Matthew Igwe Nwali1*, Nneka Immaculata Nwali2, Joseph Agboeze1, Charles Nwambeke Edene
1Department of Obstetrics and Gynaecology, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria.
2Department of Public Health, Ebonyi State Ministry of Health, Abakaliki, Ebonyi State, Nigeria
*Corresponding Author: Matthew Igwe Nwali, Department of Obstetrics and Gynaecology, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria.
Abstract
Background: This study was done in Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Southeast Nigeria. It is a tertiary referral hospital in the state serving both the state and some parts of the surrounding states.
Aim: To determine the level of acceptance and the reason behind the disappearing practice of permanent contraception in our gynecological practice.
Methods: A yearly review of sterilization in the family planning unit and a questionnaire-based prospective data collection on the reason behind the low sterilization acceptance rate.
Results: Six thousand three hundred and fifty-three clients used one family planning method or the other during the period under review. Out of this number, only 43 used the sterilization method [Bilateral Tubal Ligation only (BTL)], and there was no vasectomy done. This represents sterilization uptake of less than 1% (0.68%) for female and zero percent for male sterilization (vasectomy). Although the acceptance of female sterilization by BTL has been poor over the years, it decreased to almost zero, like vasectomy during the last three years under review when only 6 BTLs were done.
Conclusion: Sterilization as a contraceptive or family planning method is disappearing in our gynecological practice. Adequate counseling, health education, and re-orientation of our people are required for its acceptance and exercise.
Keywords: Permanent contraception, Southeast, Nigeria
Introduction
Contraception is a method that people can use to prevent or reduce the chance of impregnating their sexual partner during sex to limit or space the number of children they want.[1] Some contraceptive options, such as using condoms, hormonal pills, implants, intrauterine contraceptive devices, injectables, etcetera, are temporary and reversible, some long-acting while others are short-acting, some invasive, and some noninvasive.[2,3] There is a perfect and typical use of birth control. Excellent service describes how effective a form of birth control is if everyone uses it exactly as instructed every time, they have sex. Typical use explains how effective a form of birth control is if a person sometimes uses it as required but may also use it irregularly or imperfectly. Even with perfect use, contraception is not 100% effective.
Vasectomy and bilateral tubal ligation (BTL), on the other hand, are the forms of contraception trusted for permanent birth control for men and women, respectively. There are several different vasectomy techniques, but each works by preventing sperm from entering the vas deferens, the tube it normally flows through to exit the penis. BTL, on the other hand, each line can be closed off with a clip, band, or ring; it can be cauterized or cut. The goal is to prevent the ovum and the sperm cells from meeting in the fallopian tube, where fertilization leading to conception takes place. To cut or tie the lines, a minimally invasive outpatient procedure (mini-laparotomy or laparoscopy) or a more complex surgical method can also be done. The appropriate option depends on a person’s needs and overall health. [4] While some vasectomies and BTL are reversible, the effectiveness of these procedures depends on the method and skill of the healthcare professional who performed the procedure. Vasectomy usually takes about 3 months to become fully effective, so the couple must use alternative methods of contraception during this time. The success rate of vasectomies is higher than 99%, although about 1–2% of people who undergo the procedure experience complications such as pain or excessive bleeding. [5,6]
Sterilization is a permanent method of contraception and is the most commonly used form of family planning among couples in the United States. For men and women who no longer want to have children, it offers a permanent, safe, cost-effective, and efficacious way to prevent unwanted pregnancy. Vasectomy is less standard than Bilateral Tubal Ligation, but both are nearly 100% effective at preventing pregnancy. Data from the Centers for Disease Control and Prevention (CDC) show that among women ages 15 to 44 who use a contraceptive method, one in five used tubal ligations as their method of contraception.[7] The reverse is the case in Sub-Saharan Africa, where there is a low prevalence of acceptance of contraception and a high unmet need for family planning 24%. [8,9,10] Worldwide, about 13% of married women use long-acting contraceptives, but an estimated 80 million unwanted pregnancies still occur per year, which are both mistimed and unwanted. Approximately 280,000 of these women end up in maternal mortality every year, and about 99% of these deaths occur in Sub-Saharan Africa (SSA), including Nigeria. [8,11] Although there is some improvement or increase in the acceptance of long-acting and other family planning or contraceptive methods in our setting, permanent methods or sterilization for both men and women are almost disappearing completely. [12,13] The use of permanent contraception is low. While previous reports have shown acceptance rates for Bilateral Tubal Ligation (BTL) as 8% among women aged 35–44 years and 1.25% of all deliveries, [14,15] Vasectomy is still not widely accepted in many African countries, including Nigeria. [16,17] Previous studies in Nigeria identified Ignorance among males as the significant reason for the low acceptance of vasectomy. [18,19] Ignorance is reflected in widespread misconceptions about vasectomy. These include the belief that it causes impotence, ejaculatory failure, weight gain, and its equation with castration. The spread of accurate information in a population has been shown to improve the perception and acceptability of vasectomy. [20] Several factors were also implicated in the acceptance of female sterilization. These include Ignorance, superstition, religion, and polygamy. [21] Other studies showed spousal support and accessibility to contraception as key to contraceptive use by women. [22,23]
This study is therefore undertaken to evaluate the disappearing practice of permanent contraceptive methods or sterilization for couples that have completed their family size, hence not desirous of pregnancies anymore, and the reasons behind it.
Materials and Methods
This study is carried out in the tertiary hospital in Abakaliki, the capital city of Ebonyi state. They obtain their clients from the postnatal clinics, the general outpatient department, specialist clinics, and referrals from the primary, secondary, and private health centers within the state and the surrounding states.
This is both a retrospective and prospective study that was carried out thus. Data were collected from the family planning records, patients’ folders, and obstetrics and gynecological surgery records.
Information extracted includes sociodemographic characteristics like age, parity, religion, educational status, marital status, occupation, and type of contraception used, if any, from January 1, 2009, to December 31, 2018 (10 years). The prospective aspect of the study involved the use of a questionnaire, which was consecutively administered to the clients in the antenatal clinic, postnatal clinic, and gynecological clinic, respectively, to ascertain the reason for non-acceptance of permanent contraceptives despite not wanting further pregnancy. The information was recorded in the datasheet, and the coded data were fed into the computer using the epi info program 2008, version 3.5.1 (CDC Atlanta GA), and analysis was done. The results are presented in simple percentages, figures, and tables. The required sample size was calculated using the formula:
n = Z2 P(1-P)/d2
n = minimum sample size
Z = degree of confidence at 95% - 1.96
P = 20% from a similar study in Nigeria
d = tolerable error 5%
estimated minimum sample size = 246
considering non-response rate of 10% sample size increased to 273 respondents. Results were presented in simple percentages, tables and figures.
Ethical Issue
Ethical approval was obtained from the research and ethics committee of the hospital. Informed consent was obtained from the clients before recruiting them into the study, and they were given the option to opt out at any time if they did not want to continue. Confidentiality was also ensured as the data collected was used only for the study.
Results
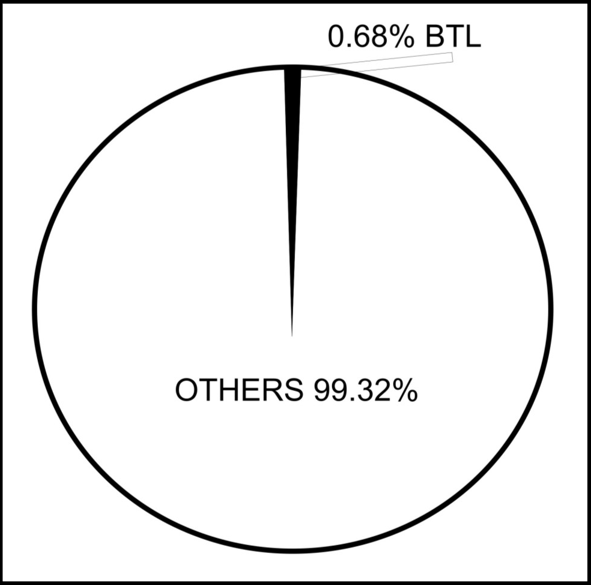
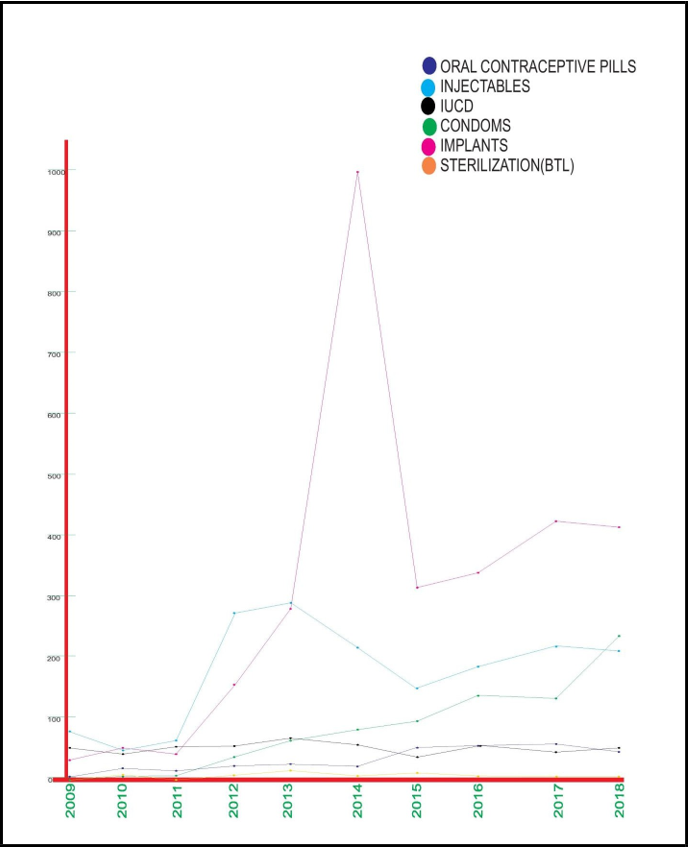
During the ten years (Jan. 2009 – Dec. 2018) in review, 6,353 clients used one family planning method or the other. Out of this number, only 43 used the sterilization method [Bilateral Tubal Ligation only (BTL)]; there was no vasectomy done. This represents sterilization uptake of less than 1% (0.68%) for female and zero percent for male sterilization (vasectomy). Figure 1. The yearly distribution of acceptance of different family planning methods in the hospital over the period in review is shown in figure 2. Although the approval of female sterilization by BTL has been poor over the years, it decreased to almost zero, like vasectomy, during the last three years under review.
Figure 1: Percentage of sterilization compared to other family planning methods.
Figure 2: Yearly distribution of acceptance of different family planning methods over the period in review
Two hundred and seventy respondents (250 females and 20 males) who gave informed consent were recruited into the prospective arm of the study to find out the reasons for non-acceptance of permanent contraception (male/female sterilization). The mean age of the group was 34 ± 8.3 years and ranged between 16 – 55 years. The mean parity for the women participants was 4.8 ± 1.5 and ranged between 1 – 7. Fifty percent of the respondents were aged 30 – 39 years. This was followed by those aged between 20 – 29 years. About 58.4% were grand multiparous, while 40% were between para 1 – 4. About 74.1% were civil servants, while 18.5% were students. About 96.3% were Christians (Table 1).
Table 1: Sociodemographic characteristics of family planning respondents
|
Variables Number (270) % |
|
Age ≤19 3 1 20-29 70 26 30-39 135 50 40-49 42 15.6 ≥50 20 7.4 Sex Male 20 7.4 Female 250 94.6 Parity Number (250) 1 4 1.6 2-4 100 40 ≥5 158 58.4 Education Number (270) None/primary 8 3 Secondary 19 7 Tertiary 243 90 Marital status Unmarried 4 1.4 Married 259 96 Widowed 7 2.6 Occupation Civil servants 200 74.1 Students 50 18.5 Traders 10 3.7 Farmers 6 2.2 House wives 4 1.5 Religion Christianity 260 96.3 Muslim 4 1.5 Others 6 2.2 |
All the men among the respondents would not accept vasectomy, and only 4 would allow BTL to be done on their wives. Among the female respondents, only 10 (4%) would let a vasectomy be done on their husbands if their husbands accepted, and only 30 (12%) would take BTL if their husbands supported them. The primary reason for non-acceptance of sterilization is fear that it can lead to impotence (78%), followed by fear of ejaculatory failure (74.4%) and polygamy (74%) as a result of competition in childbearing among the co-wives. Religion also plays a role in non-acceptance (56%). The health workers also downplay counseling on sterilization. Among the respondents, only 48% heard their health worker mention sterilization during family planning counseling (Table 2).
Table 2. Reasons for non-acceptance of sterilization
|
Variable Number % |
|
Would you accept vasectomy male (20) Yes 0 0 No 0 100 Would you like BTL for your wife Yes 4 20 No 16 80 Would you like vasectomy for your spouse female (250) Yes 10 4 No 240 96 Would you accept BTL Yes 30 12 No 220 88 Give reason** All 270 Spousal support 14 5.2 Ignorance 70 26 Can cause impotence 210 78 Can cause ejaculation failure 201 74.4 It is same as castration 125 46 Superstition a. Impotence/infertility next world 56 21 b. Encore wroth of the gods (culture) 40 15 Polygamy (competition among them) 200 74 Religion (especially Catholics) 150 56 Availability/Accessibility 50 19 Was sterilization discussed by the HW* Yes 130 48 No 140 52 |
**Multiple responses allowed, *Health Worker
Discussion
The use or acceptance of sterilization as a family planning or contraceptive method is disappearing in our gynecological practice. During the years under review, only 0.68% of family planning users accepted BTL. This is far less than the 8% acceptance rate reported by previous studies. [14,15] The two cases done in 2016 were case 1. A grand multiparous woman had a missing IUCD, which an ultrasound scan showed in the peritoneal cavity. She opted for laparotomy to remove the IUCD and signed consent for BTL, which was done case 2. A para 4+0 lady with three previous cesarean sections had uterine rupture elsewhere and was rushed to the hospital but refused a hysterectomy and instead opted for repair and BTL. The 4 cases for 2017 and 2018 were, however, done by mini laparotomy after obtaining informed consent from the clients after counseling. During the period under review, there was no vasectomy done.
The reasons for the non-acceptance of sterilization were fear of impotence, ejaculatory failure, polygamy, religion, castration, superstition, and ignorance. These had been reported in previous studies. [18,19,21] This study has also revealed that education has not been able to erase these beliefs from our setting. This is shown as the majority of the respondents are educated civil servants. The health workers are not giving adequate counseling to the clients about sterilization. This may be a result of discouragement as a result of refusal to accept sterilization after counseling by the clients. Hence, the health workers consider it a waste of time and energy to tell the clients about sterilization. It is also possible that most of the health workers do not want sterilization themselves.
Conclusion
Sterilization as a contraceptive or family planning method is disappearing in our gynecological practice. Adequate counseling, health education, and re-orientation of our people are required for its acceptance and course.
Acknowledgement
We are very grateful to the research and ethics committee of the Alex Ekwueme Federal University Teaching Hospital, Abakaliki, for approving this study protocol. We also express our profound gratitude to the staff of the family planning and medical records units for their assistance in providing the materials for this study, as well as our research assistants who helped us with data collection.
Funding: Still waiting.
Conflict of Interest: None declared.
References
- Central Statistical Agency, ICF, Ethiopia (2016) Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA.
- Charity FPA (2017) Your guide to the contraceptive implant. In. England, FPA.
- USAID (2015) Long Acting and Permanent Methods of Contraception: Meeting clients’ needs.
- EngenderHealth (2003) Minilaparotomy for Female Sterilization: An Illustrated Guide for Service Providers.
- Philp T, Guillebaud J, Budd D (1984) Late failure of vasectomy after two documented analyses showing azoospermic semen. Br Med J (Clin Res Ed). 289(6437): 77-9.
- Denniston GC (1985) Vasectomy by electrocautery: outcomes in a series of 2,500 patients. J Fam Pract. 21(1):35-40.
- National Center for Health Statistics (2018) National Survey of Family Growth. Centers for Disease Control and Prevention.
- Central Statistical Agency (2012) Ethiopia Demographic and Health Survey. Ethiopia: ICF International Calverton.
- United Nations, Department of Economic and Social Affairs, Population Division. Trends in Contraceptive Use Worldwide 2015 (ST/ESA/SER.A/349) United Nations; 2015.
- Darroch JE, Sedgh G (2011) Contraceptive technologies: Responding to women’s needs.
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, et al. (2010) Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet. 375(9726): 1609-23.
- Igwe NM, Nnamdi EB, Jude AJ (2016) A 5-year clinical evaluation of subdermal implants among Abakaliki acceptors. J Basic Clin Reprod Sci. 5(1): 1-5.
- Igwe NM (2016) Intrauterine contraceptive devise use in Abakaliki, Southeast, Nigeria. 19(2): 138.
- Omu AE, Akagbosu F. Voluntary Surgical Contraception: attitudes, knowledge and practice. University of Benin Teaching Hospital studies. Trop J Obstet, Gynaecol. 1990 ;2: 220–226.
- Omu AE, Unuigbe JA (1985) The Pattern and attitude of Nigerian women in Benin City towards female sterilization. Asia Oceania J Obstet Gynecol. 11(1): 17–21.
- Dibaba A (2001) Rural men and their attitude towards vasectomy as a means of contraception in Ethiopia. Trop Doct. 31(2): 100– 2.
- Bunce A, Guest G, Searing H, Frajzyngier V, Riwa P, et al. (2007) Factors affecting vasectomy acceptability in Tanzania. Int Fam Plan Perspect. 33(1): 13–21.
- Odu OO, Ijadunola KT, Komolafe JO, Adebimpe WT (2006) Men's knowledge of and attitude with respect to family planning in a suburban Nigerian Community. Niger J Med. 15(3): 260–5.
- Okpere EE. Contraceptive knowledge, attitudes and behavior among Nigerian Males: Benin City and Udo. A survey sponsored by the office of population, United States Agency for International Development. 1988. [10 December 2009]. Available from: http://www.popline.org.
- Muhondwa E, Rutenberg N (1997) Population Council, Africa Operations Research and Technical Assistance project. USAID; Effects of the Vasectomy Promotion Project on Knowledge, attitudes, and behaviour among men in Dares Salaam, Tanzania.
- Adesiyun AG (2007) Female sterilization by tubal ligation a re- appraisal of factors influencing decision making in tropical setting. Archives of Gynecology and Obstetrics. 275(4): 241-4.
- Kabir M, Iliyasu Z, Abubakar IS, Maje BS (2003) The role of men in contraception decision making in Fanshelara village Northeastern Nigeria. Trop J Obstet Gynecol. 20(1): 24-27.
- Kana MA, Tangurum YO, Hassan ZI, Afolanranmi TO, Ogbeyi GO, et al. (2016) Prevalence and determinants of contraceptive use in rural Northeastern Nigeria; results of a mixed quantitative and qualitative assessment. Ann Nigerian Med. 10: 3-10.