Weng Kong Low1*, Rohaman Tasarib2, Ashraf Hakim Ab Halim3, Abdul Rauf Ahmad1
1Department of Orthopaedic, Hospital Tuanku Ja’afar, Jalan Rasah, Bukit Rasah, 70300 Seremban, Negeri Sembilan
2An-Nur Specialist Hospital, Jalan Gerbang Wawasan 1, Seksyen 15, 43650 Bandar Baru Bangi, Selangor
3University Putra Malaysia, Jalan University 1, Serdang, 43400 Seri Kembangan, Selangor
*Corresponding Author: Weng Kong Low, Department of Orthopaedic, Hospital Tuanku Ja’afar, Jalan Rasah, Bukit Rasah, 70300 Seremban, Negeri Sembilan
Abstract
Complex femur malunion has always been a challenge to orthopedic surgeons. We performed a study to assess the clinical and radiological outcome of complex femur deformity correction using Ortho-SUV in our center. A total of 13 patients were included in this study. For radiological outcomes, 10 patients were graded as excellent and 3 patients were graded as well based on the ASAMI criteria. For functional outcomes, 9 patients were graded as excellent and 4 patients were graded as well based on ASAMI criteria. Osteomyelitis, thigh abscess, pin site infection, and knee stiffness were amongst the complications reported in this study. In conclusion, we would recommend the use of the Ortho-SUV Frame as a single-step correction technique for complex femoral deformity correction.
Keywords: Complex femur malunion, femoral deformity, gradual deformity correction, Ortho-SUV frame, ASAMI criteria
Introduction
Complex femur malunion has always been a challenge to orthopedic surgeons. If left untreated, it may lead to the abnormal mechanical axis of lower limb and limb length discrepancy [1]. This may in turn lead to abnormal mechanical loading on the nearby hip and knee joint, causing early osteoarthritis of the involved joints. Correction of a complex femur malunion, either by acute or gradual method, requires detailed planning. Deformities in all the planes need to be addressed accurately in order to achieve a satisfactory outcome.
Conventionally, gradual correction of complex deformity was performed using Ilizarov external fixator. However, this method often requires frequent modification of the frame for sequential correction of angulation, lengthening, translation, and rotation in different stages. This led to a prolonged duration of correction period [2] and a long period on the Ilizarov external fixator. However, this issue was overcome by the introduction of the newer computer-assisted hexapod system that can perform single-step correction for complex deformities.
The objection of this study is to assess the clinical and radiological outcome for complex femur malunion correction using a computer-assisted hexapod external fixator (Ortho-SUV frame).
Materials and methods
We conducted a cross-sectional retrospective study to review the outcome and complications that arise in the patients with femur malunion, who underwent gradual femur deformity correction using Ortho-SUV frame from the year 2016 to 2018 in our center. All the cases were performed by the second author in this study.
1. Procedure:
Preoperative plain radiographs including lower limb axis view were obtained to delineate the deviation of the mechanical and anatomical axis caused by the malunion, as well as for preoperative planning for the deformity correction and templating for the Ortho-SUV frame application.
All 13 patients in this study underwent surgery under spinal anesthesia. A standard Ortho-SUV frame construct of 2 ring levels (1 full ring and 1 femoral arch) with 4 Shantz pin fixation for the proximal segment and 2 ring levels with 5 fixations (combination of Shantz pins and wires) for the distal segment was applied for diaphysis deformity correction. For metaphysis deformity, 2 ring levels (1 full ring and 1 femoral arch) with 4 Shantz pin fixation for the proximal segment, and 1 ring level with 4 fixations (combination of Shantz pins and wires) for the distal segment were applied.
The specific post-operative anteroposterior and lateral radiographs of the femur were obtained immediately after the patient was discharged from the operation theatre. The radiographs were done under the supervision of the operating surgeon to ensure that all the parameters required by the computer correction software program were included.
Postoperatively, patients were started on non-weight bearing crutches ambulation, and motion exercises for the knee and hip joint within 48 hours once the pain is controlled. Patients were then discharged when ambulation is achieved.
Between day 10 to day 14 after surgery, patients were reviewed in the outpatient clinic where they were given the deformity correction schedule generated by the operating surgeon using the Ortho-SUV computer software. The technique of strut turning was taught to the patient or caretaker. The patient or caretaker was required to demonstrate the correct turning technique before being allowed home.
Patients were then followed up every 4 weekly for progress monitoring and strut reverse mode adjustment if required. The final anteroposterior and lateral radiograph were be obtained once the deformity correction was completed.
Modular transformation of the frame, to change the Ortho-SUV struts to the conventional threaded rod, was performed 2 weeks after completion of deformity correction. The 2 weeks window was to allow for callus consolidation at the deformity correction site to prevent loss of correction during the process of modular transformation. To accommodate for the non-parallel rings between the proximal and the distal segment, a triple hinge construct was used.
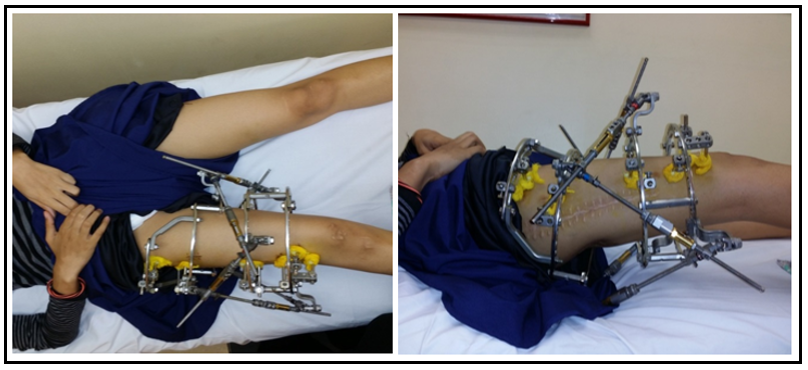
Following the modular transformation, the patient was allowed on full weight-bearing, and followed up every 6 weekly, until the osteotomy site was united. The Ortho-SUV frame was then removed. The clinical pictures of a case example are shown in Figure 1.
Figure 1: Clinical picture of the Ortho-SUV construct for one of the femur deformity correction case.
2. Radiological and functional assessment:
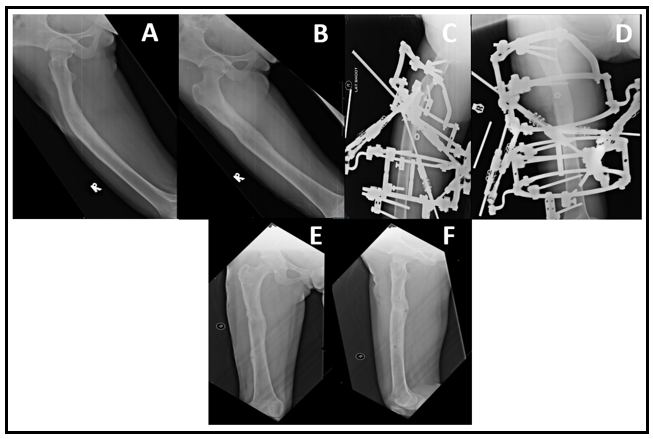
The radiological and functional assessments for each patient were done retrospectively based on the X-ray and clinical record on the last clinic review upon completion of treatment prior to discharge. The outcome was graded using Association for the Study and Application of Methods of Ilizarov (ASAMI) criteria [3]. The X-ray images preoperative, during correction on Ortho-SUV, and post-completion of correction of a case example are shown in Figure 2.
Figure 2: Preoperative X-ray showing the femoral deformity (A,B). X-ray showing femoral deformity post application of Ortho-SUV frame for gradual deformity correction (C,D). X-ray showing the corrected femoral deformity after removal of the Ortho-SUV construct (E,F).
Results
From May 2016 to June 2018, we performed 13 cases of complex femoral malunion correction using the Ortho-SUV hexapod system. Of the 13 patients, 10 were men and 3 were women. Their average age at the time of operation was 22.2-year-old (range 14 - 44-year-old). All 13 of them sustained a complex femoral deformity as a result of trauma. 11 of them had deformity involving the diaphysis and 2 involving the metaphysis of the femur. The two metaphyseal deformities were the result of premature epiphyseal closure secondary to the physis injury sustained during a trauma. While the eleven diaphyseal deformity resulted from fracture malunion. Causes of the complex femoral malunion were summarized in table 1.
All the patients achieve union at the end of their treatment. The mean time of injury to the time of application of Ortho-SUV frame was 186 weeks (range from 5 weeks to 29 years). The mean time in the frame was 39 weeks (range from 16 weeks to 81 weeks). Radiological and functional outcomes were graded using Association for the Study and Application of Methods of Ilizarov (ASAMI) criteria [3]. For radiological outcomes, 10 patients or 77 % were graded as excellent while 3 patients or 23 % were graded as good (Table 2). None of the patients in our series fall into the category of fair or poor. As for the functional outcomes, 9 patients or 69 % were graded as excellent, while 4 patients or 31 % were graded as good. None of the patients in our series were graded as fair, poor, or failed (Table 3).
In our series, we observed a total of 5 patients with pin site infection. One patient developed osteomyelitis as a sequela of pin tract infection. This patient required re-siting of the affected pin, surgical debridement, and a course of antibiotics. The second patient developed a superficial thigh abscess, requiring surgical drainage, and resolved after a course of antibiotics. The other 3 patients had mild superficial pin site infection which was resolved by increasing the frequency of dressing change at the affected pin site and a short course of preemptive antibiotics.
3 patients developed knee joint stiffness after removal of frame, despite undergoing intensive physiotherapy during the period on Ortho-SUV frame. The range of motion was limited at the range of 0 ° to 45° flexion.
Table 1: Demography of patients and causes of femur malunion
|
Cases (n) |
13 |
|
|
|
Mean age (year) |
22.2 |
(range 14-44 year) |
|
|
Gender |
Male |
10 |
|
|
Female |
3 |
|
|
|
Femur |
Left |
8 |
|
|
Right |
5 |
|
|
|
Location |
Diaphysis |
11 |
|
|
Metaphysis |
2 |
|
|
|
Causes of malunion |
Implant failure |
6 |
|
|
Alternative treatment |
3 |
|
|
|
Not suitable for surgery due to other medical illness |
2 |
|
|
|
Physical arrest |
2 |
|
Table 2: Radiological outcomes graded using Association for the Study and Application of Methods of Ilizarov (ASAMI) criteria
|
Radiological Score |
Description |
Number of patients |
|
Excellent |
Union, no infection, deformity < 7, limb length discrepency < 2.5cm |
10 |
|
Good |
Union + any two of the following: absence of infection, < 7 deformity and limb length inequality of < 2.5cm |
3 |
|
Fair |
Union + any one of the following: absence of infection, < 7 deformity and limb length inequality of < 2.5cm |
0 |
|
Poor |
Non union / refracture / union + infection + deformity > 7 + limb length inequality > 2.5 cm |
0 |
Table 3: Functional outcomes graded using Association for the Study and Application of Methods of Ilizarov (ASAMI) criteria
|
Functional Score |
Description |
Number of patients |
|
Excellent |
Active, no limp, minimum stiffness (loss of <15 knee extension / < 15 dorsiflexion of ankle), no reflex sympathetic dystrophy (RSD), insignificant pain |
9 |
|
Good |
Active, with one or two of the following: limp, stiffness, RSD, significant pain |
4 |
|
Fair |
Active, with three or all of the following: limp, stiffness, RSD, significant pain |
0 |
|
Poor |
Inactive (unemployment or inability to perform daily activities because of injury) |
0 |
|
Failure |
Amputation |
0 |
Discussion
A femur fracture is one of the commonest long bone fractures treated by an orthopedic surgeon. The worldwide incidence of femur shaft fracture has been reported to range between 10 and 21 per 100,000 every year [4]. Although the management of femur fracture has been well established, femoral malunion is not rare, especially in developing countries. This could be due to various reasons, including neglected fracture, loss of reduction after initial surgery, or poorly fixed fracture with residual deformity, commonly seen in comminuted fracture. Regardless of the underlying cause, correction of the malunited femur is very important to restore the normal mechanical and anatomical axis of the lower limb.
Ilizarov ring fixator has been widely accepted as a treatment of choice for gradual deformity correction [5]. However, in the case of complex multiplanar deformity correction, frequent adjustment and change of frame construct may be required, which is not just time-consuming but in certain circumstances, impossible [6,7]. This poses a significant challenge even to the most experienced surgeon [8,9]. This problem has been overcome following the introduction of a computer-assisted hexapod system, which allows deformity correction in 6 axes and in all planes simultaneously with the aid of computer software.
To the best of our knowledge, there were very few reports on the outcome of complex femoral deformity correction using the hexapod system. In 2007, Manner et al reported 58 cases of femoral deformity correction from his series containing 208 cases of gradual deformity correction of the lower limb using TSF [5]. He concluded that TSF has a clear advantage over the Ilizarov ring fixator in terms of deformity correction precision in 2-, 3- and 4-dimensional deformity correction.
Another report on femoral deformity correction using the hexapod system was published in 2014 by Solomon et al. He reported 47 cases of femoral deformity of various severity, who underwent gradual deformity correction using Ortho-SUV frame. He demonstrated that the Ortho-SUV frame improves the accuracy of correction and reduces correction time of deformity in the femur compared to conventional Ilizarov ring fixator in their study in 2014 [10]. There is a general consensus that hexapod systems like TSF and OrthoSUV frame are effective surgical tools in aiding to achieve complex skeletal deformity correction with high accuracy [5,8,10–12].
Pin site infection and morbidity is a common complication in the Ilizarov procedure with potential catastrophic complications when uncontrolled pin tract infection causes pin-bone interface loosening and hence threatening the stability of the construct. The reported incidence of pin site infection varies greatly, ranging from 11.3 % to 100 % [13–20]. We reported 5 cases of pin site morbidity in our series (38.5 %), with 1 case that led to osteomyelitis and 1 case of superficial abscess formation. None of the offending pin leads to construct destabilization in our series. A higher rate of pin site infection is not uncommon in Ilizarov to construct for the femur, due to the bulkier soft tissue window leading to more movement between the soft tissue-pin interface [21–23]. We advocate detailed preoperative planning so that intraoperatively a stable frame construction can be achieved, as an unstable construct can cause excessive movement of the pin-bone interface, leading to pin site irritation and infection [18,24]. The managing team should also have a detailed protocol to be adopted intraoperatively to ensure an atraumatic insertion of the pins and wires, to avoid unnecessary iatrogenic injuries to surrounding skin, soft tissue, and bone which can ultimately lead to a higher risk of infection.
Conclusion
In conclusion, various methods can be used for femoral deformity correction, depending on the degree of complexity, patient’s factor as well as surgeon’s expertise. In our study, a computer-assisted hexapod system such as the Ortho-SUV frame is a highly versatile clinical tool that if used correctly would yield high satisfactory clinical and radiological outcomes. We would recommend the use of the Ortho-SUV frame as a single-step correction technique for complex femoral deformity correction.
Conflict of interest: No conflict of interest to declare
References
- Sulaiman A, Eskandar H, Faisham W (2007) One-stage Versus Two-stage Reduction of Malunited Femoral Fracture with Shortening. Malays Orthop J. 1(1): 18–21.
- Tekin AÇ, Çabuk H, Dedeoğlu SS, Saygılı MS, Adaş M, et al. (2016) The results of bone deformity correction using a spider frame with web-based software for lower extremity long bone deformities. SICOT-J. 2: 11.
- Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, et al. (1989) Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop. (241): 146–65.
- Denisiuk M, Afsari A. Femoral Shaft Fractures. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Dec 17].
- Manner HM, Huebl M, Radler C, Ganger R, Petje G, et al. (2007) Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop. 1(1): 55–61.
- Sluga M, Pfeiffer M, Kotz R, Nehrer S (2003) Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop Part B. 12(2): 123–8.
- Fadel M, Hosny G (2005) The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 29(2): 125–9.
- Eidelman M, Bialik V, Katzman A (2006) Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 15(6): 387-95.
- Birch JG, Samchukov ML (2004) Use of the Ilizarov Method to Correct Lower Limb Deformities in Children and Adolescents. J Am Acad Orthop Surg. 12(3): 144-54.
- Solomin LN, Paley D, Shchepkina EА, Vilensky VA, Skomoroshko PV (2014) A comparative study of the correction of femoral deformity between the Ilizarov apparatus and Ortho- SUV frame. Int Orthop. 38(4): 865–72.
- Koren L, Keren Y, Eidelman M (2016) Multiplanar Deformities Correction Using Taylor Spatial Frame in Skeletally Immature Patients. Open Orthop J. 10(1): 71–79.
- Rozbruch SR, Pugsley JS, Fragomen AT, Ilizarov S (2008) Repair of Tibial Nonunions and Bone Defects with the Taylor Spatial Frame. J Orthop Trauma. 22(2): 88–95.
- Pizà G, Caja VL, González-Viejo MA, Navarro A (2004) Hydroxyapatite-coated external-fixation pins: the effect on pin loosening and pin-track infection in leg lengthening for short stature. J Bone Joint Surg Br. 86(6): 892-7.
- DeJong ES, DeBerardino TM, Brooks DE, Nelson BJ, Campbell AA, et al. Antimicrobial Efficacy of External Fixator Pins Coated with a Lipid Stabilized Hydroxyapatite/Chlorhexidine Complex to Prevent Pin Tract Infection in a Goat Model. J Trauma Inj Infect Crit Care. 50(6): 1008–14.
- Patterson MM (2005) Multicenter Pin Care Study: Orthop Nurs. 24(5): 349-360.
- Mostafavi HR, Tornetta P (1997) Open Fractures of the Humerus Treated With External Fixation. Clin Orthop. 337: 187–97.
- Cavusoglu AT, Er MS, Inal S, Ozsoy MH, Dincel VE, et al. (2009) Pin Site Care During Circular External Fixation Using Two Different Protocols. J Orthop Trauma. 23(10): 724–30.
- Parameswaran AD, Roberts CS, Seligson D, Voor M (2003) Pin Tract Infection With Contemporary External Fixation: How Much of a Problem?. J Orthop Trauma. 17(7): 503–7.
- Schalamon J, Petnehazy T, Ainoedhofer H, Zwick EB, Singer G, et al. (2007) Pin tract infection with external fixation of pediatric fractures. J Pediatr Surg. 42(9): 1584–7.
- Davies R, Holt N, Nayagam S (2005) The care of pin sites with external fixation. J Bone Joint Surg Br. 87(5): 716–9.
- Bibbo C, Brueggeman J (2010) Prevention and Management of Complications Arising from External Fixation Pin Sites. J Foot Ankle Surg. 49(1): 87–92.
- Santy J, Vincent M, Duffield B (2009) The principles of caring for patients with Ilizarov external fixation. Nurs Stand. 23(26): 50–5.
- Holmes SB, Brown SJ; Pin Site Care Expert Panel. (2005) Skeletal Pin Site Care: National Association of Orthopaedic Nurses Guidelines for Orthopaedic Nursing. Orthop Nurs. 24(2): 99-107.
- Yilmaz E, Belhan O, Karakurt L, Arslan N, Serin E (2003) Mechanical performance of hybrid Ilizarov external fixator in comparison with Ilizarov circular external fixator. Clin Biomech. 18(6): 518–22.