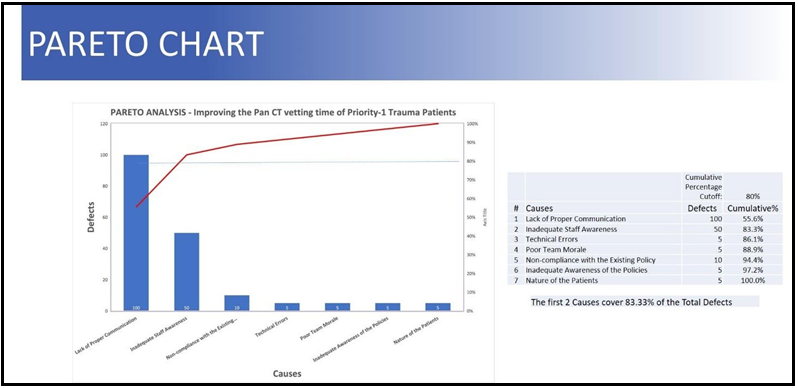
After scrutiny of these factors, a statistical technique of Pareto analysis was used to identify those causes that may contribute most significantly to the delay in the vetting process (Figure no 3). Pareto Analysis is a decision-making technique used to select a limited number of causes that produce a significant overall effect [11]. The Pareto Principle, also known as the 80/20 Rule or the law of the ‘Vital few and the trivial many’, illustrates that 80 % of effects arise from 20 % of the causes i.e. 20 % of actions/activities will account for 80 % of the results/outcomes. It is named after the Italian economist Vilfredo Pareto, who observed that 80 % of income in Italy went to 20 % of the population [12]. The Pareto Principle has many applications in quality control and is the basis for the Pareto diagram, one of the critical tools used in quality improvement analysis.
Figure 3: Pareto Chart.
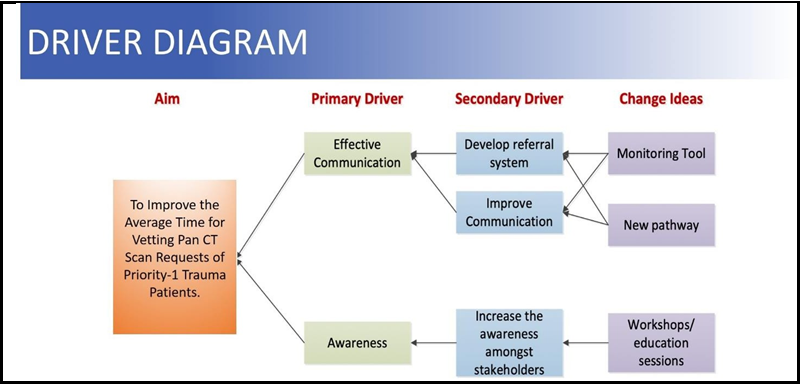
The common factors contributing to the delay in vetting were enlisted after thorough brainstorming sessions with the trauma surgeons, trauma nurses, reporting radiologists, radiology technicians, and radiology clerks. These factors were: Lack of effective and formal communication between the stakeholders, inadequate awareness among the personnel, technical errors and glitches, poor team morale at times due to heavy workload, suboptimal compliance with or inadequate awareness of the policies, and patient factors like unstable patients requiring resuscitation or stabilization, etc. The Pareto analysis revealed that an effective communication pathway between the trauma and radiology teams and staff awareness is imperative and should be the primary areas of focus in an attempt to reduce the vetting time. A driver diagram was devised accordingly (Figure no 4).
Figure 4: Driver diagram.
A reinforced robust communication between the trauma and radiology team was envisaged by employing a new communication pathway (Figure no 5). In this new pathway, to ensure effective real-time cognizance of any expected Priority-1 trauma case, the radiology technician in the CT suite is immediately informed via telephonic communication by the trauma team’s attending physician or nurse. The radiology technician in turn promptly relays this information to the on-call radiologist. This enables the on-call radiologist to be aware of the impending request in advance and comply with it as soon as it arrives on the vetting list in the RIS.
Figure 5: Process map after introduction of the ‘Monitoring tool’.
With the new communication pathway in place, a monitoring tool (Table no 1) was developed to document the patient’s hospital chart number, date of the study, time of arrival of request for CT scan, time at which a call was received from the trauma room, time of call made to the on-call radiologist, time of vetting the request, names of the radiology technician and on-call radiologist. A separate column for any additional notes was also provided to document technical difficulties, patient resuscitation/stabilization, or any other factors contributing to delay. Before adopting the monitoring tool, the CT technicians and the Radiologists were trained to be competent in implementing new proposed changes, through educational sessions and workshops. Printouts of the policy were made available, and the CT technicians/radiologists were instructed to report any technical glitches to the IT department instantly. Periodic feedback was obtained during the implementation of the monitoring tool.
Table 1: Monitoring tool for Radiology Pan CT request Vetting of Priority-1 Trauma Patients.
|
MONITORING TOOL |
|||||||||
|
Sl no |
Patient Hospital Chart number |
Date of study |
Time of Request |
Time of call from Trauma |
Time of call to on call Radiologist |
Tine of request Vetting |
Name of CT Technician |
Name of on call Radiologist |
Notes |
|
1 |
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
5 |
|
|
|
|
|
|
|
|
|
|
6 |
|
|
|
|
|
|
|
|
|
|
7 |
|
|
|
|
|
|
|
|
|
|
8 |
|
|
|
|
|
|
|
|
|
|
9 |
|
|
|
|
|
|
|
|
|
|
10 |
|
|
|
|
|
|
|
|
|
|
11 |
|
|
|
|
|
|
|
|
|
|
12 |
|
|
|
|
|
|
|
|
|
|
13 |
|
|
|
|
|
|
|
|
|
|
14 |
|
|
|
|
|
|
|
|
|
|
15 |
|
|
|
|
|
|
|
|
|
|
16 |
|
|
|
|
|
|
|
|
|
|
17 |
|
|
|
|
|
|
|
|
|
|
18 |
|
|
|
|
|
|
|
|
|
|
19 |
|
|
|
|
|
|
|
|
|
|
20 |
|
|
|
|
|
|
|
|
|
|
21 |
|
|
|
|
|
|
|
|
|
|
22 |
|
|
|
|
|
|
|
|
|
Results
The cumulative baseline pre-intervention pan CT scan vetting time of 107 eligible Priority-1 Trauma patients cases from the retrospective data analysis of 6-month duration was found to be 1598 minutes. The mean vetting time for these patients was 14.93 minutes.
During the 2 months intervention period, 57 Priority-1 trauma cases underwent pan CT scan in the department. Out of these, 30 met the inclusion criteria. The mean vetting time among this group was found to be 10.4 minutes.
The mean vetting time of the entire study population is illustrated in the run chart (Figure no 6), showing the period from baseline to post-implementation of the monitoring tool. With the implementation of the above-mentioned intervention, there was a resultant 30.3 % reduction in the mean vetting time from 14.93 minutes to 10.4 min. Thus, with the application of a simple yet efficient intervention with a monitoring tool emphasizing an effective communication pathway between the Trauma team and the Emergency Radiology team, there was a noticeable reduction in the vetting time of Pan CT requests.
Figure 6: Run chart depicting the mean vetting time of the Pan CT scans spanning the study duration.
Discussion
Diagnostic imaging forms an essential component in reducing the mortality of polytraumatized patients by aiding appropriate diagnosis and guiding emergency and definitive treatment [13]. The role of Clinical Imaging has significantly increased in such patients, especially with the augmentation of radiological equipment and the introduction of Whole-body Computed tomography (WBCT), also referred to as pan CT.
The mortality rate following a polytrauma incident varies between 10 % and 20 % and can be as high as 63 % when associated with brain injuries and up to 35% with pelvic fractures [14]. A positive outcome depends upon recognizing and managing the various injuries, and hence the emphasis on early imaging guided decision making, enabling the clinicians to focus on life-threatening injuries. Hence a delay in imaging could pose a major risk of mortality, especially in Priority-1 Trauma patients.
The on-call Radiologist not only has to report the real-time studies like Plain radiographs, Ultrasound, and CT scans but also bears the responsibility to vet the radiology requests, thereby scrutinizing each one of them for appropriateness and then either accept, reject or place the request for discussion. Vetting radiology requests in a hustling Radiology department is often a cumbersome and time-consuming process. In the event of a Priority-1 Trauma patient arriving at the hospital, the request for a Pan CT scan may linger in the vetting list of the RIS unnoticed especially if the Radiologist is busy reporting other cases, consequently resulting in a delay in its vetting and eventually leading to a delay in imaging and definitive care.
Our study has demonstrated that it is possible to substantially reduce the vetting time of Priority-1 trauma patients in busy radiology set up by the introduction of an effective communication pathway between the Trauma and Emergency radiology teams and a monitoring tool. Improving the vetting time of Priority-1 trauma patients is a multi- factorial issue that requires multidisciplinary collaboration between the Trauma and Emergency Radiology teams. A reduced vetting time implies earlier imaging of the patients, resulting in a faster diagnosis, which in turn aids in prompt treatment of critical injuries, ultimately translating into better patient outcomes.
Conclusion
Our study demonstrates that a simple yet effective monitoring tool with special emphasis on active and prompt communication between the Trauma team and the Emergency radiology team can be a crucial cog in the wheel to substantially reduce the vetting time of Pan CT scans in Priority-1 trauma patients. The model can be easily adopted in any hospital that caters to Trauma patients as a quality improvement endeavour.
Acknowledgment: We would like to acknowledge the Trauma Surgery Team of Hamad General Hospital and the CT Technologists for the unwavering support.
References
- Mackersie RC (2006) History of trauma field triage development and the American College of Surgeons criteria. Prehosp Emerg Care. 10(3): 287–94.
- National Association of EMS Physicians, American College of Surgeons-Committee on Trauma. (2011) Field triage of the injured patient. Prehosp Emerg Care. 15(4): 541.
- The ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, and the International ATLS working group. (2013) Advanced trauma life support (ATLS®): The ninth edition. J Trauma Acute Care Surg. 74(5): 1363–6.
- Harrois A, Hamada S, Laplace C, Duranteau J, Vigué B (2013) The initial management of severe trauma patients at hospital admission. Ann Fr Anesth Reanim. 32(7–8): 483–91.
- Cline MR, Cherry-Bukoweiz J, Machado-Aranda D, Chong ST (2016) Diagnostic limits, blind spots, and pitfalls in CT imaging of blunt abdominal trauma. Contemp Diagn Radiol. 39(22): 1–6.
- The vetting of requests for an imaging examination. Rcr.ac.uk.
- Standards of practice and guidance for trauma radiology in severely injured patients, second edition. Rcr.ac.uk.
- Values. Available from: https://www.hamad.qa/EN/Education- and-research/Academic-Health/About/Pages/Values.aspx
- JCI accreditation standards for hospitals, 7th edition. Joint Commission International.
- Available from: https://www.hamad.qa/EN/About-Us/find-out- more/Documents/HMC-Corporate-Brochure-English.pdf
- Picarillo AP (2018) Introduction to quality improvement tools for the clinician. J Perinatol. 38(7): 929–935.
- Buchanan M (2002) Wealth happens. Harv Bus Rev. 80(4): 49– 54, 124.
- Thippeswamy PB, Rajasekaran RB (2021) Imaging in polytrauma- Principles and current concepts. J Clin Orthop Trauma. 16: 106– 113.
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380(9859): 2095–2128.