Sherehan Zada MD*, Elise Nguyen MD, Di Lu MD, Min Han MD. PhD, Beverly Wang MD, Behdokht Nowroozizadeh MD
Department of Pathology and Laboratory, University of California, Irvine, USA.
*Corresponding Author: Sherehan Zada MD, Department of Pathology and Laboratory, University of California, Irvine, USA.
Abstract
Pancreas cysts are common lesions in the general population. The identification and accurate classification of pancreatic lesions are essential in order to offer the best treatment plan and avoid any unnecessary interventions. Herein, we analyzed fourteen patients with pancreatic cytology specimens, followed those patients further after their surgical intervention, and subsequently compared their initial cytologic diagnosis with their final diagnosis.
Introduction
The diagnosis of mucinous cysts including intraductal papillary mucinous neoplasm (IPMN) and mucinous cystic neoplasm (MCN) by cytology can significantly impact patient management; however, the diagnosis can be challenging, especially when there is scant material. We aim to describe the cytomorphologic characteristics and the influence of the cytologic findings on clinical management.
Materials and Methods
We identified patients who underwent endoscopic ultrasound and were found to have cysts containing mucin based on cytology. The EUS features, gross aspirate characteristics, ancillary chemistry tests, and cytomorphology were described.
Results
Fourteen patients, who underwent endoscopic ultrasound-guided fine-needle aspiration of pancreatic cysts, had mucin identified by cytology. Four cysts had scant mucin; five were moderate, and five were abundant (Table 1). The texture of the mucin varied from granular to colloid-like with features including cracking, ferning, and folding. Seven aspirates contained glandular cells that ranged from mildly to moderately atypical. Seven aspirates had concurrent CEA, amylase, and lipase samples. Three cases had CEA less than 192ng/ml, and four cases had CEA greater than 192ng/ml. Most cases had significantly elevated amylase and lipase. In thirteen cases out of fourteen, the clinical assessment following cytologic diagnosis was either IPMN or MCN. In five cases, cytologic findings changed the clinical impression from pancreatic cyst not otherwise specified to IPMN or MCN. In six cases, the clinical impression of IPMN was supported. In one case, the clinical impression of pseudocyst was changed to IPMN. In one case, the clinical impression of pancreatic cyst NOS was assessed as pseudocyst after fine-needle aspiration.
|
Case |
Location |
Amount of mucin |
String sign |
Gross description |
CEA ng/ml |
Amylase/Lipase U/L |
|
1 |
Pancreatic tail |
Scant |
|
Thin yellow cloudy |
0.9 |
152 / 212 |
|
2 |
Pancreatic uncinate process |
Scant |
|
Viscous |
|
|
|
3 |
Pancreatic head |
Scant |
|
Viscous brown |
285.3 |
>20000 / 35148 |
|
4 |
Pancreatic neck |
Scant |
|
Reddish cloudy |
7.6 |
- / >60000 |
|
5 |
Pancreatic neck |
Moderate |
12mm |
Very viscous, clear |
|
|
|
6 |
Pancreatic body |
Abundant |
|
|
|
|
|
7 |
Pancreatic head |
Abundant |
|
Viscous clear |
465.3 |
>20000 / 49288 |
|
8 |
Pancreatic head |
Moderate |
|
Viscous yellow semi-cloudy |
101.9 |
>20000 / >60000 |
|
9 |
Pancreatic tail |
Abundant |
|
Very viscous yellow Semi-cloudy |
|
|
|
10 |
Pancreatic uncinate process |
Moderate |
>20mm |
Thick mucinous clear |
|
|
|
11 |
Pancreatic neck |
Moderate |
8mm |
Viscous reddish semi-cloudy |
|
|
|
12 |
Pancreatic head |
Abundant |
10mm |
Viscous |
|
|
|
13 |
Pancreatic body |
Moderate |
0mm |
Pinkish cloudy |
11 |
|
|
14 |
Pancreatic tail |
Abundant |
10mm |
viscous |
65.6 |
|
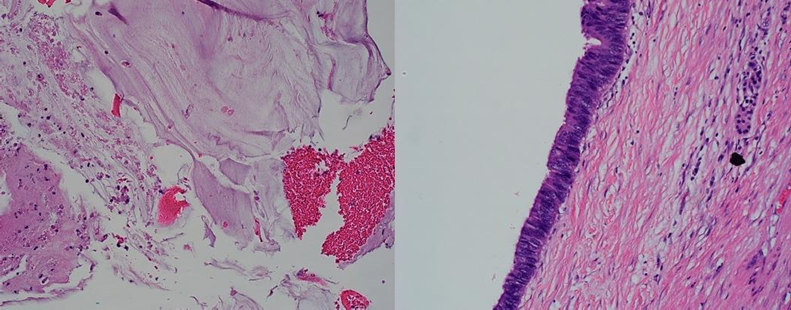
Figure 1- A: Cell block (20X) of pancreas cyst showing abundant acellular mucinous material with mild inflammation and focal hemorrhage, no epithelial components has been detected in the cytology specimen
B: H&E staining (20X) section from the surgical resection specimen revealed intraductal proliferation of intestinal type epithelial with focal low-grade dysplasia consistent with IPMN with focal low-grade dysplasia
Discussion
Pancreas cysts are common lesions in the general population. They have been further classified into inflammatory cysts, true cysts, and cystic tumors [1,2]. The recognition and classification of these lesions are very important as the management plan and the prognosis may differ accordingly. The diagnosis of pancreatic lesions can be a challenge in diagnostic radiology. The most common method for diagnosing these lesions is to use imaging studies [Endoscopic Ultrasonography (EUS), Computerized Tomography (CT) Scan, Magnetic Resonance Imaging (MRI), Cholangiography, and Endoscopic Retrograde Cholangiography (ERCP)] in conjunction with biopsy [3,4,5,6]. Endoscopic guided fine needle aspiration (EUS/FNA) is an efficient method of diagnosing pancreatic cystic lesions and may be able to distinguish mucinous from non-mucinous tumors. Unfortunately, the material obtained from FNA may occasionally be scant and limited. However, the chemical analysis of pancreatic cyst fluid along with the mucin content may still aid in the diagnosis.
The chemical analysis of cyst fluid has been investigated in several studies. The chemical analysis included amylase levels, lipase levels, carcinoembryonic antigen (CEA) levels, and others [3,7,8,9]. High levels of some markers like CEA (cut off of 192 ng/ml) suggested more of a mucinous producing tumor whereas elevated enzymes such as amylase, and lipase favored more of an inflammatory process. Mucin has been found in a variety of pancreatic cysts, although it is most commonly found in mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous neoplasms (IPMNs) [10,11,12,13].
Cyst's mucin content has also been studied in several studies. The features of mucin, including the amount of mucin, the texture of the mucin, the color of the mucin, and the presence of benign or atypical glandular components, can aid in the diagnosis. Where high levels of viscous and cellular material suggested more of a mucinous producing neoplasm[13,14,15,16,17].
In all of our fourteen cases, the morphology of the mucin helped us further exclude inflammatory cysts, suggested true cystic lesions in some cases, and raised the suspicion of possible dysplastic processes in rare cases.
Conclusion
Fine needle aspirate can be useful in determining the nature of a pancreatic cyst. Although the aspirate may yield scant material and cellularity, the cytomorphologic features, when considered with radiographic, and chemical findings, can help determine if the cysts are neoplastic. Although some aspirates in the case series were acellular and CEA levels less than 192ng/ml, the presence of mucin raises the concern for mucinous neoplasm, warranting surveillance by endoscopic ultrasound. This case series highlights the importance of detecting and reporting the presence of mucin by cytology.
References
- Garcea G, Ong SL, Rajesh A, Neal CP, Pollard CA, et al. (2008) Cystic lesions of the pancreas. A diagnostic and management dilemma. Pancreatology. 8(3): 236–251.
- Siriwardena AK (2005) Contemporary management of pancreatic pseudocysts. Pancreatology. 5(6): 507–509.
- Acar M, Tatli S (2011) Cystic tumour of the pancreas: a radiological perspective. Diagn Interv Radiol. 17(2): 143–149.
- Al-Haddad M, El Hajj II, Eloubeidi MA (2010) Endoscopic ultrasound for the evaluation of cystic lesions of the pancreas. J Pancreas. 11(4): 299–309.
- Baron TH, Morgan DE (1997) The diagnosis and management of fluid collections associated with pancreatitis. Am J Med. 102(6): 555–563.
- Parra-Herran CE, Garcia MT, Herrera L, Bejarano PA (2010) Cystic lesions of the pancreas: clinical and pathologic review of cases in a five-year period. J Pancreas. 11(4): 358–364.
- Sugiayam M, Aomi Y (1998) Intraductal papillary mucinous tumours of the pancreas: imaging studies and treatment strategies. Ann Surg. 228(5): 685–691.
- Koito K, Namieno T, Nagakawa T, Shyonai T, Hirokawa N, et al. (1997) Solitary cystic tumour of the pancreas: EUS-pathologic correlation. Gastrointest Endosc. 45(3): 268–276.
- Sedlack R, Affi A, Vazquez-Sequeiros E, Norton ID, Clain JE, et al. (202) Utility of EUS in the evaluation of cystic pancreatic lesions. Gastrointest Endosc. 56(4): 543–547.
- Recine M, Kaw M, Evans DB, Krishnamurthy S (2004) Fine needle aspiration cytology of mucinous tumours of the pancreas. Cancer. 102(2): 92–99.
- Pitman MB, Deshpande V (2007) Endoscopic ultrasound guided fine needle aspiration cytology of the pancreas: a morphological and multimodal approach to the diagnosis of solid and cystic mass lesions. Cytopathology. 18(6): 331–347.
- Ryu JK, Woo SM, Hwang JH, Jeong JB, Yoon YB, et al. (2004) Cyst fluid analysis for the differential diagnosis of pancreatic cyst. Diag Cytopathol. 31(2): 100–105.
- Petrone MC, Arcidiacono PG (2001) Role of endoscopic ultrasound in the diagnosis of cystic tumours of the pancreas. Dig Liver Dis. 40(11): 847–853.
- Rafique A, Freeman S, Carroll N (2007) A clinical algorithm for the assessment of pancreatic lesions: utilization of 16- and 64-section multidetector CT and endoscopic ultrasound. Clin Radiol. 62(12): 1142– 1153.
- Stelow EB, Shami VM, Abbott TE, Kahaleh M, Adams RB, et al. (2008) The Use of Fine Needle Aspiration Cytology for the Distinction of Pancreatic Mucinous Neoplasia. American Journal of Clinical Pathology. 129(1): 67–74.
- Boot C (2014) A review of pancreatic cyst fluid analysis in the differential diagnosis of pancreatic cyst lesions. Annals of Clinical Biochemistry. 51(2): 151-166.
- Brugge BR (2015) Diagnosis and management of cystic lesions of the pancreas. J Gastrointest Oncol. 6(4): 375–388.



