Shahaboddin Dolatkhah1, Farhad Zamani2, Fatemeh Farhang3, Ali Zare Mehrjerdi4, Mehdi Nikkhah2*
1Department of Internal Medicine, Iran University of Medical Sciences, Tehran, Iran.
2Gastrointestinal and Liver Diseases Research Center, Iran University of Medical Sciences, Tehran, Iran.
3Department of Pathology, Imam Khomeini Hospital Complex, Tehran, Iran.
4Department of Pathology, Iran University of Medical Sciences, Tehran, Iran.
*Corresponding Author: Mehdi Nikkhah, Gastrointestinal and Liver Diseases Research Center, Iran University of Medical Sciences, Tehran, Iran.
Abstract
Solitary Peutz-Jeghers type polyps are categorized as hamartomatous polyps without evidence of mucocutaneous pigmentation, family history of JPS, and in the absence of mutation of the STK11/LKB-1 gene Introduction. Here in, we report an 80-year-old female who was presented with epigastric pain and early satiety six months ago. Esophagus-gastro duodenoscopy showed a single sizeable sessile polyp sized 35x30 mm without bleeding in the duodenal bulb. Pathologic assessment of the specimen revealed a diagnosis of "Hamartomatous polyp," which is regarded as a rare polyp in the absence of Peuthz-Jeghers syndrome.
Introduction
Hamartomatous polyps are rare lesions that may not present with specific symptoms and could be found as an incidental endoscopic finding [1]. These polyps could be a part of Peutz-Jeghers syndrome (JPS) or present in the absence of other clinical results of JPS.
Although most hamartomatous polyps are benign lesions with a good prognosis, there are some case reports of hamartomatous polyp-aroused adenocarcinoma, which considers that all hamartomatous polyps should be removed and sent for pathologic evaluation [2].
Case report
Here, we report an 80-year-old female with a medical history of hypertension and duodenal ulcer (diagnosed twenty-one years ago) who presented with epigastric pain and early satiety six months ago. Epigastric pain was accompanied by heartburn, especially after meal eating, but there was no history of fever, jaundice, or weight loss months ago. Drug history included Amlodipine 5 mg daily and pantoprazole 40 mg daily. On physical examination, slightly increased systolic blood pressure (135 mmHg) and an epigastric located with mild tenderness on deep pressure were identified, but there were no significant pathologic findings, including fever, supraclavicular lymphadenopathy, palpable mass, or organomegaly. Routine blood biochemistry and blood cell count revealed a mildly elevated fasting plasma glucose (112 mg/dl), while other tests, including liver function tests, were unremarkable. The abdominopelvic ultra-sonographic study showed an increased hepatic echogenicity consistent with fatty liver grade 1, normal gallbladder and biliary tract (common bile duct:4.5 mm), normal pancreas and spleen (span:83mm), and a 5x4 mm diverticula located in abdominal left lower quadrant which was consistent with diverticulitis. Further abdominopelvic computerized tomography scan with intravenous and oral contrast revealed sigmoid and left colon diverticulitis, while other findings were unremarkable.
Esophagus-gastro duodenoscopy showed a single sizeable sessile polyp sized 35x30 mm without bleeding in the duodenal bulb (Figure 1). Piecemeal polypectomy by hot snare was performed in the duodenal bulb. Before polypectomy, 10 ml of dilated epinephrine was injected into the polyp's base. The polyp was retrieved completely, and successful clipping was performed (Figure 2).
Figure 1: duodenal bulb polyp
Figure 2: clipping the polyp site
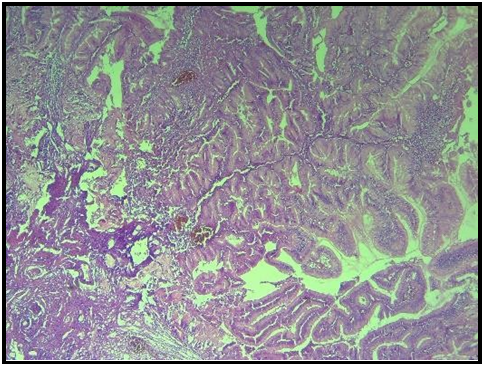
Pathologic evaluation of the specimen showed a core of smooth muscle tissue with tree-like branching of smooth muscle fibers covered by hyperplastic duodenal mucosa (Figure 3 and Figure 4)
Figure 3: Hamartomatous polyp showing the characteristics overgrowth of epithelium and an arborizing smooth muscle core.
Figure 4: the overlying mucosa is typically non-dysplastic and maintains its normal architecture
Eight months follow up of the patient revealed no recurrent symptoms and no complications.
Discussion
Solitary Peutz-Jeghers type polyps are categorized as hamartomatous polyps without evidence of mucocutaneous pigmentation, family history of JPS, and in the absence of mutation of the STK11/LKB-1 gene [3]. These polyps would appear as pedunculated, semi-pedunculated, or sessile polyps and may also be found in unusual areas such as the appendix [4]. There are only a few reports of mentioned polyps; most of them were diagnosed by endoscopy incidentally. A previous review of the literature showed that most patients with sporadic duodenal hamartomatous polyps are identified in the fifth or sixth decade of their life, while our case had a diagnosis of the mentioned lesion in the ninth decade of her life [1].
The risk of malignant transformation of the gastrointestinal tract in JPS is higher than in the general population. It's better to say that solitary Peutz-Jeghers-type polyps also risk malignant transformation [5], and accurate pathologic evaluation is recommended.
Conclusion
Like previous reports, our case had a history of upper gastrointestinal complaints, and the polyp was identified during the endoscopy.
During upper endoscopy, it's better not to exclude the "hamartomatous polyp" diagnosis in the absence of other presentations of JPS.
References
- Acea Nebril B, Taboada Filgueira L, Parajó Calvo A, Gayoso García R, Gómez Rodríguez D, et al. (1993) Solitary hamartomatous duodenal polyp; a different entity: Report of a case and review of the literature. Surgery Today. 23(12): 1074-7.
- Suzuki S, Hirasaki S, Ikeda F, Yumoto E, Yamane H, et al. (2008) Three cases of Solitary Peutz-Jeghers-type hamartomatous polyp in the duodenum. World Journal of Gastroenterology: WJG. 14(6): 944-7.
- Rathi CD, Solanke DB, Kabra NL, Ingle MA, Sawant PD (2016) A Rare Case of Solitary Peutz Jeghers Type Hamartomatous Duodenal Polyp with Dysplasia! J Clin Diagn Res. 10(7): OD03- OD4.
- Nozoe T, Mori E, Iguchi T, Kohno M, Maeda T, et al. (2013) Pedunculated hamartomatous polyp of the appendix: report of a case. Surgery Today. 43(2): 191-3.
- Sekino Y, Inamori M, Hirai M, Suzuki K, Tsuzawa K, et al. (2011) Solitary Peutz-Jeghers type hamartomatous polyps in the duodenum are not always associated with a low risk of cancer: two case reports. Journal of Medical Case Reports. 5(1): 240.