Binbin He, Rui Xia*, Bo Li, Shun Guo, Weiwei Liu, Li Tang, Wei Xu
All authors: Department of Anesthesiology, The First Affiliated Hospital of Yangtze University, No. 55 North Jianghan Road, Shashi District, Jingzhou city, 434000, Hubei province, China
*Corresponding Author: Rui Xia, PhD, Chief Doctor, Department of Anesthesiology, The First Affiliated Hospital of Yangtze University, No. 55 North Jianghan Road, Shashi District, Jingzhou city, 434000, Hubei province, China.
Abstract
Objective "Tubeless general anesthesia" is achieved with a humidified rapid insufflation ventilatory exchange (THRIVE) technique in elderly patients undergoing upper esophageal foreign body removal surgery.
Methods Ten patients undergoing upper esophageal foreign body removal surgery received a non-intubated intravenous anesthesia strategy with BIS maintained at 50-60 levels and oxygen supply provided by the THRIVE,100 % oxygen, 40-70 litres.min-1. MAP, HR, SpO2, apnoea oxygenation time, minimum SpO2, and arterial blood gas (PaO2, PaCO2, pH) were monitored and recorded for every subject.
Results Ten patients aged 66(65,70) years, BMI 24.70 (3.11) kg.m-2, ASA(Ⅱ-Ⅲ) were included. The MAP and HR were stable during anesthesia without vasoactive medication intervention, while these data changed within 25 % of baseline. Patients were well oxygenated, SpO2 was never below 90 %, and SpO2 ≥ 98 % for eight patients. SpO2 dropped transiently to 90 % and 93 % in two patients during the anesthesia induction, but SpO2 > 96 % was maintained after jaw-thrust and facemask ventilation. The mean apnoea oxygenation time was 15.64(3.63) min. PaCO2 steadily increased, and pH gradually declined within 15 minutes of asphyxia, but PaO2, PaCO2, and pH after the patient's awakening were notsubstantially different from baseline.
Conclusion The THRIVE technique allows "tubeless anesthesia" for esophageal foreign body removal surgery in elderly patients undergoing general anesthesia. However, monitoring of PaCO2 and pH is necessary.
Keywords: Humidified Rapid-Insufflation Ventilatory Exchange; Esophageal foreign body removal surgery; Intravenous Anesthesia
Introduction
Esophageal foreign body removal surgery is a standard ENT emergency procedure and frequently occurs in elderly patients. The operation is brief and minimally invasive, and the patient recovers rapidly without requiring a deep anesthetic level. As a result of the need for intraoperative mandibular relaxation and a shared upper airway, general anesthesia with endotracheal intubation is typically used.
Tracheal intubation and extubation frequently result in intense stress reactions and circulatory fluctuations [1]. Moreover, the anesthetic level required to control tracheal intubation stress is about three times that needed for surgical skin incision.
The combination of cardiovascular illness and poor circulatory reserve function in geriatric patients renders them highly vulnerable to anesthetic medications. In older individuals, the incidence of hypotension and bradycardia will increase if the level of anesthesia is too deep; if the level of anesthesia is too light, tracheal intubation and extubation will trigger a significant stress response, elevated blood pressure, and accelerated heart rate, which will cause large circulatory fluctuations and cardiovascular accidents.
Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) device delivers continuous, warm, and 100 % humidified O2 at a high flow rate through a nasal cannula to clinically apneic patients to meet the requirements of apnea oxygenation and thus extends the duration of apnea, which can last up to 65 minutes [2,3]. This report describes the use of THRIVE in elderly patients undergoing foreign body removal from the upper esophagus surgery during general anesthesia and serves as a clinical reference.
Materials and Methods
This report was obtained with informed consent from patients and their families and approved by the Ethics Committee at the First People's Hospital in Jingzhou city, Hubei Province, China. Ten patients, 5 males and 5 females, aged 66(65,70) years, with BMI 24.70 (3.11) kg.m-2, ASA(Ⅱ-Ⅲ), presenting for upper esophageal foreign body removal surgery were included in this observation report that is descriptive and prospective. There was no difficulty airway in the preoperative evaluation; the foreign body was in the upper esophagus, and the procedure duration was below 30 minutes. Exclusion criteria: problems such as pneumothorax and cardiac rupture resulting from a foreign body penetrating the esophagus, trachea, heart, lung, and other vital organs; gastrointestinal system illnesses such as full stomach and intestinal obstruction.
The patient was not permitted to drink liquids for four hours or eat food for eight hours before surgery. Intravenous access was established in the operation room for Lactated Ringer's Solution. Noninvasive blood pressure (NBP), SpO2, RR, HR, and ECG were continually monitored, and radial artery cannulation was completed under local anesthesia. After 5 minutes, invasive arterial pressure was continuouslymonitored, and blood samples were obtained for arterial blood gas (ABG). The BIS monitor was employed to evaluate the depth of anesthesia, while the organon muscle relaxation monitor was utilized in TOF.
All patients were pre-oxygenated with an OptiflowTM (Fisher &Paykel Healthcare, New Zealand) at a rate of 10 litres.min-1 for 10 min. Intravenous anesthesia induction then commenced with propofol target-controlled infusion boluses (TCI), and plasma concentration raised gradually from 1.0μg.mL-1 to 2.0~3.0μg.mL-1, sufentanil 0.1~0.2μg.kg-1, suxamethonium chloride injection 1.5~2.0mg.kg-1, followed by a peripheral infusion of propofol at concentration of TCI plasma 2.0~3.0μg.mL-1 and remifentanil at a speed of 5~15 g.(kg.h)-1. The additional intraoperative amount of suxamethonium chloride was 1 mg.kg-1. The dosage and rate of anesthesia drugs were modified according to the patient's circulatory alterations. The concentration of propofol TCI was adjusted to 1.0~1.5μg. mL-1 and remifentanil were discontinued at the end of the operation. After the propofol infusion was terminated, the OptiflowTM was changed to 10~20 litres.min-1 until spontaneous breathing recovery. After fully awakened (the patient could open his eyes, raise his head for more than 5 seconds, and raise upper limbs for more than 10 seconds), he was deoxygenated for 10 minutes before returning to the ward.
The termination criteria: surgery duration>30 minutes, PaCO2 > 82.5 mmHg, pH 7.15, SpO2 < 90 %, or malignant arrhythmia incidence. If these items were met, tracheal intubation and mechanical ventilation were used to end the asphyxiation period. If 90 % ≤ SpO2 < 95 %, provide jaw-thrust and facemask ventilation supports until SpO2 reaches 98 %; otherwise, perform tracheal intubation. Managing all other emergency airway conditions refers to the 2015 DSA guidelines [4]. If MAP varies (< 65 mmHg or > 125 mmHg) and HR is altered (<50 or >100 beats.min-1), appropriate vasoactive drugs are necessary. Each subject was operated on by the same team of otolaryngologists and anesthesiologists using the same equipment.
MAP, HR, and SpO2 are also recorded at the specified times: five minutes after radial artery puncture(T1), one minute before insertion of the esophagoscope into the mouth cavity(T2), after reassembling the esophagoscope(T3), in termination of surgery(T4), two minutes before departure from the operating room(T5). In addition, at the following times: 5 minutes after radial artery cannulation (baseline, BL), total asphyxiation duration (marked in the order of 0min,5 min, 10 min until 30 min), spontaneous breathing recovery (RR), full waking (ED),PaO2, PaCO2, and pH are recorded.
Statistical analysis
Normally distributed data are presented as Mean (SD), and a one-way ANOVA test was utilized for within-group comparisons. Skewed data are presented as M(IQR), and Kruskal Wall's Test was used for within-group comparisons (SPSS25.0 software). GraphPad Prism software was applied to statistical charting.
Results
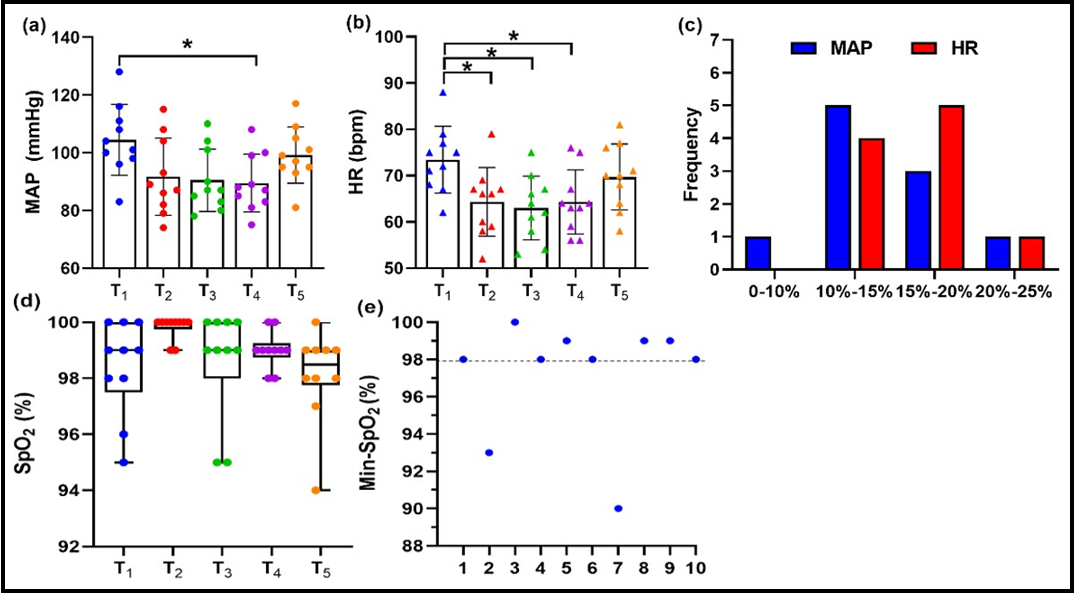
Information about patients' age, sex, BMI, ASA grade, additional medical records, intraoperative adverse events, duration of apnoea, duration of anesthesia, and duration of awakening were presented in (Table 1). The MAP and HR at T1 to T5 for 10 patients are shown (Figure 1a-b). MAP and HR changed within 25 % of the baseline, with 9 cases within 20 % and 1 between 20 % and 25 % (Figure 1c). Ten patients' SpO2 at T1 to T5 was shown (Figure 1d). The difference in SpO2 between baseline and T2 to T5 was not statistically significant. Patients were well oxygenated, SpO2 was never below 98 % for eight patients, and the minimum SpO2 was 90 % and 93 % in two cases in Figure 1(e). One patient with asphyxia oxygenation time beyond 20 mins was excluded. PaO2, PaCO2, and pH of nine patients are presented in Figure 2(a-c). PaO2, PaCO2, and pH between baseline and full waking were not statistically significant. During apnoea 0~5min, 5~10min, and 10~15min, PaO2 increased by 13.58, 11.02, and 4.17mmHg.min-1; PaCO2 increased by 2.08, 2.14, 0.96 mmHg.min-1; pH fell by 0.10,0.008, 0.006 min-1 (Figure 2d-f).
Table 1 Patient characteristics; F=female, M=male; BMI=body mass index; ASA=American Society of Anesthesiologists; Medical records= additional medical records; Intraoperative adverse events including: nose itching or nasal bleeding, SpO2 < 95 %, MAP or HR fluctuation range greater than 25 % of baseline, postoperative nausea and vomiting, choking and coughing; Duration of apnoea=from administration of neuromuscular blockade to commencement of spontaneous breathing; Duration of anesthesia=from anesthesia induction to departure from the operation room; Duration of awakening=from finishing surgery to departure from the operation room; M/M=mean or median, SD=standard deviation, IQR=interquartile range; DM=diabetes mellitus; SLE=systemic lupus erythematosus; HBP=hypertension; Min SpO2=intraoperative minimum peripheral oxygen saturation.

Figure 1 Comparison of MAP and HR at various times (a-b). The intraoperative MAP and HR variations range compared to baseline (T1) (c). Comparison of SpO2 at multiple times (d). Minimal intraoperative SpO2 in 10 subjects (e). Each point represents an individual patient. MAP= mean arterial pressure, HR=heart rate.
Figure 2 Comparison of PaO2, PaCO2, and pH at various times (a-c). The data is excluded because there was just one case at 20 minutes of asphyxiation oxygenation time. Each point represents an individual patient: PaO2, PaCO2, and pH overtime during the anesthesia (d-f). Data are presented as mean (SD), n=10.Baseline=5 minutes after radial artery cannulation, 0-20min=total asphyxiation duration, RR= spontaneous breathing recovery, ED=full waking. PaO2=partial pressure of arterial oxygen, PaCO2=partial pressure of arterial carbon dioxide.
Discussion Retrospective
Chinese aging population has increased the number of elderly surgery patients. Elderly individuals with a high prevalence of esophageal foreign bodies removal surgery have a limited tolerance for tracheal intubation and extubation, which causes intense stress reactions, and increased sensitivity to circulatory depression induced by anesthetic drugs, causing severe circulatory swings. Tracheal intubation may obstruct the operator's view, whereas sore throat, hoarseness, laryngospasm, and lung infection follow tracheal extubation. There are no clinical case reports on the THRIVE in elderly patients performing general anesthesia for upper esophageal foreign body removal surgery. Intraoperative MAP changed within 10 % of the baseline in one patient, 10 %-15 % in five cases, 15 %-20 % in three cases, and 20 %-25 % in one case. HR changed within 15 % of the baseline in four patients, 15 %-20 % in five points, and 20 %-25 % in one case. (Figure 1c). After induction of anesthesia, all patients did not have significant hypotension or bradycardia, nor a sudden increase in blood pressure or heart rate without vasoactive medication intervention. Analysis of possible reasons: (1) small circulatory fluctuations following induction of anesthesia are related to propofol TCI; (2) the fundamental requirement of general anesthesia is the loss of consciousness and the suppression of the reflex to injurious stimuli. Trauma and stress caused by tracheal intubation are far more than those caused by the surgery. The procedure was completed with THRIVE, avoiding the stress response caused by tracheal intubation and the depth of anesthesia required for tracheal intubation, which reduced anesthetic medication dosage and ensured steady circulation. (3) The operation is minimally invasive, and postoperative recovery is painless. Thus, the THRIVE provides a satisfying intraoperative oxygen supply, preventing the stress response from tracheal intubation and circulatory depression from deep anesthesia. Propofol is chosen as a sedative because sufentanil may exacerbate myoclonus-induced etomidate [5]. The impact of circulatory fluctuations on patients may be lessened if intraoperative etomidate TCI is performed, which is one of the limitations of this report.
Apnoea oxygenation time is 15.64(3.63) min, with a maximum of 22 minutes (Table 1). an intraoperative SpO2 of 8 patients is never below 98 %. (Figure 1d). The tendency of PaO2 increases within 15 min of apnea (Figure 2a). These are the physiological mechanisms: (1)THRIVE effectively improves preoxygenation[6]; (2)The exchange of O2 from the alveoli to the blood during hypoxia causes alveolar pressure below atmospheric pressure, generating a negative pressure gradient of up to 20 cmH2O, which drives oxygen into the alveoli from the physiological dead space[7]; (3)Low levels of continuous positive airway pressure and high FiO2 are provided [8,9]. (4) Reduce upper airway resistance and labor of breathing [10]. However, one patient's SpO2 dropped to at least 90 % following induction of anesthesia and was maintain at 96 % - 98 % after jaw-thrust and facemask ventilation; in another patient, SpO2 dropped to 93 % during induction of anesthesia and held at 99 % after jaw-thrust. Oxygen saturation decrease mainly due to upper airway obstruction caused by glossoptosis after anesthesia induction. Adequate intraoperative oxygenation was achieved by mask ventilation and upper airway patency with jaw-thrustand inserting an esophagoscope in the mouth.
Furthermore, C. Lyons et al. [11] concluded that high-flow nasal cannula therapy under apnea conditions can provide a satisfying gas exchange for tubeless anesthetic during laryngeal surgery. Similarly, Kotwinski et al. [12] THRIVE has been utilized safely and successfully during non-intubated laryngoscopy and brief laryngeal surgery under total intravenous anesthesia.
PaCO2 is also found to have a rising trend within 15 min of apnea. The accumulation of CO2, generated by the continuous gas exchange in the alveolar cavity, which cannot be evacuated from the body due to relaxed respiratory muscles, is the primary reason for the increase in PaCO2 and the decline in pH. Similar results were reported in a study by I. M. Gustafsson et al. [13] PaCO2 steadily declines when the patient spontaneous breathing recovered. PaCO2 and pH between baseline and full waking are not statistically significant (Figure 2b-c). This suggests that CO2 accumulation in operation dosen't result in a rise in PaCO2 and a drop in pH after the surgery. Therefore, constant monitoring of PaCO2 and pH is necessary while utilizing THRIVE. Some suggestions are given: (1) adequate preoxygenation is a prerequisite for securing intraoperative oxygen delivery; (2) the nasal catheter must be secured to prevent insufficient oxygen supply caused by nasal catheter dropping out of the nose; (3) When intraoperative SpO2 declines with THRIVE in the procedure, jaw-thrust and facemask ventilation, nasopharyngeal airway combined with THRIVE can restore oxygen saturation. Based on the above observations about PaO2, PaCO2, and pH, facemask ventilation is a practical approach for promoting CO2 expulsion between the end of surgery and spontaneous breathing return.
The strategy of non-intubated intravenous anesthesia with the THRIVE technique in esophageal foreign body removal, surgery avoids deep anesthesia and tracheal intubation and avoids a series of complications related to tracheal intubation, stabilizing the circulation in elderly patients, and facilitating their rapid postoperative recovery. However, the problems of increased PaCO2 and dropped pH require more attention. This case report series is a single-center, tiny sample of clinical observations that have not been compared to general anesthesia tracheal intubation protocols. To verify further the THRIVE technique for upper esophageal foreign body removal surgery under general anesthesia, multicenter and large sample studies are needed.
Authors' Contributions
Study design/planning: Binbin He, Rui Xia, Wei Xu
Study conduct: Binbin He, Weiwei Liu, Li Tang.
Data analysis: Binbin He, Bo Li, Shun Guo.
Writing paper: Binbin He.
Revising paper: All authors
References
- Perkins, ZB, Wittenberg MD, Nevin D, Lockey DJ, Brien OB (2013) The relationship between head injury severity and hemodynamic response to tracheal intubation. J Trauma Acute Care Surg. 74(4): 1074-1080.
- Huang L, Dharmawardana N, Badenoch A, Ooi EH (2020) A review of the use of transnasal humidified rapid insufflation ventilatory exchange for patients undergoing surgery in the sharedairway setting. Journal of Anesthesia. 34(1): 134-143.
- Patel A, Nouraei SA (2015) Transnasal Humidified Rapid- Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways.Anaesthesia. 70(3): 323-329.
- Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, et al. (2015) Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 115(6):827-48.
- Han PK, Arnold R, Bond G, Janson D, Abu-Elmagd K (2002) Myoclonus secondary to withdrawal from transdermal fentanyl: case report and literature review. J Pain Symptom Manage. 23(1): 66-72.
- Mir F, Patel A, Iqbal R, Cecconi M, Nouraei SA (2017) A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre- oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia. 72(4): 439-443.
- BARTLETT RG Jr, BRUBACH HF, SPECHT H (1959) Demonstration of aventilatory mass flow during ventilation and apnea in man. J Appl Physiol. 14(1): 97-101.
- Ritchie JE, Williams AB, Gerard C, Hockey H (2011)Evaluation ofa humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. AnaesthIntensive Care. 39(6): 1103-10.
- Sim MA, Dean P, Kinsella J, Black R, Carter R, et al. ( 2008) Performance of oxygen delivery devices when the breathing pattern of respiratory failure is simulated. Anaesthesia. 63(9): 938-40.
- Wang J, Lee KP, Chong SL, Loi M, Lee JH (2018) High flow nasal cannula in the emergency department: indications, safety and effectiveness. Expert Rev Med Devices. 15(12): 929-935.
- Lyons C, Callaghan M (2017) Apnoeic oxygenation with high- flow nasal oxygen for laryngeal surgery: a case series. Anaesthesia. 72(11): 1379-1387.
- Kotwinski D, Paton L, Langford R (2018) The role of high flow nasal oxygen therapy in anaesthesia. Br J Hosp Med (Lond). 79(11):620-627.
- Gustafsson IM, Lodenius Å, Tunelli J, Ullman J, Jonsson FagerlundM (2017) Apnoeic oxygenation in adults under general anaesthesia using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) - a physiological study. Br J Anaesth. 118(4):610-617.