Devraj Kandel 1*, Prakash Dhakal 1, Siddhartha Bhandari 3, Sandeep Mahat 1, Jagat Baniya 2
1Department of Radiodiagnosis and Imaging, National Academy of Medical Sciences, Mahabouddha, Kathmandu, Nepal.
2National Public Health Laboratory, Teku, Kathmandu, Nepal.
3St Vincent Hospital, Worcester, MA
*Corresponding Author: Devraj Kandel, Department of Radiodiagnosis and Imaging, National Academy of Medical Sciences, Mahabouddha, Kathmandu, Nepal.
Abstract
Introduction: Rasmussen Encephalitis is a rare, chronic inflammatory condition of the brain mostly affecting children and involving one cerebral hemisphere. The most common presentation is a chronic intractable seizure with the diagnosis being made on MRI as a part of a comprehensive neurological or seizure work-up.
Case summary: An 18-year-old male on anti-epileptics for 5 years developed increased episodes of seizure even with regular intake of anti-epileptics for the last three monts.
Imaging findings: CT and MRI of the brain show an atrophied left cerebral hemisphere including head of left caudate nucleus with dilatation of ipsilateral lateral ventricle.
Differential diagnosis: For the given imaging characteristics, the common differentials are; Dyke Davidoff Masson syndrome (DDMS), Sturge- Weber syndrome and Hemi-megalencephaly.
Discussion: First diagnosed in 1958, Rasmussen encephalitis is yet to find the complete curative treatment. Development of advanced imaging modalities have facilitated the diagnosis. Surgical excision is the modality with promising results however in expense of permanent hemiparesis after hemispherectomy.
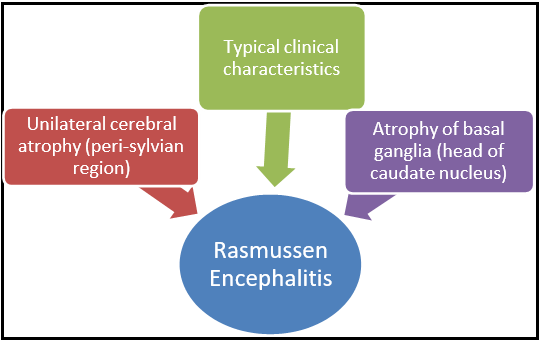
Conclusion: In a patient presenting with typical clinical history and imaging findings of unilateral cerebral atrophy (peri-sylvian region) and atrophy of basal ganglia (head of caudate nucleus), Rasmussen encephalitis should be considered.
Keywords: Rasmussen Encephalitis, Hemiatrophy, Atrophy of head of caudate nucleus, Intractable Seizure, Cortical Atrophy
Graphical Abstract
Introduction:
Rasmussen Encephalitis is a rare, chronic inflammatory condition of the brain mostly affecting children and involving one cerebral hemisphere.[1] It is most common in children below 10 years of age with rare instances seen in adolescents and young adults. The most common presentation is a chronic intractable seizure with the diagnosis being made on MRI as a part of a comprehensive neurological or seizure work-up. Some cases may present with hemiparesis, neurological deterioration, or loss of speech or motor skills.[2] We present an 18-year-old male, who presented to the department of neurosurgery, Bir Hospital with a progressive seizure disorder.
Clinical history:
The patient had initially developed seizures 5 years back and had been on anti-epileptics. For the last 3 months, the frequency of seizures had increased with one to three episodes daily even with regular intake of anti-epileptics for which the patient was brought our to hospital.
The patient's family also complained of progressive right-sided hemiparesis in the child and deterioration in his cognitive functions. Past history of high grade fever with hospitalization for 14 days at the age of 9 months is present.
Imaging findings:
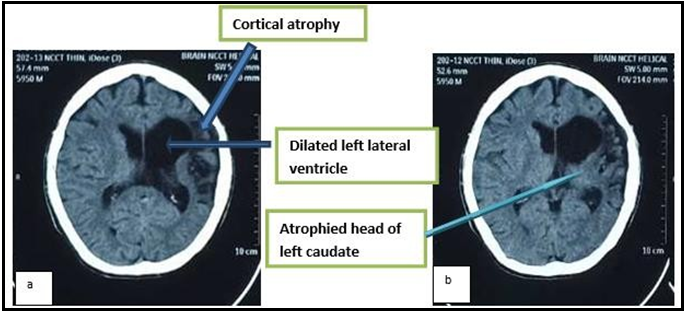
Non contrast CT Brain shows decreased volume of left cerebral hemisphere with atrophy of left fronto-parietal lobe and left basal ganglia predominantly involving the head of caudate nucleus.
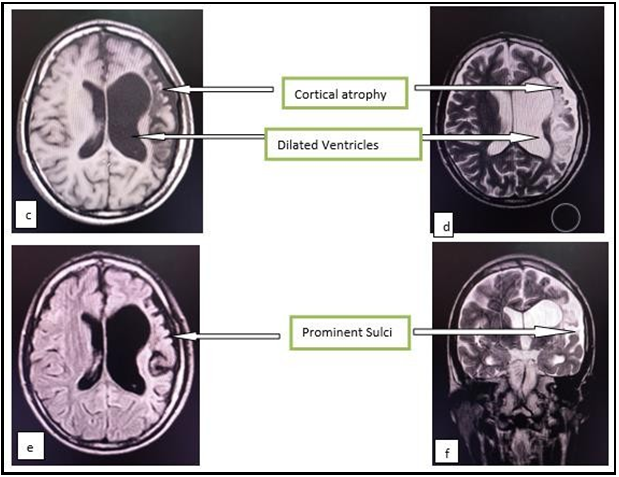
MRI also shows similar findings of decreased left cerebral hemisphere volume with areas of T1 hypointensity, T2 hyperintensity which are not suppressed on FLAIR sequences representing atrophied area of brain parenchyma including left basal ganglia. Adjacent T2/FLAIR high signal intensity area representing the gliotic changes are also noted.
Note is made of prominent sulci in the region of atrophied cortex with prominent adjacent subarachnoid space in both CT and MRI images. Dilatation of ipsilateral lateral ventricle is also noted in both CT and MRI images. Adjacent bony calvarium however appears normal.
These imaging findings support the diagnosis of Rasmussen Encephalitis.
Figure ‘a’ and ‘b’ are non-contrast CT head axial images showing an atrophied left cerebral hemisphere including head of left caudate nucleus with dilatation of ipsilateral lateral ventricle.
Figure ‘c’, ‘d’ and ‘e’ are T1, T2, and FLAIR axial images while figure ‘f’ is T2 coronal MRI brain image showing atrophied left cerebral hemisphere including left basal ganglia with dilatation of the ipsilateral lateral ventricle and adjacent gliotic changes.
Differential diagnosis:
For the given imaging characteristics, the common differentials are;
- Dyke Davidoff Masson syndrome (DDMS): unilateral cerebral atrophy is accompanied with ipsilateral calvarial enlargement and sinus hyperpneumatization.[3]
- Sturge-Weber syndrome: cerebral atrophy with tram track gyral calcification, enhancing angiomas and ipsilateral enlarged choroid plexus. [3]
- Hemimegalencephaly: a large unihemisphere with ipsilateral ventriculomegaly with areas of polymicrogyria, pachygyria and heterotopia. [3]
The above differential diagnoses were ruled out in our patient based on clinical findings together with CT and MRI findings
Discussion
First diagnosed in 1958, Rasmussen encephalitis is yet to find the complete curative treatment. In this era of high resolution CT and MRI, number of cases being diagnosed have increased. The imaging findings depend on the stage of the disease that are- prodromal, active, and chronic stages.4,5 Initially, there may be unilateral localized cortical edema. T2/FLAIR hyperintensity develops over time in the affected side's cortex and subcortical white matter. Unilateral cerebral and basal ganglia atrophy is evident as the disease progresses into the chronic phase. [4,5] Predilection for peri-sylvian cortex is seen. In our case, there is involvement of peri-sylvian cortex with atrophic brain changes suggesting the late stage of the disease. In cases with uncontrolled seizures, surgical excision of the involved half of cerebral hemisphere has been seen promising in terms of controlling the seizures and halting further deterioration of cognitive functions[6,7]. However, permanent hemiparesis is inevitable and the beforehand documentation of hemiparesis is advised. In our case however, patient refused to undergo surgery with high risk consent and chose to stay on anti-epileptics as for now.
Conclusion:
In a patient presenting with typical clinical history and imaging findings of unilateral cerebral atrophy (peri-sylvian region) and atrophy of basal ganglia (head of caudate nucleus), Rasmussen encephalitis is very likely.
Disclosure
Financial support: Nil
Conflict of interest: None declared
Acknowledgments: Vote of thanks to Prof. Dr Hensan Khadka, Dr. Nirmal Neupane and my dear wife Dr. Shishan Dhakal.
Patient consent: Informed written consent has been taken from the parent of the child by me, the principal author and can be reproduced as and when required.
References
- Geller E, Faerber EN, Legido A, Melvin JJ, Hunter JV, et al. (1998) Rasmussen encephalitis: complementary role of multitechnique neuroimaging. AJNR Am J Neuroradiol. 19(3): 445–9.
- Saeed Ahmed SK. Rasmussen’s Encephalitis: A Case Report. Journal of Neurological Disorders. 2013;02(01).
- Varghese B, Aneesh M, Singh N, Gilwaz P (2014) A Case of Rasmussen Encephalitis: The Differential Diagnoses and Role of Diagnostic Imaging. Oman Medical Journal. 29(1): 67–70.
- Bien CG, Widman G, Urbach H, Sassen R, Kuczaty S, et al. (2002) The natural history of Rasmussen’s encephalitis. Brain. 125(pt 8): 1751–9.
- Varadkar S, Bien CG, Kruse CA, Jensen FE, Bauer J, et al. (2014) Rasmussen’s encephalitis: clinical features, pathobiology, and treatment advances. The Lancet Neurology. 13(2): 195–205.
- Sarkar C, Deb P, Sharma M, Gaikwad S, Tripathi M, et al. (2005) Neuropathological spectrum of Rasmussen encephalitis. Neurol India. 53(2): 156-60 ; discussion 160-1.
- Hart YM, Andermann F, Robitaille Y, Laxer KD, Rasmussen T, et al. (1998) Double pathology in Rasmussen’s syndrome: A window on the etiology? Neurology. 50(3): 731–5.