Anamika Saha1*, Erin Demoulin2, James Newman3
1MBBS, Clinical Development Fellow, Glasgow Royal Infirmary, Glasgow, G4 0SF, Scotland.
2MBChB MRCS, ST5 Trauma and Orthopedic Registrar, York District Hospital, England.
3MB ChB, MRCS, FRCS (Tr & Ortho) Consultant, Trauma and Orthopedics, The Mid Yorkshire Hospitals NHS Trust, UK.
*Corresponding Author: Anamika Saha MBBS, Clinical Development Fellow, Glasgow Royal Infirmary, Glasgow, G4 0SF, Scotland.
Abstract
Aims: In the UK, around 70,000 people require hip surgery annually. Often patients are elderly and frail with multiple co-morbidities making them more vulnerable to higher risk of respiratory compromise and mortality associated with COVID-19. The aim of this study is to determine the increased morbidity and mortality associated with peri-operative COVID-19 infection in neck of femur (NOF) fracture patients.
Methods: We conducted a retrospective, descriptive study involving 188 NOF fracture patients who underwent surgery from 21/03/2020 to 21/07/2020 in The Mid Yorkshire Hospitals Trust. Only people who tested positive for COVID-19 within 30 days of operation were included in the positive cohort. The primary outcome was the 7- and 30-day mortality rate. The secondary outcomes were total hospital stay and pre- and post-operative symptoms in NOF fracture patients undergoing surgery.
Results: In total, 188 patients were included. 21 patients tested positive for COVID-19, 16 within 30 days of operation and the remaining 5 tested positive beyond 30-day from operation. 24 were not tested. 143 tested negatives. The average age of patients was 79.02±11.163 years. Average hospital stay was 14.69±10.66 days (average stay for positive patients 22±13.79 days). 12 patients had pre-operative symptoms (respiratory symptoms and fever) out of which 2(16.67 %) tested positive. 7-day post-op mortality was 2.128 % (6.25 % for COVID-19 positive patients). 30-day mortality was 6.383 % (5.814 % for untested/negative patients and 12.5 % for positive patients). 41 patients (21 .81 %) developed post-operative respiratory symptoms (56.25 % for positive patients). 8.51 % developed post-operative sepsis (25 % of positive patients).
Conclusion: This study has shown that patients with a neck of femur fracture have a high rate of mortality and post-operative co-morbidities when diagnosed with COVID-19 within the perioperative period resulting in an increased length of stay for the patients affected.
Introduction
A SARS-CoV-2 (COVID-19) pandemic was declared by the World Health Organization on 11 March 2020 [1]. The pandemic has caused a large global health crisis, severely impacting the safe and sustainable provision of healthcare worldwide. At the time of writing the report, 220,563,227 cases have been reported worldwide [2]. The infection may result in a spectrum of symptoms varying from asymptomatic infection to dyspnea, refractory hypoxemia, and acute respiratory distress syndrome [3].
Health system resources around the world have been redeployed to manage the crisis, with human and physical resources diverted to meet the rising critical care demands. Many of the resources usually used to provide orthopedic care were repurposed, thus limiting the capacity to continue providing urgent orthopedic care. Our hospital had to restructure its medical operation resulting in loss of dedicated NOF ward. Despite this, the orthopedic team has continued to provide care to patients presenting with neck of femur fracture.
The purpose of this report is to analyses the perioperative mortality rate as well as in patient hospitalization issues associated with neck of femur fracture patients who presented during the global COVID- 19 pandemic.
Materials and methods
A single-center cross-sectional study was performed with analysis of a consecutive series of neck of femur fracture patients who presented to our hospital’s ED between 21/03/2020 to 21/07/2020.
21st March was chosen to be as the first day as this was the start of first peak of COVID-19 activity in our hospital.
Patients who presented with either an OTA/AO 31A or OTA/AO 31B fracture, and patients who had peri-prosthetic fractures of the femur were excluded. Only patients who tested positive for COVID-19 within 30 days of operation were included in the positive cohort.
We analyzed patient demographics, pre-operative symptoms, operative procedure performed, inpatient stay and any inpatient complications. Complications included respiratory symptoms and sepsis.
All analysis was completed with Microsoft Excel.
Early findings were presented in the Trust Clinical Governance Meeting.
Results
Between 21st March 2020 to 21st July 2020, 188 patients were treated surgically for NOF in the Mid Yorkshire Hospitals NHS Trust. Mean age was 79 years ranging from 37 to 98.
Table 1:
|
Operation type |
Number |
Percentage |
|
Hip hemiarthroplasty |
98 |
52 % |
|
DHS/CHS |
33 |
17.5 % |
|
THR |
14 |
7.5 % |
|
Gamma nail |
43 |
23 % |
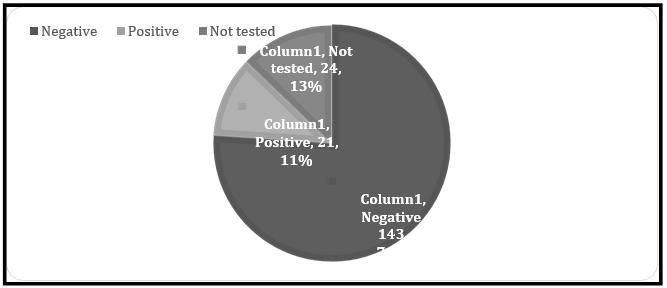
12 patients had pre-operative symptoms (respiratory symptoms, fever) out of which 2 (16.67 %) tested positive in PCR testing. Total 21 patients tested positive for COVID-19, 16 within 30 days of operation and remaining 5 tested positive beyond 30-day period. 24 were not tested. 143 tested negatives.
Chart 1: COVID testing
Only the 16 patients who tested positive during 30 days of their hospital stay were counted in the COVID-19 positive cohort.
Post-operative mortality as well as post-operative respiratory complications were much higher in COVID-19 positive patients compared to COVID-19 negative patients and patients from 2019. They also had a relatively longer hospital stay.
Table 2: COVID-19 positive cohort vs COVID-19 negative cohort
|
|
|
COVID-19 positive |
COVID-19 negative/untested |
Total |
|
ASA, n (%) |
1 |
0 (0 %) |
0 (0 %) |
0 (0 %) |
|
2 |
0 (0 %) |
1 (10 %) |
1 (8.3 %) |
|
|
3 |
1 (50 %) |
6 (60 %) |
7 (58.3 %) |
|
|
4 |
1 (50 %) |
3 (30 %) |
4 (33.33 %) |
|
|
Delay to theatre in days (mean ± SD), median |
|
1, 1 |
1.9 ± 1.375, 1 |
1.75 ± 1.299, 1 |
5 patients passed away after 30 days following their operation. 4 of them were negative and 1 patient was not tested.
Most patients who passed away had ASA grade of 3. Maximum patients (8, 66.67 %) had surgery the day after their admission and 2 patients had surgery within 2 days of their admission. One patient waited 4 days, and another waited 5 days for surgery to optimize them pre-operatively. Both were COVID-19 negative.
Table 3: Demographic of post-op mortality
|
|
|
COVID-19 positive |
COVID-19 negative/untested |
Total |
|
ASA, n (%) |
1 |
0 (0 %) |
0 (0 %) |
0 (0 %) |
|
2 |
0 (0 %) |
1 (10 %) |
1 (8.3 %) |
|
|
3 |
1 (50 %) |
6 (60 %) |
7 (58.3 %) |
|
|
4 |
1 (50 %) |
3 (30 %) |
4 (33.33 %) |
|
|
Delay to theatre in days (mean ± SD), median |
|
1, 1 |
1.9 ± 1.375, 1 |
1.75 ± 1.299, 1 |
Discussion
Elderly patients with COVID-19 have higher morbidity and mortality compared to younger patients and are more at risk of developing severe disease [5]. Our study shows that patients with COVID-19 have higher peri-operative morbidity and mortality, mirroring findings from other specialties [6]. Compared to 2019 and the COVID-19 negative cohort, the COVID-19 positive cohort has increased length of stay as well as increased post-operative mortality. We tried to reduce delay to theatre with the aim of prompt surgical and anesthetic care as per guidelines [7]. However, in certain cases medical optimization prior to surgery was required resulting in delay. Apart from the direct impact of COVID-19 on patients’ health, we were also affected by lack of adequate manpower and resources. Our dedicated combined orthogeriatric ward was redeployed as a COVID ward resulting in patients being admitted to our regular orthopedic ward. Redeployment and staff sickness also affected physiotherapy cover and continuity of care was greatly impacted.
We were limited in our study due to its small sample size and retrospective nature. 13 % of patients did not have a COVID swab after admission even though some were symptomatic. Also, it is possible that some of the patients may have had false negative results. We were unable to follow our patients up for longer period of time to assess long term outcome.
Conclusion
COVID-19 has impacted care of our elderly and vulnerable patients world-wide. Our study shows patients with COVID-19 have significantly higher 30-days mortality despite not having any significant delay to theatre likely due to the impact of COVID-19 on already susceptible and weak patients. They also took longer to be deemed fit enough to leave hospital and had more respiratory complications.
Conflicts of Interest: The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- Royal College of Physicians. Caring for hospital patients with COVID-19: Quality of care in England examined by case record review. London: RCP, 2021.
- WHO Weekly operational update on COVID-19 - 6 September 2021.
- Ramanathan K, Antognini D, Combes A, Paden M, Zakhary B, et al. (2020) Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 8(5): 518-526.
- National Hip Fracture Database Dashboard report for Pinderfields General Hospital (PIN) 2019.
- Liu K, Chen Y, Lin R, Han K (2020) Clinical features of COVID- 19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 80(6): e14-e18.
- Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP (2020) COVID-19 Outbreak and Surgical Practice: Unexpected Fatality in Perioperative Period. Ann Surg. 272(1): e27-e29.
- BGS. Managing Hip Fractures during COVID-19 2020.