Daud Fadi Jean1*, Nouini Adrâa2*
1Emergency department, Delta Hospital- Chirec, Brussels, Belgium
2Neurology department, Delta Hospital- Chirec, Brussels, Belgium, adraa.nouini@gmail.com
*Both authors are first authors
Introduction
Background
Nitrous oxide poisoning has been more and more common for several years. This hilarant gas is nowdays mostly consumed by young adults and teenagers for recreational purposes. It also used in the healthcare institutions for its analgesic, sedative and anesthetic proprieties.
We will report the case of a young eighteen-year-old patient who presented to the emergency department (ED) with multiple neurological and psychiatric symptoms, with cerebral white matter lesions that is not frequently reported in the medical literature.
Case Report
An eighteen-year-old patient presented to the ED on 13/12/2022, accompanied by her family members. She does not have any medical history. She does not take any medication and has no allergies. Since a night out with her friend two days before the presentation, she reports excessive sleeping, anorexia, positional orthostatic vertigo, and balance impairment. She also reports bilateral upper limbs paresthesia without weakness or walking difficulties. She also has intermittent blurry vision and memory impairment for one week.
The patient’s mother describes episodes in which her daughter loses contact and “keep staring”, without conscience loss. One day before the presentation, the mother found the patient unconscious in the bathroom. The patient reports no fever, chills, weight loss or night sweating. She does not have any cardio-pulmonary, digestive, or urinary symptoms.
She smokes 10 cigarettes a day since 6 years. She consumes excessive amounts of alcohol occasionally (binge drinking). She also reports nitrous oxide consumption since two years, around hundred inhalations per day on average.
The patient’s mother describes scholar difficulties and social isolation during the past year. She frequently has a depressive humor and compulsive behaviors like excessive shopping and binge eating.
On clinical examination, vital signs were normal.
Heart sounds are normal, regular without murmur. The lung sounds were normal. Her peristalsis was present and abdomen soft without hepatosplenomegaly.
On the neurological examination, she was bradypsychic but oriented towards person, place and time. She had a normal pupillary light reflex and normal cranial nerfs test. The meningeal signs were negative.
She had a normal motor exam with 5/5 strength on four limbs. Sensory examination for light touch, pain and vibration were normal. Ankle tendons reflexes were absent on both sides, the other tendon reflexes were normal and symmetric. She had no ataxia and the finger to nose test was normal. The Romberg sign was present. Babinski sign was absent.
Based on the patient’s anamnesis and clinical examination, the diagnosis of nitrous oxide poisoning and vitamin B12 deficiency was made.
Blood test showed vitamin B12 deficiency (< 150ng/L) and hyperhomocysteinemia. The cerebral scanner was normal.
On the next day, the patient went to the neurology department and an electro-encephalography showed epileptic encephalopathy.
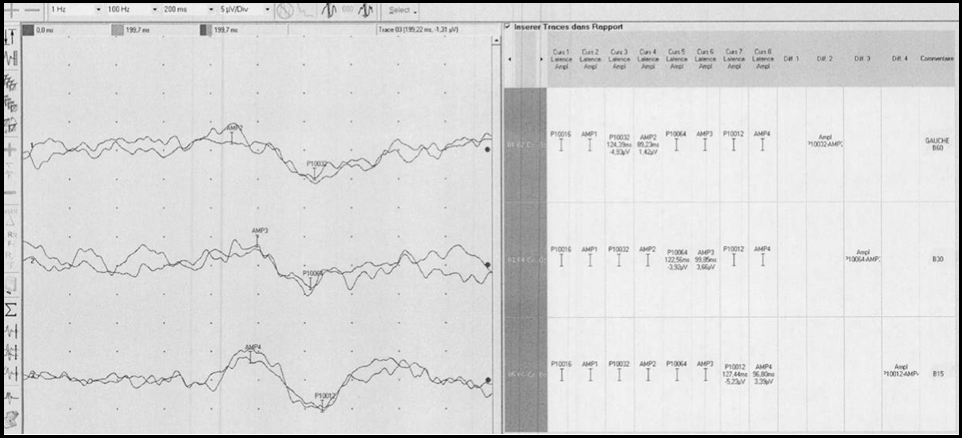
Visual evoked response test shows prolonged P100 latency > 118 ms on both eyes that was more severe on the left eye that indicates optic neuropathy (Figure 1)
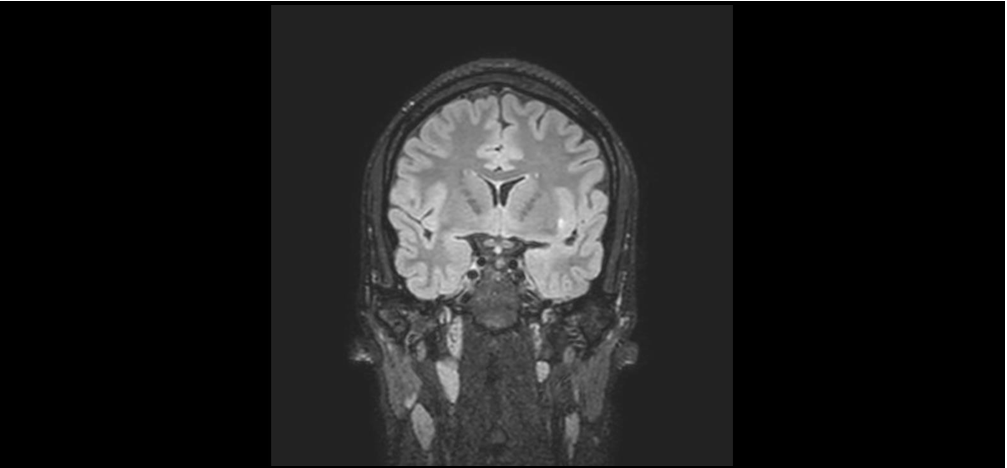
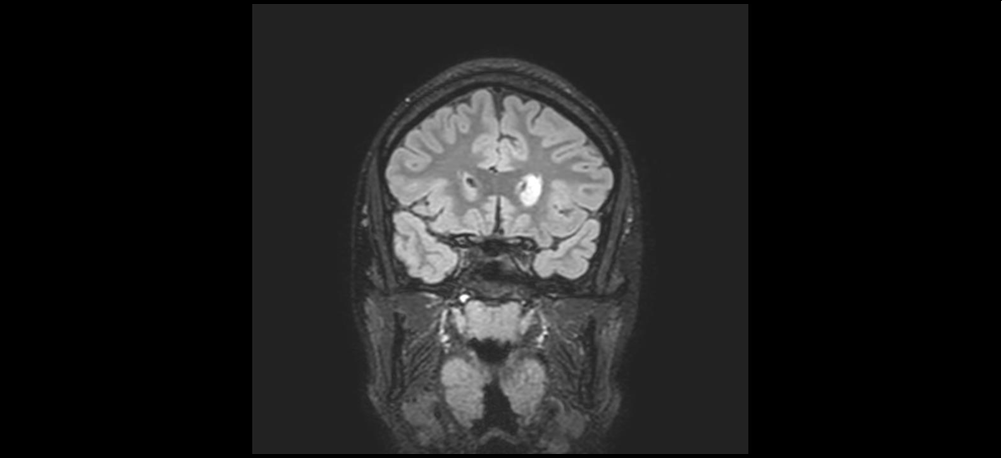
Electormyography was normal and with no evidence of polyneuropathy. Brain MRI three month later showed two white matter lesions, the first one involving the left frontal periventricular white matter and the second one involving the external left capsule (Figure 2).
Figure 1:
A. Visual evoked response : left eye.
B. Visual evoked response : right eye
Figure 2:
A: T1 Brain MRI showing left external capsular white matter lesion.
B: T1 Brain MRI showing left frontal periventricular white matter lesion
The spinal cord MRI showed no evidence of myelopathy.
We started treatment with vitamin B12 replacement and levetiracetam. After one month of treatment, the vertigo disappeared and the patient reported a significant improvement with her memory loss, she had no more visual symptoms. Her neurological exam showed normal ankle reflexes and Romberg sign was absent.
Her control EEG showed resolution of the epileptic activity and we stopped the levetiracetam.
Discussion
Nitrous oxide had been used in the medical field since the nineteen century and since 1956 there has been more and more evidence to its toxic effect, that are most commonly neurologic, psychiatric, cardiac and hematologic [1]. It also used in the food industry to fabricate whipped cream, which makes it accessible to the general population and can be purchased for recreational use due to its euphoric and dissociative effects. Individuals can inhale nitrous oxide through balloons or canisters [1].
The most frequent complications of nitrous oxide toxicity are neurological disorders. Several theories has been proposed to explain this effect, mostly the inactivation of vitamin B12 from its +1 state to +3. As a result, the inactivated vitamin B12 cannot fulfill its role as a cofactor of multiple chemical reactions:
1. The generation of methionine from homocysteine via the methionine synthase enzyme, which is cobalamin dependent. The inactivation of this reaction results in the accumulation of homocysteine [7].
2. Alteration in the conversion of 5-methytetrahydrofolate to tetrahydrofolate is important for DNA synthesis.
3. Inhibition of the conversion of metylmalonic acid to succenyl-coA via the methylmalonyl-CoA mutase enzyme that is also cobalamin dependent. This results in the accumulation of methylmalonic acid [22].
The clinical presentation of patients with nitrous oxide toxicity is variable. The clinician distinguishes the symptoms of acute intoxication from chronic intoxication.
During the acute intoxication, nitrous oxide passes more rapidly than oxygen through the alveoli basal membrane, which results in a transient hypoxia that is generally well supported in good health individuals but can cause mental status alteration as bradypschia , vertigo and seizures like the case of our patient, or could event result in cardiopulmonary complications and cardiac arrest specially in patient with cardiovascular co morbidities [10].
Our patient had probably presented clinical seizures when she was found in the bathroom. This hypothesis is reinforced by the next day EEG that showed spike waves. A recent study by Gao and Al has shown that the prevalence of seizures during nitrous oxide intoxication is 5% [5]
Chronic intoxication has a different presentation: patients will mostly report paresthesia, weaknesses, ataxia, difficulty walking and memory loss. Usually, symptoms start with ascendant paresthesia that progress to ataxia and walking difficulties [3]. Less frequently, patients may report urinary or fecal incontinence, sexual dysfunction, or mental status alteration.
Teenagers might present with less specific symptoms like abdominal pain, constipation or involuntary movements and it is important to consider nitrous oxide intoxication in these patients when they present to the ED. [3]
Psychiatric symptoms include psychoses, behavioral and humor disorders. It is important to mention that psychiatric symptoms might be the only presentation symptoms and it is important for the clinician to still consider N2O intoxication in these patients. Nitrous oxide had been added to the 5th DSM edition [22]. Our patient had several psychiatric symptoms which are probably related to megalobastic mania due to vitamin B12 deficiency and includes depression, mania, irritability, paranoia, delusion and lability. This clinical presentation was also described by Stabler and Al [15]
Other than the neurological and psychiatric presentations, some patients might have nonspecific cardio-respiratory symptoms like dyspnea and chest pain.
Neurological complications include transverse myelitis and peripheral neuropathy that can be axonal ou demyelination neuropathy. Our patient, who had vitamin B12 deficiency, probably had demyelination myelopathy of the posterior and lateral corns of the spinal cords. She had paresthesia, balance difficulties, positive Romberg sign but no pyramidal syndrome as described in the study conducted by Stabler and Al [15]. The absence of myelopathy on the spinal cord MRI can be explained by the fact that it was done 3 months after the correction of the vitamin B12 deficiency. She also had a deficiency optic neuropathy. The vitamin B12 deficiency can also cause cerebral white matter demyelination seen also in our patient (figure 2). In the study made by Bao and Al, 4 patients out of 33 (12%) had white matter demyelination in the bilateral frontal, periventricular, and centrum semi vale regions on brain MRI [10]. In a recent study by Gao and Al that included 13 patients, 15% had such lesions. Our patients control brain MRI after 7 months showed no change in these lesions [5].
Other than the neurological complications, recent studies showed that nitrous oxide intoxication can cause severe thromboembolic complications such pulmonary embolism, deep venous thrombosis, acute coronary artery syndrome and cerebral vascular accident [12] which could be related to the hyperhomocysteneimia and its prothrombotic effect. [13]
The diagnosis of nitrous oxide intoxication can be challenging and is done mainly through anamnesis. The blood test isn’t specific. N2O has a very short half-life and is rapidly eliminated by the lungs.
Vitamin B12 dosage and mean corpuscular volume are not sensitive enough to make the diagnosis and there is a bad correlation between the vitamin B12 blood value and its tissue stock value (which reflects more the tissue toxicity and clinical presentation). This means that blood vitamin B12 blood value can be still normal while nitrous oxide intoxication and B12 deficiency are already present. [14]
Several studies showed that homocysteine and methylmalonic acid blood values are more sensitive than the vitamin B12 value for the diagnosis of nitrous oxide intoxication and homocysteine was elevated in about 90% of cases in some studies [17,8,23,13]
Brain MRI can show toxic leuco-encephalopathy like we have seen with our patient, that’s why we recommend including brain MRI in the diagnostic approach.
Electromyography is also important to look for peripheral neuropathy. A study conducted by Zheng and Al showed that peripheral neuropathy is the second most frequent complication of nitrous oxide intoxication after myelopathy [23].
Prognosis after nitrous oxide intoxication is still limited, complete remission is possible, but persistence of sensitive and walking difficulties is common [8]. Our patient had a complete remission of her neurological symptoms.
The remission rate of neurological complications varies from different studies. Vascoles and Al had a remission rate of 14% [18] while a study made by Lan and Al showed 46 % although this study included mostly teenagers and only 9 patients in total [9].
The duration and severity of neurological symptoms before the diagnosis seem to be a factor influencing the rapidity of symptoms resolution after treatment initiation [11] and complete resolution of symptoms is higher in patients without spinal cord atrophy and with negative Babinski and Romberg signs upon presentation [18].
Other factors that favorably influence symptoms resolution are young age and the absence of anemia [18]. The most frequent sequelae seems to be sensitive anomalies and fatigue [1,8].
In what concerns the mortality rate, evidence is limited. Statistical review between 1985-2015 found 52 mortality cases mostly by asphyxia [4]
The treatment of nitrous oxide intoxication consists mainly of the complete abstinence of N2O usage and vitamin B12 deficiency correction. Studies had shown no difference between the high dose oral and the classic intramuscular administrations [2,15,21]. It is important to mention that recent studies are showing that N2O might have a neurological toxicity per se, mainly motor neuropathy that is different than the classic demyelination sensitive neuropathy seen with vitamin B12 deficiency. A case report published by Ji R and AL describes good response to methylprednisolone therapy in a patient who didn’t respond to B12 replacement which could indicate that corticoids might be a treatment option in such patients, further studies need to be done. [7]
Conclusion
Recreational use of nitrous oxide is more and more common since recent years mainly among teenagers and young adults. It is important to consider nitrous oxide intoxication in young patients presenting in the ED department with paresthesia and difficulty walking. Nitrous oxide toxicity is mainly due to vitamin B12 deficiency and complications are mainly neurologic, psychiatric and thromboembolic. We recommend adding brain MRI imaging for search for cerebral white matter lesions and EEG in patients with altered mental status. The treatment consists mostly in the complete abstinence of N2O usage and vitamin B12 replacement. Other therapy options are being studied.
References
- Garakani A, Jaffe RJ, Savla D, Welch AK, Protin CA, et al. (2016) Neurologic, Psychiatric, and Other Medical Manifestations of Ni-trous Oxide Abuse: A Systematic Review of the Case Literatur, Am J Addict. 25(5): 358-369.
- Andrès E, Fothergill H, Mecili M (2010) Efcacy of oral cobalamin (vitamin B12) therapy. Expert Opin Pharmacother. 11(2): 249–256.
- Burvill PW, Jackson JM, Smith WG (1969) Psychiatric symptoms due to vitamin B12 deficiency without anaemia. Med J Aust. 2(8): 388–390.
- Cockery J, Schifano F (2015) Volatile Substance Abuse Mortality Project.
- Gao H, Wang R, Zeng Y, Qin L, Cai H, et al. (2023) Nitrous oxide- induced neurotoxicity: Clinical characteristics and impacts on over- all neurological impairments. 14: 1132542.
- Hathout L, El-Saden S (2011) Nitrous oxide-induced B-12 defi- ciency myelopathy: Perspectives on the clinical biochemistry of vit- amin B12. J Neurol Sci. 301(1-2): 1–8.
- Ji R, Xie Z, Wang K, Zheng X (2018) Glucocorticoid treatment of myeloneuropathy induced by nitrous oxide toxicity. Neurol India. 66(4): 1167–1169.
- Keddie S, Adams A, Kelso ARC, Turner B, Schmierer K, et al. (2018) No laughing matter: subacute degeneration of the spinal cord due to nitrous oxide inhalation. J Neurol. 265(5): 1089-1095.
- Lan SY, Kuo CY, Chou CC, Kong SS, Hung PC, et al. (2019) Rec- reational nitrous oxide abuse related subacute combined degenera- tion of the spinal cord in adolescents - A case series and literature review. Brain Dev. 41(5): 428–435.
- Bao L, Li Q, Li Q, Chen H, Zhang R, et al. (2020) Clinical, Elec- trophysiological and Radiological Features of Nitrous Oxide- Induced. Neurological Disorders. 16: 977-984.
- Lin RJ, Chen HF, Chang YC, Su JJ (2011) Subacute combined de- generation caused by nitrous oxide intoxication: case reports. Acta Neurol Taiwan. 20(2): 129–137.
- Caris MG, Kuipers RS, Kiestra BE, Ruijter BJ, Riezebos RK, et al. (2023) Nitroux oxide abuse leading to extreme homocysteine levels and extreme venous thrombosis in young adults: a case series. 21(2): 276-283.
- Oussalah A, Julien M, Levy J, Hajjar O, Franczak C, et al. (2019) Global burden related to nitrous oxide exposure in medical and rec-reational settings: a systematic review and individual patient data meta-analysis. J Clin Med. 8(4): 551.
- Sanders RD, Weimann J, Maze M (2008) Biologic effects of nitrous oxide: a mechanistic and toxicologic review. Anesthesiology. 109(4): 707–722.
- Stabler SP (2013) Clinical practice. Vitamin B12 defciency. N Engl J Med. 368(2): 149–160.
- Tani J, Weng HY, Chen HJ, Chang TS, Sung JY, et al. (2019) Elu- cidating unique axonal. dysfunction between nitrous oxide abuse and vitamin B12 deficiency. Front Neurol. 10: 704.
- Thompson AG, Leite MI, Lunn MP, Bennett DL (2015) Whippits, nitrous oxide and the dangers of legal highs. Pract Neurol. 15(3): 207–209.
- Vasconcelos OM, Poehm EH, McCarter RJ, Campbell WW, Que- zado ZM (2006) Potential outcome factors in subacute combined degeneration: review of observational studies. J Gen Intern Med. 21(10): 1063–1068.
- Veber D, Mutti E, Galmozzi E, Cedrola S, Galbiati S, et al. (2006) Increased levels of the cd40:Cd40 ligand dyad in the cerebrospinal fluid of rats with vitamin b12(cobalamin)-deficient central neuropa- thy. J. Neuroimmunol. 176: 24–33.
- Waclawik AJ, Luzzio CC, Juhasz-Pocsine K, Hamilton V (2003) Myeloneuropathy from nitrous oxide abuse: Unusually high methylmalonic acid and homocysteine levels. WMJ. 102(4): 43–45.
- Wang H, Li L, Qin LL, Song Y, Vidal-Alaball J, et al. (2018) Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 def- ciency. Cochrane Database Syst Rev. 2018(3): CD004655.
- Xiang Y, Li L, Ma X, Li S, Xue Y, et al. (2021) Recreational Ni- trous Oxide Abuse: Prevalence, Neurotoxicity, and Treatment. Neu- rotoxicity Research. 39(3): 975–985.
- Zheng D, Ba F, Bi G, Guo Y, Gao Y, et al. (2020) The sharp rise of neurological disorders associated with recreational nitrous oxide use in China: a single-center experience and a brief review of Chinese literature. J Neurol. 267(2): 422-429.