Konan N’guessan1*, Harvey Attoh-Toure1, Antoine Droh3, Sidoine Konan2, Audrey Marie-Michelle Abina, Sam Ghislaine N’guessan, Kouadio Daniel Ekra
1National Institute of Public Hygiene, Abidjan, Côte d'Ivoire.
2National Blood Transfusion Center. Ivory Coast
3National Institute of Youth and Sports
*Corresponding Author: Konan N’guessan, National Institute of Public Hygiene, Abidjan, Côte d'Ivoire.
Abstract
The FSUCOM maternity ward of Yopougon roof red is faced with an unpleasant psychosocial experience for patients in the delivery room. The objective of this study was to understand the psychosocial experience of the patient in the delivery room.
Method
This was a cross-sectional study with a descriptive aim carried out over 1 month. The selection criteria allowed us to retain 98 patients.
Results
The survey included 98 participants including. The average age was 29.07, with extremes ranging from 16 to 43 years. An early [16-22] and late [37-43] maternity age group with respective proportions of 22% and 13%. The majority of our respondents (39%) were not educated, 33% had barely completed primary school and 68% were unemployed. Among the multiparous women encountered, almost 2/3 (63%) estimated that they had a negative obstetric memory. Around 2/3 (62%) were anxious, (69%) were distressed and (86%) had feelings of fear during their time in the delivery room. Fear of losing a child at 72%. More than half (52%) said they felt unsafe around staff and (62%) said they lacked emotional support from the professionals who cared for them.
Conclusion
The psychosocial experience of the patient at the FSUCOM maternity ward of Yopougon roof rouge was negative. Childbirth professionals must be guarantors of the physical and psychological well-being of patients in order to allow them to have a good time.
Keywords: Experienced-Psychosocial-Patient; Delivery room ; Cote d’Ivoire
Introduction
Psychosocial experience is subjective and can be perceived as the way in which a person experiences his or her interactions with those of his or her social environment [1]. The world of the delivery room and all the experience that takes place there are exclusively the prerogative of animators (patients, childbirth professionals, any inert object). During our time in the delivery room, we were given the opportunity to observe agitation, dyspnea and tachycardia in most of the patients in the said room. When questioned, some expressed feelings of anxiety, stress and fear. This psychosocial atmosphere is maintained in part, in the opinion of some patients, by the less courteous and less communicative attitude of the professionals in the room delivery towards the patients.
For all women, the birth of a child is a wonderful but emotionally upsetting event. It is also described as a potentially stressful event in their lives. An author such as Szejer in the USA addresses, in his book, all the feelings that women can experience during childbirth [2]). Women can be anxious, panicked, frightened in the face of certain life situations that can be found during childbirth such as pain, death of the child and/or mother. They may also feel a certain stress, a certain pressure during this event which is important and not negligible in their lives [2].
The delivery room is an alienating environment for many women where institutional routines such as systematic undressing on arrival, lack of privacy, will dispossess some patients of their sense of intimacy as described in the United Kingdom by Creedy et al in 2000 [3]. The anxiety caused by the loss of their sense of control can interfere with the normal course of childbirth [3]. Simkin in 1990 in the USA reports that the patient's feeling of having control or not determines the positive or negative memory of the birth [4].
In our African societies, rites, prayers, sacrifices and oracle consultations surround major events such as the birth of a woman. These practices reassure the individual and families and reduce worry, anxiety and various fears related to childbirth [5]. A Senegalese study comparing traditional and modern childbirth concluded that patients giving birth traditionally were well surrounded by their mothers, sisters, and cousins who took care of them [6].
In Côte d'Ivoire, the recent events that have shaken the world of delivery rooms, even going so far as to the death of some patients, including that of Adzopé and the Cocody University Hospital among others, have left no one indifferent. The country's authorities have taken measures to improve their situation in maternity wards, such as increasing the number of midwifery students, creating the midwifery sector, building maternity wards, and renewing and increasing beds in delivery rooms and maternity wards. The construction of a mother- child centre in Bingerville and at the Cocody University Hospital, to name but a few. However, these salutary measures seem not to have taken into account all aspects such as those relating to the psychosocial experience of the patient in the delivery room. In our tropics, in the academic field, it remains insufficiently explored and this is where our study finds all its interest. Although the "psychosocial experience" has been addressed in some studies from other aspects. In particular, "the psychosocial experience of men declared infertile in patients followed in andrological consultations at the Cocody University Hospital" [7].
Whereas the ideal would be end-to-end, heart-to-heart assistance in order to protect patients from anguish, anxiety and stress for a more humanized delivery. And this is what Lewin calls the "psychological field" when he says that human behaviour is always part of a well- defined environment [8].
This study is based on the conception of nursing care which reports that the person is a whole with fourteen basic needs [9].
To conduct our study properly, we asked ourselves the question of: What is the psychosocial experience of the patient in the delivery room at the FSUCOM in Yopougon toit rouge?
Our work, pursuing the objectives below, is based on the hypothesis that the psychosocial experience of the patient in the delivery room is linked to interactions with the facilitators of this particular social environment.
To conduct our study properly, we asked ourselves the question: What is the psychosocial experience of the patient in the delivery room at the FSUCOM of Yopougon toit rouge?
The overall objective of our work is to do so. To understand the psychosocial experience of the patient in the delivery room at the Urban Community Health Training (FSUCOM) of Yopougon red roof.
Specific objectives
1. Describe the sociodemographic characteristics of the patient in the delivery room of the FSUCOM of Yopougon toit rouge,
2. Identify the personal feelings of the patient in the delivery room of the FSUCOM of Yopougon toit rouge (joy, trust, fear, anguish, anxiety).
Materials and Methods
Type and period of study
This was a cross-sectional study with a descriptive purpose. It took place from November 22 to December 22, 2023
Scope of the study
Our study framework is the Yopougon Community Urban Health Facility red-roofed of the Yopougon East health district. The FSUCOM toit rouge is the first centre born of Ivorian-French cooperation within the framework of the Abidjan Santé Project (PSA). It is managed privately and non-profit-making by an association from the populations (AFOSUC) which is linked to the Ivorian State by a public service agreement. The center covers a health area of 88854 inhabitants. The medical activity is led by a medical and paramedical team headed by a chief physician supported in his task by a deputy chief physician and a supervisor of the care units (SUS) who work closely together to guarantee the quality of care provided to patients.
Study Location
The location chosen for this study is the FSUCOM toit rouge in the commune of Yopougon, located in the west of the district of Abidjan. Yopougon has two health districts, including Yopougon East and Yopougon West. In terms of health infrastructure, the municipality has a university hospital under rehabilitation, two (02) general hospitals and ten (10) community-based urban health facilities, including the one where our study is taking place. The delivery room has four (4) beds separated by front beds. The delivery room service is open 24 hours a day, 7 days a day.
Study population
Our study population consisted of patients using or having used the delivery room of the FSUCOM in Yopougon toit rouge.
Selection criteria
Inclusion criteria
To be part of our study, you have to be in the delivery room,
1. Have given birth less than 6 weeks ago,
2. Agree to participate in the study,
3. To be in possession of one's mental faculties.
Non-inclusion criteria
Not included in the study
1. patients who do not understand and do not speak the French language,
2. Those refusing to participate in the study,
3. Those who gave birth more than 6 weeks ago.
Dependent variable
Psychosocial experience of the patient.
Independent variables
Sociodemographic variables of the patient using the delivery department of the FSUCOM of Yopougon toit rouge.
1. Age
2. Level of education (not in school/ primary/secondary/tertiary)
3. Marital status (married/cohabiting/single/divorced)
4. Occupation (non-occupation/middle manager/senior manager)
5. Gestient (primiges/multi-gesture)
6. Parité (primiparous/multiparous)
7. Obstetric history of multiparous women (negative/positive)
8. Type of focus (monogamous/polygamous)
Variables related to the patient's personal feelings
1. Anxious (yes/no)
2. Fear of the outcome of childbirth
3. Reasons for fear
4. Confidence in the delivery room staff
5. Joy of giving birth
Sampling method
In the present study, since we do not have a sampling frame or knowledge of the probability that each individual in the patient population will be included in the sample, we propose to do a non- probability sampling.
Technique and sample size
To constitute our total survey population, we used the simple random technique of all patients who used the delivery room of the FSUCOM Yopougon toit rouge for the duration of our study and this in accordance with our inclusion criteria. So we worked with a total of 98 patients.
Data collection technique and tools
The technique adopted for the collection of data for our study is based on individual interviews with patients.
Data analysis
Data were entered using Word 2010 and then analyzed using Excel 2010 and Epi info 7.2.5.0
Results
Sociodemographic characteristics of the patient received in the delivery department of the (FSUCOM) of Yopougon toit rouge.
1. The dominant age group was [23-29] years old with a proportion of 35%. The average age was 29.07, with the extremes ranging from 16 to 43. There is also an age group of early [16-22] and late [37-43] motherhood, with proportions of 22% and 13% respectively.
2. Most of our respondents (39%) were not in school and (33%) had barely passed the primary level.
3. Among our respondents were single (30%) or cohabiting (36%).
4. More than 2/3 of the patients (68%) of our respondents were without a profession.
5. Of the patients surveyed, 3/4 (74) % had had more than one pregnancy (multi-procedure).
6. About 3/4 (74%) of patients had more than one delivery.
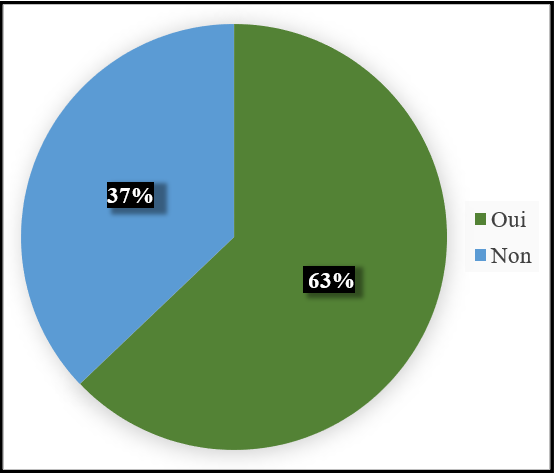
7. Of all multiparous women, nearly 2/3 (63%) felt that they had a bad obstetric memory.
8. Separated patients were predominant (60%).
Variables related to the patient's personal feelings
1. Nearly 2/3 (62%) of patients said that they were anxious during their time in the delivery room.
2. Among the respondents, more than 2/3 were anxious (69%) during their stay in the delivery room.
3. The feeling of confidence was reported at a proportion of (63%) among our respondents.
4. Among our respondents, the feeling of joy in giving birth was reported in a proportion of (68%).
5. More than 4/5 (86%) of the patients surveyed said they felt afraid about the outcome of the delivery room when they went to the delivery room.
Of all the reasons for fear, the risk of bleeding after childbirth and loss of the baby was widely mentioned in proportions of (85%) and (72%) of the.
Figure 1: Distribution of patients according to their feeling of anxiety
Figure 2: Distribution of respondents according to their feeling of anxiety
Figure 3: Distribution of patients according to their sense of confidence in the Delivery room staff
Table I: Epidemiological profile of patients
|
Age Range (Years) |
Absolute value |
Proportion (%) |
|
[16; 22] |
22 |
22 |
|
[23; 29] |
34 |
35 |
|
[30; 36] |
29 |
30 |
|
[37; 43] |
13 |
13 |
|
Level of study |
||
|
Not in school |
38 |
39 |
|
primary |
31 |
32 |
|
Secondary |
21 |
21 |
|
Upper |
08 |
08 |
|
Marital status |
||
|
Married |
26 |
26 |
|
Divorced |
09 |
09 |
|
Cohabitation |
34 |
35 |
|
Single |
29 |
30 |
|
Profession |
||
|
No profession |
67 |
68 |
|
Senior Executive |
11 |
11 |
|
Middle management |
21 |
21 |
|
Gesturity |
||
|
Multi-gesture |
73 |
74 |
|
Primigeste |
25 |
26 |
|
Parity |
||
|
Multiparous |
73 |
74 |
|
Primiparous |
25 |
26 |
|
Multi-pair patients |
Positive |
Negative |
|
|
37 |
63 |
|
Type of fireplace |
Absolute value |
Proportion |
|
Monogames |
17 |
17 |
|
Polygames |
23 |
23 |
|
Separate |
59 |
60 |
Table II: Distribution of patients according to the reason for the fear expressed N=98
|
Reasons for fear |
Frequency |
Percentage |
|
Bleeding after childbirth |
83 |
85% |
|
Death of the child |
71 |
72% |
|
Being evacuated for complications |
50 |
51% |
|
Stillborn child |
48 |
49% |
|
High expenses |
46 |
47% |
|
Traumatic injuries |
44 |
45% |
|
Unknown personnel |
43 |
44% |
|
Embarrassed by the gaze of others |
36 |
37% |
|
Suffering without being listened to |
36 |
37% |
|
Have a caesarean section |
32 |
33% |
|
Inability to cope with the pain of childbirth |
30 |
31% |
|
The idea of giving birth again |
25 |
26% |
|
Malformed child |
24 |
24% |
|
Infection in newborns |
19 |
19% |
|
Child of unwanted sex |
13 |
13% |
Discussion
In our study, the dominant age group was [23-29] years old with a proportion of 35%. The average age was 29.07, with extremes ranging from 16 to 43 years. We also report an age range of early [16-22] years and late [37-43] motherhood with proportions of 22% and 13% respectively. Our results are substantially similar to those of Obossou et al in Benin in (2017) who reported an average age of 27 years.
Nearly 2/3 (63%) of patients felt that they had a negative obstetric memory. Our results do not corroborate those of Guittier conducted in France in 2018 [10]. This author reported only 6% of multiparous patients who reported having had a bad experience with the aspects of childbirth. This finding of negative obstetric memory, synonymous with a negative psychosocial experience, is linked to the physical trauma (episiotomy, caesarean section) and psychological trauma (loss of the baby) that women experience during their time in the delivery room. Our results reported that (62%), or nearly 2/3 of our respondents, said they had been anxious during their time in the delivery room. Our results are similar to those of studies conducted in the USA and France [11]. Indeed, Ford et al showed in their 2008 studies in the USA that 61% of patients were anxious in the delivery room [11]. Also, in France, Blondeau et al (2012) showed that 57.5% of patients in the delivery room were also anxious [12]. The anxiety observed in patients could be explained by the feeling of fear that is largely regained and also by the fact that women are vulnerable beings, they are more prone to the emotions that they could easily be led to. In addition, many pregnant women who went to the delivery room lived apart from their spouses. This situation could lead to a feeling of loneliness and lead to the anxiety observed, consequently a negative psychosocial experience.
In our study, we found that more than 2/3 of the respondents were anxious, i.e. 69%, during their stay in the delivery room. Our results are contrary to those of Obossou et al in 2017 in Benin who reported that 23% of patients had confessed to being anxious [13]. This difference in the percentage of our results and those of Obossou could be explained by the fact that our survey took place in a single health centre.
More than 4/5 (86%) of the patients surveyed said they felt fear when they went to the delivery room. Our results do not corroborate those of Songül Aktaş (2018) in Turkey who reported that a proportion of 27% of patients were fearful [14]. Also, Smarandache et al (2016) in Canada reported a proportion of 13% of fearful patients [15]. Our results could be explained by the absence of sessions to prepare patients for childbirth. We have also reported an early and late age of motherhood among our patients. This could promote fear in both first- time and multiparous women.
Of all the reasons for fear, the risk of bleeding after childbirth (85%) and loss of the child (72%) were widely mentioned by patients. In contrast to our study, Obossou et al (2017) in Benin found the health status of the newborn (76%), the maternal condition (64%), and the high cost of care (61%) as reasons for fear [10]. Blondeau et al (2012) in France had found as reasons, the fear of giving birth to a stillbirth (40%), fear of maternal death during childbirth (25%), fear of caesarean section (23%), fear of newborn malformation (17%) [12]. Our results could be explained by a negative experience of the birth of the patient or a relative. We should also note the prejudices surrounding childbirth in our communities and those conveyed about the staff in the delivery room. Another explanation could come from the lack of psychological preparation of pregnant women before childbirth.
Of all the patients surveyed, more than half (52%) said they did not feel safe with the staff. Our results corroborate those of Oboro (2011) in Nigeria who found that 61% of women who came to give birth asked for at least one relative because they did not feel safe with the staff [16]. On the other hand, Aktaş (2018) in Turkey in his study found a significantly lower proportion (18%) [14].
In our study, the high rate of patients who felt unsafe may be explained by the absence of their loved one at the time of delivery or by a lack of psychological preparation.
Of all our respondents, 62% said they lacked emotional support from the professionals who cared for them. In contrast, the study by Hollander et al in 2017 showed that only 8.1% of the women surveyed stressed that they lacked emotional support [17]. Henriksen et al in their 2017 study showed that women in the delivery room who did not receive emotional support had a significantly higher prevalence and negative childbirth experience [18]. Analyzing closely, we can say that the lack of emotional support from midwife staff could be explained by the fact that they who have to take care of several patients at the same time, do not have the material time to listen exclusively to each patient.
Not all the events surrounding childbirth were identified by (77%) of patients, as shown in our study. Our results are corroborated by Elmir et al en (2010) who showed in their study that 53% of patients did not understand what was happening around them [19]. The conclusion is that of a lack of communication which is a factor leading to a potentially traumatic experience. In the same vein, Hollander et al in 2017 reported that 43.7% of women surveyed attributed their trauma to a lack of communication [17]. This misunderstanding of the events during childbirth could be explained by the fact that the healthcare staff do not clearly explain the course of the birth.
Conclusion
Our work consisted of the study of the psychosocial experience of the patient in the delivery room at the FSUCOM of Yopougon toit rouge. The objective was to understand the psychosocial experience of the patient of the said structure. Our results showed an early and late age range of motherhood. These two aspects, early motherhood and late motherhood, could negatively influence the psychosocial experience of patients in the delivery room. Most patients were not in school or had barely passed the primary level. Many of our respondents were unemployed, and in the multiparous population, many reported having a negative obstetric memory.
Thanks
We would like to thank the administrative and health officials and all the staff of the community-based health facility of Yopougon Toit Rouge.
Ethical consideration
Administrative authorization
An investigation authorization from the (Directorate of Health Establishments and Health Profession) DEPS has been issued to us. With this document, we sent a request for authorization of investigation to the Departmental Director of Health of the Yopougon health district who accepted it. Then another authorization that we addressed to the management of the FSUCOM of Yopougon toit rouge which in turn accepted it.
Conflicts of Interest: No conflict of interest is to be reported.
References
- Riazuelo H (2017) Chapter 2. The psychic work of pregnancy. In: 35 grandes notions de Périnatalité. Paris: Dunod. pp. 63–151.
- Szejer M, Stewart R, Lambrichs LL, Frydman RP. Those nine months: a psychoanalytic approach to pregnancy and birth. Paris, France: Robert Laffont; 2002. 310 p.
- Creedy DK, Shochet IM, Horsfall J (2000) Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth. 27(2): 104–11.
- Simkin P (1992) Just another day in a woman’s life? Part II: Nature and consistency of women’s long-term memories of their first birth experiences. Birth. 19(2): 64–81.
- Jacques B (2008) Sociologie de l’accouchement.
- Royer M (1998) Conceiving and Born. give birth in Africa, give birth in France. Les cahiers de l'URACA N°9. 1998.
- Bony ES, Bokossa ME (2006) Male infertility at the chu of cocody about 280 cases andrological consultations.
- Lewin. Lewin's force field theory. In: Social Psychology. 2010.
- Rebelo Marques K, Dall'Armellina L (2018) What midwifery support in the delivery room promotes a good childbirth experience?.
- Guittier M-J (2018) Assessing the experience of childbirth. France. 16–22.
- Ford E, Ayers S (2009) Stressful events and support during birth: the effect on anxiety, mood and perceived control. J Anxiety Disord. 23(2): 260–8.
- Blondeau M (2012) Experience of the delivery room by patients belonging to a health profession. 103.
- Obossou A, Salifou K, Aboubakar M, Ahouingnan F, Bagnan A, et al. (2017) Psychological experience of the patient in the delivery room at the maternity ward of the Borgou Departmental and University Hospital Center in Parakou (BENIN). European Scientific Journal, ESJ. 13(21): 407.
- Aktaş S, Aydın R (2019) The analysis of negative birth experiences of mothers: a qualitative study. J Reprod Infant Psychol. 37(2): 176–92.
- Smarandache A, Kim THM, Bohr Y, Tamim H (2016) Predictors of a negative labour and birth experience based on a national survey of Canadian women. BMC Pregnancy and Childbirth. 16(1): 114.
- Oboro VO, Oyeniran AO, Akinola SE, Isawumi AI (2011) Attitudes of Nigerian women toward the presence of their husband or partner as a support person during labor. Int J Gynaecol Obstet. 112(1): 56–8.
- Hollander MH, van Hastenberg E, van Dillen J, van Pampus MG, de Miranda E, et al. (2017) Preventing traumatic childbirth experiences: 2192 women’s perceptions and views. Arch Womens Ment Health. 20(4): 515–523.
- Henriksen L, Grimsrud E, Schei B, Lukasse M, Bidens Study Group. (2017) Factors related to a negative birth experience - A mixed methods study. Midwifery. 51: 33–39.
- Elmir R, Schmied V, Wilkes L, Jackson D (2010) Women’s perceptions and experiences of a traumatic birth: a meta- ethnography. J Adv Nurs. 66(10): 2142–53.