Alesci Rs1*, Hecking C1, Weißmann M2, Dempfle Ce2
1IMD Coagulation Centre Hochtaunus, Bad Homburg, Germany.
2IMD Coagulation Centre Hochtaunus, Mannheim, Germany.
*Corresponding Author: Alesci Rs, IMD Coagulation Centre Hochtaunus, Bad Homburg, Germany.
Abstract
Venous thromboembolism (VTE) is a common and severe blood clotting condition, and the incidence has been steadily increasing for years. Previous studies demonstrated that a VTE diagnosis is associated with emotional and mental harm, leading to anxiety and depressive disorders. Conversely, the risk of VTE development is known to be increased in patients with mental illnesses, which may lead to an increased risk of VTE recurrence.
In this prospective cohort study, 163 patients with confirmed VTE and 55 control subjects were surveyed about their mental status using validated questionnaires to assess the risk of developing anxiety and depression after a venous thromboembolic event. In general, VTE patients exhibited significantly increased Zung scores for concern (33.98 ± 9.93 vs. 28.53 ± 6.96, p<0.001) as well as for depression (38.22 ± 11.22 vs. 32.42 ± 7.6, p<0.001) compared to the control cohort. In addition, the evaluation revealed a higher risk of developing anxiety or depression in women than men. There was a trend towards a higher risk of mental health impairment after VTE with decreasing age, indicating an age-related effect. The association of anxiety with depression was confirmed and was not influenced by the occurrence of VTE events.
Our study provides additional evidence for an association between venous thromboembolic events and an increased risk of developing anxiety and depressive disorders, especially in female and young VTE patients. Therefore, more attention should be paid to mental health and quality of life in managing VTE treatment.
Keywords: Venous thromboembolism, anxiety, depression, quality of life
Introduction
Venous thromboembolism (VTE) is a common and severe blood clotting condition that includes both deep-vein thrombosis (DVT) and pulmonary embolism (PE).[1] The estimated incidence of VTE events in Germany of 0.14 is comparable to international rates.[2,3] The VTE incidence increases with age for men and women, whereby higher rates are reported in women during their childbearing years (age 16-44). Nevertheless, the overall age-adjusted annual incidence rate is higher for men than women. Since the year 2000, the annual incidence of venous thromboembolic events has increased and is the third most common cardiovascular cause of death. [2]
A few studies have shown that a VTE diagnosis is associated with emotional harm, mental fatigue, anxiety, and depression. Thus, 40.6% of patients with VTE are afraid of developing another clot.[4,5] However, little is known about the significance of the impact of VTE on patients' psyche. Some more data exists regarding quality of life. A recent Danish cohort study showed that the absolute risk of depression was 10.3% (95% CI, 10.1%-10.6%) in the VTE cohort and 5.6% (95% CI, 5.5%-5.6%) in the comparison cohort. VTE was associated with a 2.35-fold (95% CI, 2.28-2.43) increased risk of depression. The association was attenuated after adjustments for socioeconomic status and comorbidities (hazard ratio, 1.91; 95% CI, 1.85-1.97). [6]
Another prospective multicenter study group analyzed the quality of life for PE patients.
Even early discharge from hospitals in low-risk pulmonary embolism improves a patient's quality of life. [7] Conversely, the risk of venous thromboembolism increased in patients with concurrent depressive, bipolar, and schizophrenic disorders as well as in patients with psychotic disorders. [8,9] Thus, depression may be associated with an increased risk of VTE recurrence in the sense of a negative feedback loop.[9,10]
Despite the increasing number of VTE patients, increasing attention is paid to quality of life in the management of VTE treatment.[11,12] Comparing data of QoL prospective studies regarding anxiety and depression are conducted. To complement other recent German studies, [13,28] we aim to assess the risk of developing anxiety and depression disorders and a potential age-related and gender-related effect on this risk in VTE patients. In general, we intend to focus more on patients' mental health, which significantly impacts the quality of life of VTE patients.
Methods
The study was designed as a prospective, monocentric, questionnaire-based case-control study. Participants were recruited from May 2018 to August 2021. The study design was reviewed and approved by the Ethics Committee of the Medical Association of Hesse (Ref no FF104/20187) in November 2018 and is consistent with the ethical standards included in the Declaration of Helsinki of 1964 and its later amendments.
Patients and controls
Adult patients from the Coagulation Centre Hochtaunus, Germany, with confirmed diagnoses of thromboembolic events, including deep vein thrombosis and pulmonary embolism, were recruited consecutively. Patients with arterial thrombosis or atypical thrombosis were omitted. In addition, healthy accompanying adult persons (non-relatives) or relatives of patients, as well as adult staff and family members of the team without thromboembolic events, without known hereditary thrombophilia, and anticoagulation therapy, were used as the control group. Further, exclusion criteria were pregnancy, active cancer, known depression or anxiety, or other severe chronic diseases like rheumatoid arthritis. All participants were required to provide their written informed consent before enrolment. Much effort was made to match the cases and controls (Table 1).
Questionnaires
The primary objective was the assessment of anxiety and depression, which was carried out using two questionnaires, the Zung Self-Rating Anxiety Scale (SAS) [14]and the Zung Self-Rating Depression Scale (SDS). [15] All questionnaires were paper-based self-report / self- assessment forms mailed to the patients and the control cohort. The SAS and SDS by Zung are used to evaluate the level of anxiety and depression in patients. There are 20 items on each scale, which rate psychological and somatic symptoms associated with anxiety and depression. Each question is scored on a scale of 1-4, resulting in total raw scores from 20-80.[14,15] The clinical interpretation of the participants’ anxiety level is determined by the following cut-offs:
- 20-44 normal range,
- 45-59 mild to moderate anxiety level,
- 60-74 marked severe anxiety levels,
- 75-80 extreme anxiety level.[14]
The level of depression is determined by the following cut-offs:
- 20-49 normal range,
- 50-59 mildly depressed,
- 60-69 moderately depressed,
- 70-80 severely depressed.[15]
Another questionnaire was the PHQ-D (Patient Health Questionnaire- Depression). which was used as a self-administered screening tool to assess the severity of depressive symptoms. Unlike other depression scales, PHQ-9 includes 9 items, focusing on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) for MDD.
PHQ- showed good reliability and validity and high adaptability for patients with depression. It is a simple, rapid, effective, and reliable tool for screening and evaluating the severity of depression. He PHQ-9 The questionnaire assesses how often the subjects had been disturbed by any of the 9 items during the immediately preceding 2 weeks [29].
Secondary objectives were changes in quality of life, hospitalization for mental illness, and the need for antidepressant therapy.
Statistical analyses
Runge Statistik GmbH Hamburg, Germany, performed descriptive and interference statistical analyses of all collected data.
For the comparison of patients and control cohort regarding scores for anxiety as well as for depression, the t-test with Welch correction was applied. The comparison of age-related as well as gender-specific effects on the expression of anxiety and depression in patients and controls was tested by using the Median test. The assessment of the association of generalized anxiety with depression was done by regression analysis with resampling in the sense of bootstrapping. To find out if the association between stress and depression was influenced by thromboembolic events, a moderation analysis was performed. All tests were two-sided, and significance was declared at the 0.05 level. A statistical number of cases was planned.
Results
Baseline characteristics of patients and controls
This study enrolled 163 patients, with almost equal gender distribution (77 male, 86 female patients) and a median age of 59 years, ranging from 21 to 89 years, with a standard deviation of 14.59 years. Of the VTE patients, 115 were diagnosed with deep vein thrombosis (DVT) and 137 with pulmonary embolism (PE). Of the DVT patients, 35.1% experienced one recurrence, 4.4% twice, and 1.8% three times. Of the PE patients, 8.2% experienced one recurrence and 1.4% twice. All patients with PE received anticoagulant therapy. Noticeably, the medical history and comorbidities were evaluated for all patients, and the family history of 56% of patients was known, while both were not recorded for the control cohort (Table 1).
The control cohort included 55 persons with unequal gender distribution (18 male, 37 female) and a median age of 48 years, ranging from 19 to 68 years, with a standard deviation of 7.2 years. None of them received anticoagulant therapy.
Table 1: Baseline characteristics of VTE patients and control cohort.
|
Characteristics, n |
Patient cohort (n=163) |
Control cohort (n=55) |
|
Age, mean (Range) |
57.9 (21-89) |
46.2 (19-68) |
|
Gender, n Male Female |
77 86 |
18 37 |
|
Deep vein thrombosis, n Recurrences, n (%) 1 2 3 |
115 40 (35.1) 5 (4.4) 2 (1.8) |
- |
|
Pulmonary embolism, n Recurrences, n (%) 1 2 |
137 12 (8.2) 2 (1.4) |
- |
|
Anticoagulant therapy, n (%) |
137 (84.1) |
- |
|
Medical history known, n (%) |
163 (100) |
0 |
|
Family history known, n (%) |
91 (56) |
0 |
Higher scores for anxiety and depression in patients compared to controls.
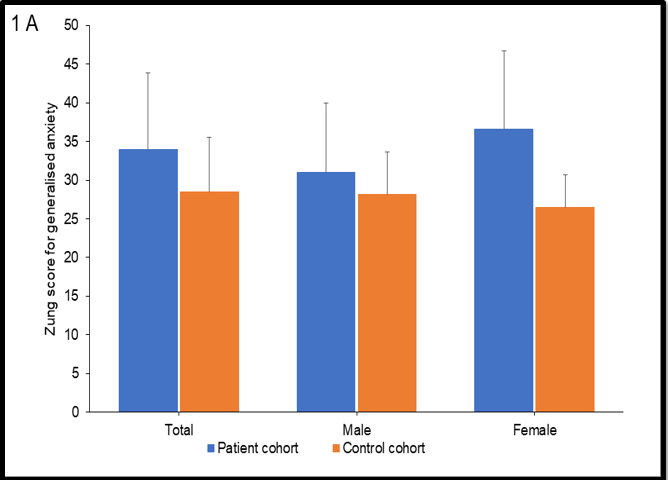
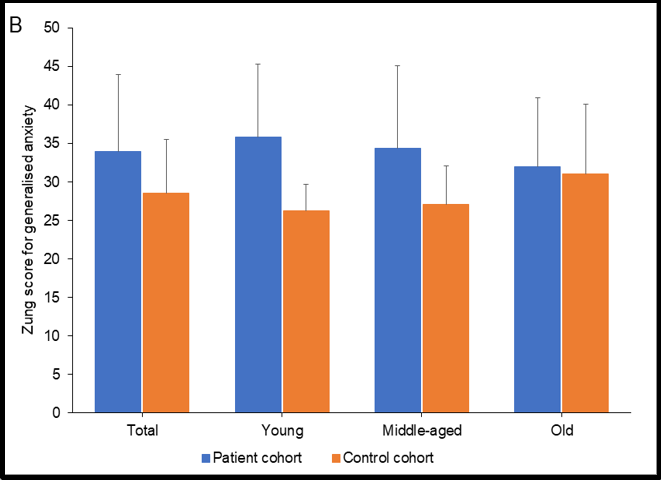
As depicted in (Figure. 1), the Zung scores for generalized anxiety were significantly higher in patients than control participants (33.98± 9.93 vs. 28.53 ± 6.96, p<0.001). A gender-related effect could be determined by measuring higher scores in female compared to male patients (36.62 ± 10.12 vs. 31.04 ± 8.88), while in controls no difference between females and males (26.43 ± 4.28 vs. 28.17 ± 5.49) could be observed. The significant increase in the anxiety score in patients is mainly driven by the more profound mean difference between the scores of patients vs. controls in women compared to men (mean difference: 10.18 vs. 2.87) (Figure. 1A). Additionally, age-related effects could be observed by measurement of higher scores for young and middle-aged patients compared to elderly patients (35.77± 9.53 vs. 34.35 ± 10.75 vs. 31.97 ± 8.98), with young patients having the highest anxiety scores. In controls, the older adults had the highest scores (31.00 ± 9.06; young: 26.27 ± 3.45; middle-aged: 27.12 ± 4.95). Consequently, the difference in the scores from the control to patient cohort turned out to be smaller in the elderly than in middle-aged and young subjects (mean difference: 0.97 vs. 7.23 vs. 9.5) (Figure. 1B). Of note, the age distribution differed remarkably between patient and control cohort. The classification into young, middle-aged, and old was based on the percentiles of the whole population to obtain equal-sized groups (young: ≤51 years, middle-aged: 52-63 years, old: ≥64 years). This resulted in a considerably different age distribution with 48 young, 49 middle-aged, and 65 geriatric patients, 26 young, 25 middle-aged and only 4 old control participants.
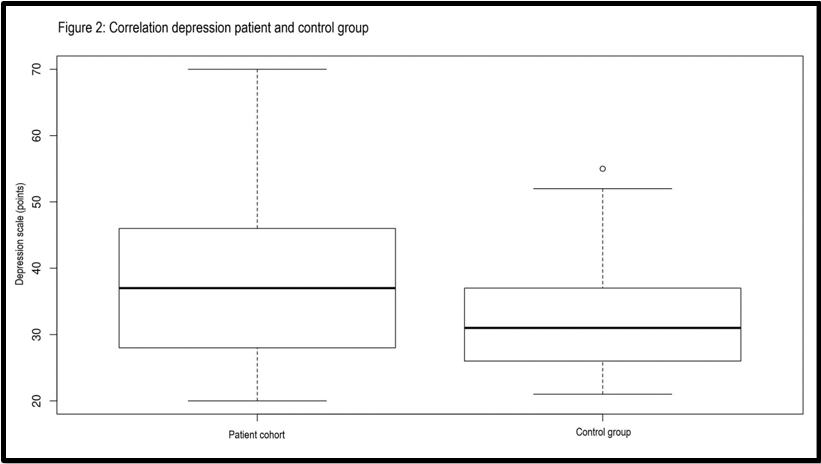
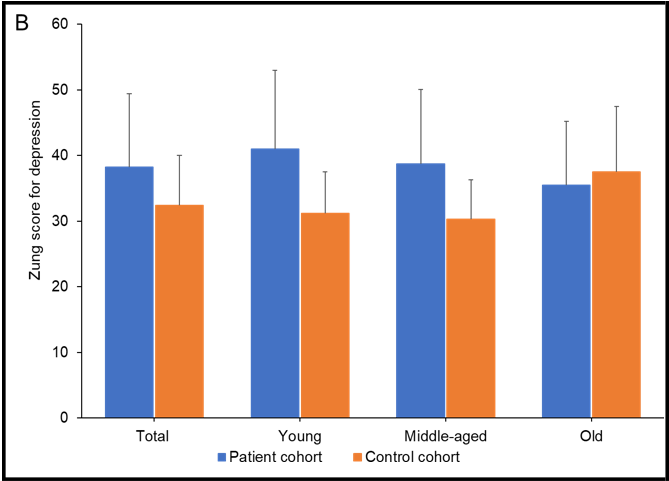
Similar to the results for generalized anxiety, the Zung depression scores were, in general, significantly higher in patients than in the control cohort (38.22 ± 11.22 vs. 32.42 ± 7.6, p<0.001) (Figure. 2). As well, a gender-related effect could be measured with higher scores in female patients compared to male patients (41.13 ± 12.11 vs. 34.97 ± 9.17). The control cohort showed no difference between females and males (30.67 ± 5.64 vs. 32,50 ± 8.15). Hence, the difference between the scores of patients and the scores of control participants was more profound in women than men (mean difference: 10.45 vs. 2.47) (Figure. 2A). An age-related effect on the development of depression after VTE could also be determined. The Zung depression scores were higher for young and middle-aged patients than elderly patients (40.96 ± 12.04 vs. 38.69 ± 11.34 vs. 35.52 ± 9.72), with young patients exhibiting the highest depression scores. Among the control cohort, the elderly participants had the highest depression scores, comparable to anxiety scores. Interestingly, the depression scores were slightly elevated in elderly control participants compared to elderly patients (37.50 ± 9.95 vs. 35.52 ± 9.72). Therefore, the difference between the scores from the control and the patient groups is smaller in the elderly than in middle-aged and young subjects (mean difference: -1,98 vs. 8.37 vs. 9.37) (Figure. 2B).
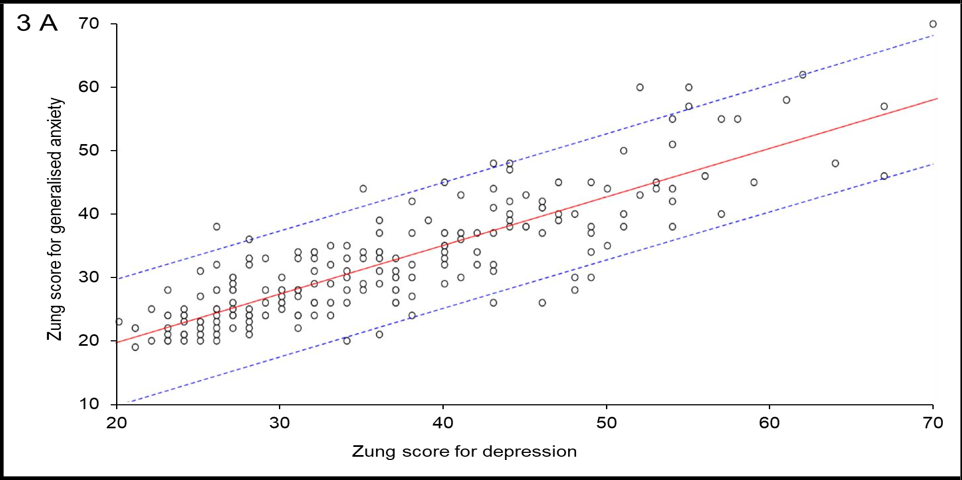
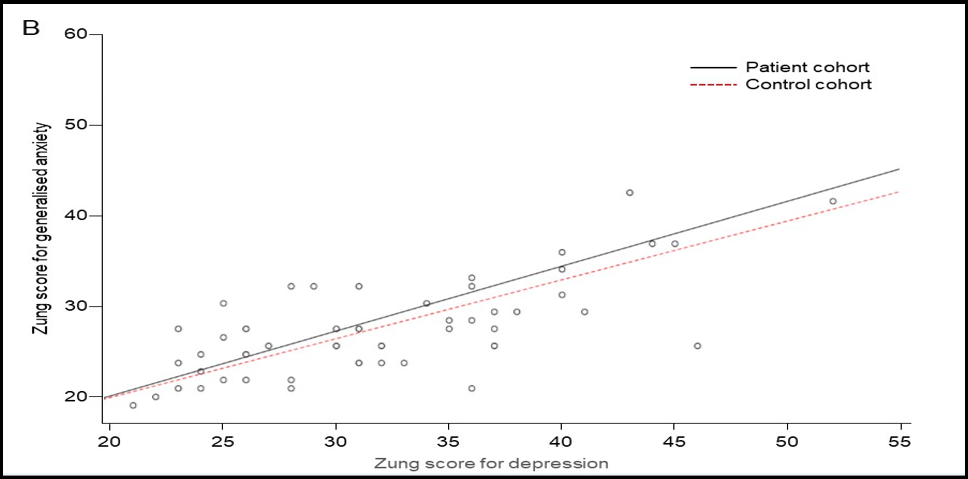
Further, we could show a significant (p < 0.001) correlation between the BDI and the Zung depression score (figure 3). In summary, this indicates that the results were similar even when using another questionnaire.
Figure 1: Anxiety in VTE patients vs. healthy controls. A) Zung scores for generalised anxiety in total patient cohort and comparison cohort in general and differentiated by gender. Blue bars: Mean of Zung scores in patient cohort; orange bars: Mean of Zung scores in control cohort; error bars mark standard deviation; P<0.001 for the interaction of the Zung scores between male patients and male controls, and female patients and female controls, respectively. B) Zung scores for generalised anxiety in total patient cohort and control cohort in general and differentiated by age. Blue bars: Mean of Zung scores in patient cohort; orange bars: Mean of Zung scores in control cohort; error bars mark standard deviation; P=0.002 for the interaction of the Zung scores between young patients and young controls, middle-aged patients and middle-aged controls, and old patients and old controls, respectively.
Figure 2: B Depression in VTE patients vs. healthy controls. A) Zung scores for depression in total patient cohort and comparison cohort in general and differentiated by gender. Blue bars: Mean of Zung scores in patient cohort; orange bars: Mean of Zung scores in control cohort; error bars mark standard deviation; P<0.001 for the interaction of the Zung scores between male patients and male controls, and female patients and female controls, respectively. B) Zung scores for depression in total patient cohort and control cohort in general and differentiated by age. Blue bars: Mean of Zung scores in patient cohort; orange bars: Mean of Zung scores in control cohort; error bars mark standard deviation; P=0.002 for the interaction of the Zung scores between young patients and young controls, middle-aged patients and middle-aged controls, and old patients and old controls, respectively.
Figure 3: Assessment of a potential influence of VTE occurrence on the association of anxiety with depression. A) Regression analysis to assess the association of anxiety with depression of the whole population (controls and patients) as the basis for the subsequent moderation analysis. B) Moderation analysis to assess an influence of VTE (black line: patient cohort vs. red dotted line: control cohort) on association of anxiety with depression.
Discussion
In line with comprehensive evidence from other studies, [4,13,16,17,28] this current study reveals an association between the development of generalized anxiety disorders and thromboembolic events and between depression and VTE events. The result of anxiety and depression was also seen in other rare bleeding disorders and thrombotic diseases, indicating a significant impact of general cardiovascular events on the patient's mental health and quality of life. [6,7,18] Of note, one of the study's limitations is that comorbidities were only evaluated in the patient but not the control cohort. This also includes conditions such as thyroid diseases, hypertension, heart failure, renal diseases, or gene mutation of blood coagulation factors, which can affect the cardiovascular system and thus impair the patient's quality of life. Finally, these aspects may also influence the Zung scores for anxiety and depression in the patient group of this study.
However, not only does venous thromboembolism increase the risk of impaired mental health, but conversely, anxiety and depression, as well as the use of antidepressants, are associated with an increased risk of developing VTE. [9,10,19] Hence, mental disorders developing after a thromboembolic event may enhance the risk of VTE recurrence. VTE treatment management should pay more attention to patients' quality of life and possible risk factors leading to VTE recurrence to prevent this downward cycle. The mechanisms by which mental disorders increase the risk for VTE occurrence or recurrence are still not fully understood. It is known that patients with depression have high rates of hyperhomocysteinemia, which have been suggested to be correlated with an increased risk of VTE. [20,21] In addition, depressed patients have been reported to exhibit greater platelet activation and increased procoagulant activity.[22] Based on a depression-like phenotype in mice with knock-in of a polymorphism of the BDNF gene, which also revealed a hypercoagulable state and platelet hyperreactivity, a genetic cause for this effect was assumed. [23] Further research is needed to potentially identify not only new risk factors but also biomarkers to achieve better prevention and treatment options for at-risk patients both with depressive disorders and VTE.
In this study, the scores for anxiety and depression were lower in elderly VTE patients compared to middle-aged and younger patients, while in controls, older adults had higher scores than middle-aged and young people. This effect could be due to some coping mechanisms based on life experience. Noticeably, this is a very speculative assumption, especially since another limitation of the study was the generally higher age of the patients compared to the control group. Nevertheless, it would still be an interesting future research objective, as most studies – which focused either on VTE risk due to depression or on increased risk of developing depression due to prior VTE – did not mention any age-related assessment, so such an effect has not been described so far. [4,9]
In the patient cohort, more women than men developed anxiety and depression compared to healthy controls with no sex-dependent difference. Slightly higher scores for anxiety and depression were also reported previously, [4] but to a lesser extent than observed in this study. In general, women had a significantly higher odds ratio of major depressive disorder (MDD) compared to men [24] and well, women are 1.5 to 2 times more likely to develop an anxiety disorder.[25] One reason for these observations could be that women are at higher risk of developing VTE especially during their potentially childbearing years (16-44 years). [2]In a Jordan study, more than 96% of pregnant women experiencing VTE reported anxiety and depression after the thrombotic event. [26]In terms of increased risk of VTE recurrence after development of a depressive or anxiety disorder, women represent a particularly vulnerable group to recurrent VTE. [8,9]
Anxiety and depressive disorders are highly comorbid, [25]confirmed by the regression analysis in this study, revealing a solid association of generalized anxiety with depression in all participants. As shown by moderation analyses, VTE events do not influence this association. This suggests that VTE events do not increase the risk of developing additional depression in anxious patients about potential thromboembolic recurrences and their impact on patients' mental health.
The study is limited by the small number of participants, the different age distribution between the patient and control cohorts, the lack of knowledge about the medical and family history of the control cohort, and the aspect of potential bias due to the subjective assessment of anxiety and depression. Nevertheless, the validated questionnaires by Zung can also be mentioned as one of the study's strengths. Furthermore, the comparison with a control cohort was feasible, and gender- and age-related effects could be investigated and identified, mainly since the latter has not been described yet.
In summary, experiencing thromboembolic events increases the risk of developing anxiety and depressive disorders, as shown by this and other studies.[4,5,13,17] Additionally, anxiety and depression are risk factors themselves for the development of VTE. [9,19,27] Therefore, the question arises if recurrence of thromboembolic events could be prevented if the treatment management would pay more attention to patient's mental health and quality of life.[10] Current management of care of VTE patients does not include the maintenance of impaired mental health or patients' quality of life in general, [11,12] but this study confirms previous suggestions that patients with VTE could benefit from interventions improving their quality of life.[16]
Conclusion
The results of this study support the association between VTE and depression and anxiety. We hope to highlight the importance of incorporating mental health into managing VTE patients and raise awareness of this critical correlation. Patients with anxiety and depression have a reduced quality of life- it should be our goal to improve their quality of life by offering therapeutical interventions.
Funding sources: There is no funding source to declare.
Acknowledgments
The statistical analysis was performed with the help of Runge Statistik GmbH, Hamburg, Germany. The preparation of the manuscript was supported by med: unit GmbH, Rheinbach, Germany.
Conflict of Interest: There is no conflict of interest to declare of each other.
Summary
Increasing evidence indicates an association between venous thromboembolism (VTE) and an increased risk of developing anxiety and depressive disorders. Our study aims to assess the risk of developing anxiety and depression disorders and a potential age-related as well as gender-related effect on this risk in VTE patients by surveying VTE patients and healthy control subjects using validated questionnaires (Zung Self-Rating Anxiety Scale and Zung Self-Rating Depression Scale). Significantly increased scores for anxiety and depression were revealed in patients compared to healthy controls. Evaluation of potential gender- and age-related effects demonstrated a higher risk of developing anxiety and depression after VTE in female and younger patients. We, therefore, suggest enhancing VTE treatment management by additionally focussing on patients' mental health to improve quality of life and minimize the risk of VTE recurrence.
References
- Reitsma PH, Versteeg HH, Middeldorp S (2012) Mechanistic view of risk factors for venous thromboembolism. Arterioscler Thromb Vasc Biol. 32(3): 563-8.
- Heit JA (2015) Epidemiology of venous thromboembolism. Nat Rev Cardiol. 12(8): 464-74.
- Keller K, Hobohm L, Ebner M, Kresoja KP, Münzel T, et al. (2020) Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur Heart J. 41(4): 522-529.
- Feehan M, Walsh M, Van Duker H, Godin J, Munger MA, et al. (2018) Prevalence and correlates of bleeding and emotional harms in a national US sample of patients with venous thromboembolism: A cross-sectional structural equation model. Thromb Res. 172: 181-187.
- Lukas PS, Krummenacher R, Biasiutti FD, Begré S, Znoj H, et al. (2009) Association of fatigue and psychological distress with quality of life in patients with a previous venous thromboembolic event. Thromb Haemost. 102(6): 1219-26.
- Jørgensen H, Horváth-Puhó E, Laugesen K, Brækkan SK, Hansen JB, et al. (2022) Venous thromboembolism and risk of depression: a population-based cohort study. J Thromb Haemost. 21(4): 953- 962.
- Barco S, Schmidtmann I, Ageno W, Anušić T, Bauersachs RM, et al. (2021) Survival and quality of life after early discharge in low-risk pulmonary embolism. Eur Respir J. 57(2): 2002368.
- Kowal C, Peyre H, Amad A, Pelissolo A, Leboyer M, et al. (2020) Psychotic, Mood, and Anxiety Disorders and Venous Thromboembolism: A Systematic Review and Meta-Analysis. Psychosom Med. 82(9): 838-849.
- Lin CE, Chung CH, Chen LF, Chien WC (2019) Increased risk for venous thromboembolism among patients with concurrent depressive, bipolar, and schizophrenic disorders. Gen Hosp Psychiatry. 61: 34-40.
- von Känel R, Margani A, Stauber S, Meyer FA, Demarmels Biasiutti F, et al. (2015) Depressive symptoms as a novel risk factor for recurrent venous thromboembolism: a longitudinal observational study in patients referred for thrombophilia investigation. PLoS One. 10(5): e0125858.
- Piazza G (2020) Advanced Management of Intermediate- and High-Risk Pulmonary Embolism: JACC Focus Seminar. J Am Coll Cardiol. 76(18): 2117-2127.
- Renner E, Barnes GD (2020) Antithrombotic Management of Venous Thromboembolism: JACC Focus Seminar. J Am Coll Cardiol. 76(18): 2142-2154.
- Kämpf S, Weißbach L, Zotz R (2022) Epidemiological study about the mental state of patients after a pulmonary embolism or deep venous thrombosis event. Blood Coagul Fibrinolysis. 33(5): 257-260.
- Zung WW (1971) A rating instrument for anxiety disorders. Psychosomatics. 12(6): 371-9.
- Zung WW (1965) A Self-Rating Depression Scale. Arch Gen Psychiatry. 12: 63-70.
- Erickson RM, Feehan M, Munger MA, Tak C, Witt DM (2019) Understanding Factors Associated with Quality of Life in Patients with Venous Thromboembolism. Thromb Haemost. 119(11): 1869-1876.
- Hunter R, Lewis S, Noble S, Rance J, Bennett PD (2017) "Post- thrombotic panic syndrome": A thematic analysis of the experience of venous thromboembolism. Br J Health Psychol. 22(1): 8-25.
- Alesci SR, Schwan V, Miesbach W, Seifried E, Klinger D (2013) Rare bleeding disorders are associated with depression and anxiety. Hamostaseologie. 33 Suppl 1: S64-8.
- Kunutsor SK, Seidu S, Khunti K (2018) Depression, antidepressant use, and risk of venous thromboembolism: systematic review and meta-analysis of published observational evidence. Ann Med. 50(6): 529-537.
- Penninx BW, Guralnik JM, Ferrucci L, Fried LP, Allen RH, et al. (2000) Vitamin B(12) deficiency and depression in physically disabled older women: epidemiologic evidence from the Women's Health and Aging Study. Am J Psychiatry. 157(5): 715-21.
- Ray JG (1998) Meta-analysis of hyperhomocysteinemia as a risk factor for venous thromboembolic disease. Arch Intern Med. 158(19): 2101-6.
- Musselman DL, Tomer A, Manatunga AK, Knight BT, Porter MR, et al. (1996) Exaggerated platelet reactivity in major depression. Am J Psychiatry. 153(10): 1313-7.
- Amadio P, Colombo GI, Tarantino E, Gianellini S, Ieraci A, et al. (2017) BDNFVal66met polymorphism: a potential bridge between depression and thrombosis. Eur Heart J. 38(18): 1426- 1435.
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, et al. (2003) The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 289(23): 3095-105.
- Thibaut F (20017) Anxiety disorders: a review of current literature. Dialogues Clin Neurosci. 19(2): 87-88.
- Al-Husban N, Alnsour LN, El-Adwan Z, Saleh NA, El-Zibdeh M (2021) Impact of Pregnancy-Related Venous Thromboembolism on Quality of Patients' Lives. Clin Appl Thromb Hemost. 27: 10760296211040873.
- Lee CW, Liao CH, Lin CL, Liang JA, Sung FC, et al. (2015) Depression and risk of venous thromboembolism: a population- based retrospective cohort study. Psychosom Med. 77(5): 591-8.
- Valerio L, Barco S, Jankowski M, Rosenkranz S, Lankeit M, et al. (2021) Quality of Life 3 and 12 Months Following Acute Pulmonary Embolism: Analysis From a Prospective Multicenter Cohort Study. Chest. 159(6): 2428-2438.
- Sun Y, Fu Z, Bo Q, Mao Z, Ma X, et al. (2020) The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 20(1): 474.