Chun Peng Goh1, *, Ira S. Sun2, Shiong Wen Low2
1Division of Neurosurgery, Department of General Surgery, National University Hospital, Singapore.
2Division of Neurosurgery, Department of General Surgery, Ng Teng Fong General Hospital, Singapore.
*Corresponding Author: Goh CP, Division of Neurosurgery, Department of General Surgery, National University Hospital, Singapore
Keywords: primary central nervous system lymphoma, intracranial pressure, dexamethasone
Dear Editor,
It is well-documented that at least 40 % of patients with primary central nervous system lymphoma (PCNSL) show steroid-induced responses, leading to a rapid improvement in clinical symptoms and radiographic features [1], [2].The initial response to steroids is associated with favourable outcomes with definitive treatment [3].
We describe the case of a 64-year-old lady who presented with a three-week history of progressive drowsiness. Her significant past medical history includes left MCA infarct in 2016 with resultant right sided hemiparesis, chronic hepatitis B and diabetes mellitus. Her Glasgow coma scale was E3V3M5, and pupils were 3mm and brisk bilaterally.
Contrasted magnetic resonance imaging (MRI) of the brain (Figure 1) revealed a large lobulated, irregular, enhancing mass with epicentre in the left basal ganglia and extending into the corpus callosum. It measured 5.8 x 4.5 x 5.7 cm (AP x ML x CC) with significant perilesional vasogenic oedema.
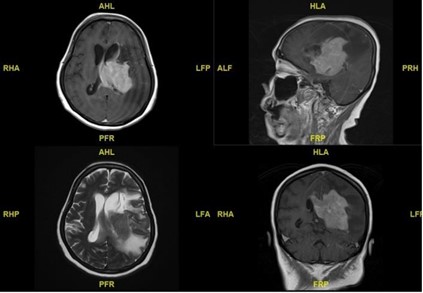
Figure 1: Pre-operative MRI brain showed a large lesion with epicentre in the left basal ganglia
Stereotactic needle biopsy of the tumour was performed, and the intra-op frozen section supported a diagnosis of lymphoma. 8mg of intravenous dexamethasone was given after biopsy. Due to poor GCS pre-operatively, an intra-parenchymal intracranial pressure (ICP) monitor was placed. ICP upon completion of surgery was between 27-30 mmHg. An immediate postoperative CT brain (Figure 2) did not reveal any large haemorrhage. The patient was kept intubated and sedated with propofol 100mg/hr and fentanyl 150 mcg/hr.
Her ICP was still high (up to 21 mmHg) upon arrival in ICU. However, without increasing sedation, and within two hours after dexamethasone administration, her ICP had dropped to 3-7 mmHg. Sedation was weaned quickly, and her GCS improved to E3VtM6. She was successfully extubated the next day. A non-contrasted CT brain (Figure 3) six days after surgery showed significant improvement of mass effect.
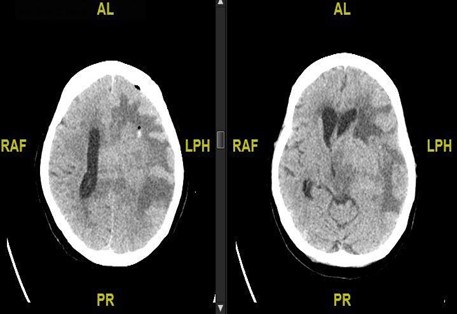
Figure 2: Immediate post-operative CT brain. Left: evidence of pneumocephalus at biopsy site with minimal haemorrhage. Right: Mass effect is like prior MRI brain.
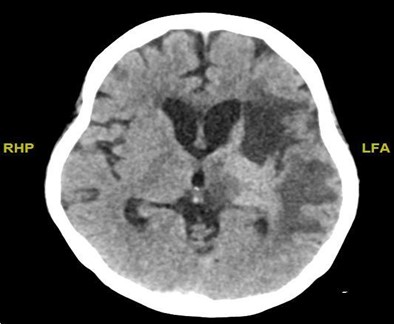
Figure 3: CT brain done six days after surgery which showed significant improvement of mass effect.
We are pleasantly surprised by our patient’s rapid clinical improvement within two hours of dexamethasone administration. It has previously been reported that response may occur ‘within days’ [4], [5].
We believe this is the first time a response in terms of improvement of intracranial pressure is documented. We hope that this may serve as further supporting evidence to encourage early biopsy and corticosteroid commencement for cases of primary CNS lymphoma.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers bureaus; membership, employment, consultancies, stock ownership or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Heckmann JG, Bockhorn J, Stolte M, Druschky A, Neundorfer B (1998) An instructive false diagnosis: steroid induced complete remission of a CNS—probably lymphoma. Neurosurg Rev 21: 48 -51.
- Paydas S (2017) Primary central nervous system lymphoma: essential points in diagnosis and management. Medical Oncology 34(4): 61.
- Mathew BS, Carson KA, Grossman SA (2006) Initial response to glucocorticoids 106(2): 383-387.
- Bromberg JEC, Siemers MD, Taphoorn MJ (2002) Is a “vanishing tumor” always a lymphoma? Neurology 59(5): 762-764.
- Weller M (1999) Glucocorticoid treatment of primary CNS lymphoma. J Neurooncol 43: 237-239.



