Abderrahmane Housni1*, Badr Rouijel2, Sofia Elakroud1, Mamoune El Mostarchid1, Freshnel Obam1, Ettayebi Fouad2, Elouahabi Abdessamad3
1Military Hospital Mohamed V of Rabat, Morocco.
2Hopital D'enfant Rabat, Morocco.
3Hopital des spécialités ONO Rabat
*Corresponding Author: Abderrahmane Housni, Military Hospital Mohamed V of Rabat, Morocco.
Abstract
We report here a case of a 4-year-old girl, who spontaneously presented severe torticollis, we have discovered by a CT scan a dislocation of the axis and the atlas, and we have reduced the dislocation under sedation, and have got good control.
Introduction
Spontaneous atlantoaxial subluxation is a rare cause of hard torticollis, It can happen in the context of viral infection as ORL, or post-traumatic. It is often taken for opisthotonos, this case needs a good analysis of the situation as a complete physical examination, adequate radiography, and quick treatment.
Case Report
A 4-year-old girl was admitted to the emergency of the pediatric hospital with a history that one month earlier she had woken up with a stiff neck, and torticollis, with no notion of trauma or infection before. At first, her family took her to a generalist who prescribed some analgesics. One week later the patient had not improved, so the family came to the emergency department of the pediatric hospital. At her admission, the child was apyretic, conscious, GCS 15, she had irreducible torticollis, and her head was turned to the left side. She had severe right-sided torticollis, she also had a spasm of the sternocleidomastoid muscle, and there was no evident neurologic deficit.
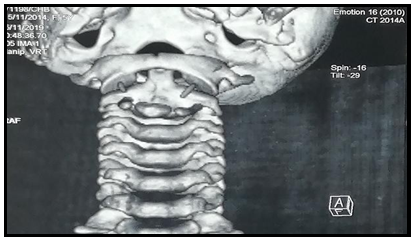
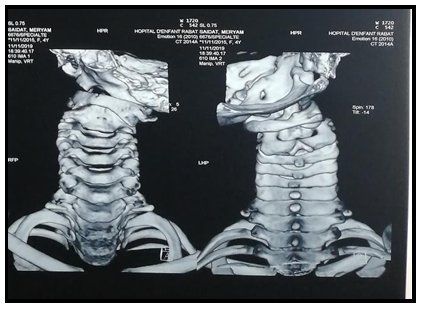
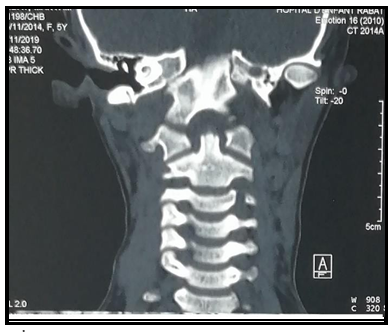
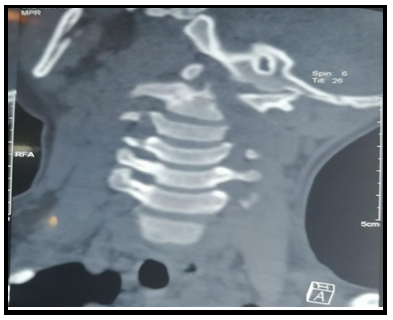
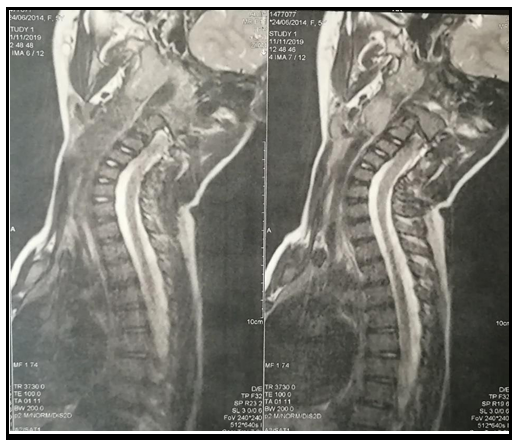
In front of the history of the patient, and the medication that she had already taken, we have done immediately a CT scan and an MRI that had shown a subluxation of the axis and the atlas (figure 1, figure 2, figure 3). We could not individualize any abscess. There were no spinal, ligament, or muscular injuries. The blood standard test was normal.
Figure 1: 3D reconstruction show the subluxaion and control after reduction
Figure 2: Ct scan shown the atlanto axial subluxation
Under sedation, our team realized a successful reduction of the dislocation that was confirmed by a CT scan (figure 4, figure 5). The position of the neck was fixed by a 3 kg traction for 4 days. The family and the medical staff were informed to minimize the mobilization of the patient in order to get the best results.
Figure 3: MRI shown the subluxatiion
After removing the traction, we stabilized the child’s neck in a neutral position by a Philadelphia collar for 2 months. Some analgesics were also prescribed. At last, the pain disappeared, and the mobilization of the neck was normal.
Discussion
In 1830, Bell described the first case of atlantoaxial rotatory subluxation for a syphilitic patient with pharyngeal ulceration [1] since that, multiple authors report some cases of pediatric spontaneous atlantoaxial subluxation, but the mechanism remains incompletely understood.
Typically, the patient is about 4 years old with a sex ratio of 1 and suffering from torticollis for about 2 weeks. Usually, it can be the second or third consultation. The first sign is the torticollis, then limited movement, and in some rare cases, the child can only feel a little neck discomfort [2].
Every child with torticollis should be carefully examined. The child’s physical exam usually shows no neurologic deficit, but typically the head is tilted to one side and rotated to the opposite side which is called Cock Robin position. A muscle spasm is often found because it tried to correct the position of the head. Also, limited neck motion is found. The child’s consciousness is generally conserved. The rest of the physical examination is usually normal. However, pediatricians should eliminate an upper respiratory infection, the notion of trauma, mistreatment, or inflammation in a child’s history.
In front of a child who suffers from neck pain, and a Cock Robin position, physicians should have a suspicion of atlantoaxial rotatory subluxation, and must realize some imagery. The radiographic exam must include conventional radiography respecting anteroposterior, lateral, and odontoid views, also, dynamic incidence can be very useful.
CT scan is the gold standard for atlantoaxial rotatory subluxation diagnosis. It helps to confirm the diagnosis and find out a bone fracture or bony abnormality, the subluxation, and to classify the subluxation. [2,3]
An MRI can be realized later and helps to determine some laxity, ligament or abnormalities, or abscess. Biologic exams are also important in order to eliminate an infection (especially ORL).
Multiple authors tried to explain the mechanism of the subluxation. First of all, we need to understand the normal anatomy, the natural position of the atlantoaxial complex is guaranteed by facet joint capsules, spinal ligaments, and the articulations surfaces. The facet joints at C1 and C2 are also shallow and more horizontally oriented for children, allowing more motion [4] then we can say that upper cervical bones and joints are intrinsically unstable. [5], however, some congenital laxity can explain the predisposition of some children to have an atlantoaxial rotatory subluxation as described by G. Thouassa, who had reported 3 cases of AAR for children with trisomy 21 [5] Grisel’s syndrome was also often described in the literature as an AAR, developed after an upper respiratory infection, probably due to hyperemia of soft tissues around the atlantoaxial complex, sometimes favored by a minimal trauma-7- there is also some association between juvenile rheumatoid arthritis and congenital ligamentous laxity, which can often cause a SAAR as reported by Sullivan CR [7].
The management of SAAR must be urgent, and diagnosis must not delay the treatment.
If the atlantoaxial rotatory subluxation had been discovered early less than one week, probably only a medical treatment, associated with some rest and simple immobilization would be enough. However, if it is not sufficient, or the diagnosis was a little late (less than one month), we can proceed to a reduction associated with a collar for about six weeks. If recurrence, we can try again an immobilization but longer this time for about 3 months-2-surgical option is maintained as the last option, especially, posterior surgical in some specific cases as a failure of the orthopedic treatment, recurrences, and neurologic involvement [6,7]
Conclusion
Torticollis is a common affection in childhood. Practicians should be aware of potential atlantoaxial rotatory subluxation, especially in predisposition cases. They have to know that early diagnosis and quick treatment can offer better chances for orthopedic treatment and can minimize risks for surgery to avoid chronic deformity.
References
- Charles B (1830) The nervous system of the human body,embracing the paper delivred to the royal society on the subject of nerves. Case 143; 403.
- Sferopoulos NK (2018) Atlantoaxial rotatory subluxation in children: A review. J Radiol Med Imaging. 2: 1009
- Fielding JW, Stillwell WT, Chynn KY, Spyropoulos EC (1978) Use of computed tomography for the diagnosis of atlanto-axial rotatory fixed. A case reports. J Bone Joint Surg Am. 60(8): 1102- 1104.
- Charles S, Millbrandt T, Gelb D, Ludwig SC (2005) The Management of Pediatric Cervical Spine Injuries. Seminars in Spine Surgery. 17(2): 95-99.
- Thouassa G, Bouare F, Laghmari M, Lmejjati M, Ghannane H, et al. (2018) Luxation atlanto-axoïdienne spontanée et trisomie 21, à propos d’une observation dans le service de neurochirurgie, CHU Mohammed VI, université Cadi-Ayyad, Marrakech. Neurochirurgie. 64(3): 255.
- Crossman JE, Thompson D, Hayward RD, Ransford AO, Crockard HA (2004) Recurrent atlantoaxial rotatory fixation in children: a rare complication of a rare condition. Report of four cases. J Neurosurg. 100(3 Suppl Spine): 307-311.
- Crossman JE, David K, Hayward R, Crockard HA (2004) Open reduction of pediatric atlantoaxial rotatory fixation: long-term outcome study with functional measurements. J Neurosurg. 100(3 Suppl Spine): 235-240.