Gibello U1, Bezzi M1*, Guaschino L2, Della Ferrera F2, Appendino P3
1DDS, Private Practice in Turin, Italy
2DDS, Department of Dentistry and oral Surgery (DDOS); Mauriziano Umberto I Hospital, Turin, Italy
3MD, DDS, Department of Dentistry and oral Surgery (DDOS); Head of Dentistry Unit, Mauriziano Umberto I Hospital, Turin, Italy
*Corresponding Author: Marta Bezzi, DDS, Private Practice in Turin, Italy.
Abstract
A radicular cyst is an inflammatory cyst and it is one of the most common and significant types of cystic lesion affecting the jaw.
It is a chronic inflammatory response to the epithelial rest of Malassez which occurs in the periodontium of affected teeth. It is usually symptomless and detected incidentally on plain OPG.
Several treatment options are available for a radicular cyst such as surgical endodontic treatment, extraction of the offending tooth, enucleation with primary closure, or marsupialization followed by enucleation.
We present a case of radicular cyst in a 61-years-old female patient and the treatment of this based on a review of the literature.
Keywords: Radicular cyst; Non-vital tooth; Enucleation; Root canal treatment.
Introduction
The radicular cyst develops at the apex of a necrotic erupted tooth and is one of the most common and significant types of cystic lesion affecting the jaw accounting for about 52 %–68 % of all incidences [1,2,3]. The incidence is highest in the third and fourth decades of life with male predominance [4].
According to the classification of Kramer et al. (1992) is an inflammatory cyst.
Mandibular molars are the favoured site for the development of radicular cysts as they are frequently affected by caries [5,6]. Cortical bone in this region is thick; therefore, lesions may not drain readily through the sinus tract [7,8]. The cyst is believed to form by the proliferation of the epithelial cell rests of Malassezia in inflamed peri radicular tissues [9]. Its size rarely exceeds 1 cm and is usually associated with carious, non-vital, discoloured, or fractured teeth [10,11]. The radicular cyst is usually symptomless and detected incidentally on plain OPG while investigating for other diseases; radiographically, the radicular cyst appears as a well-defined round or oval unilocular radiolucency with a radiopaque sclerotic margin in the periapical region of involved tooth [12].
The vitality test is essential for the diagnosis: the vitality of the tooth involved would rule out the presence of a radicular cyst.
Radicular cysts are generally considered to be the direct consequence of a periapical granuloma, but less than 20 % of granulomas have this type of evolution.
Several treatment options are available for a radicular cyst such as surgical endodontic treatment, extraction of the offending tooth, enucleation with primary closure, and marsupialization followed by enucleation [11].
The purposes of this paper were to report the case of a 61-year-old female patient with a radicular cyst in mandibular molar teeth and the treatment of this based on a review of the literature.
Case Report
A 61-year-old female patient was reported to S.C. of Odontostomatology of the A.O. Mauriziano of Turin in July 2020, with a chief complaint of pain related to the third quadrant and swelling.
The patient refers to a previous history of melanoma (1998), and at present the daily intake of escitalopram and delorazepam.
The orthopantomography, carried out at the diagnostic radiology service, shows a large radiolucent with a sclerotic radiopaque margin involving the root apexes of elements 36 and 37 and the crown of element 3.8 included in the mesh version. [Figure 1-2]
The second level radiographic examination (CT cone beam) confirms the reports of the radiolucent lesion with the apexes of the elements. [Figure 3].
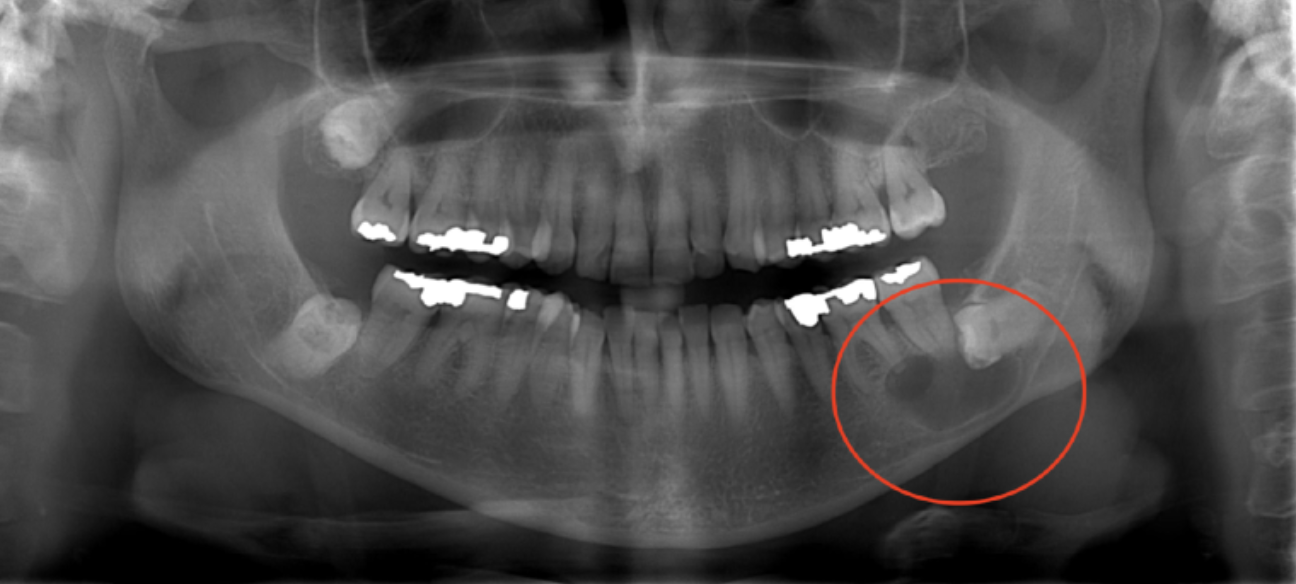
Figure 1: Orthopantomography: large radiolucent with a sclerotic radiopaque margin involving the root apexes of elements 3.6 and 3.7 and the crown of element 3.8 included in mesioversion

Figure 2: Intraoral radiography

Figure 3: CT cone beam
On clinical examination there was a voluminous swelling at the fornix of elements 3.6 and 3.7; the opening of the mouth is limited.
Elements 3.6 and 3.7 were subjected to periodontal probing, which was negative, and the absence of viability was confirmed through a viability test with cryospray and electrical.
Clinical, radiographic examination, and excisional biopsy reports were suggestive of a radicular cyst associated with mandibular left molars.
The histopathological examination confirmed the provisional diagnosis of a radicular cyst.
It showed the presence of stratified squamous epithelium with sub- adjacent granular tissue and inflammatory infiltration.
Procedure
The patient was informed about the treatments she must undergo and signed informed consent.
The patient first underwent root canal therapy of elements 36 and 37. During the first session, the endodontic treatments of elements 3.6 and 3.7 were performed.
The treatment, despite the total absence of vitality, was conducted with an inferior alveolar nerve block (IANB) with mepivacaine without a vasoconstrictor.
In both elements, 3 root canals were found.
Element 3.6 had 2 mesial canals 22 mm long, shaped with the Protaper Next system (Dentsply Sirona) up to X2 (0.25) and filled with a carrier-based system (Thermafil 0.25); the distal canal was shaped up to X3 (0.30) and obturated with a carrier based system (Thermafil 0.30).
Element 3.7 had 2 confluent mesial canals; the main one (lingual month) was shaped with the Protaper Next system up to X2 and filled with Thermafil 0.25, the lingual month up to X1 (at the confluence) and filled with thermal 0.20; the distal was shaped up to X3 and filled with Thermal 0.30.
Both elements were provisionally filled with glass ionomer cement. [Figure 4]

Figure 4: Intraoral radiography: root canal therapy of elements 36 and 37
Then, the patient underwent the extraction of the included element 3.8 and the contextual enucleation of the cyst. The surgery was performed in narcosis.
Local anesthesia was performed with plexus anesthesia with a vasoconstrictor to reduce bleeding.
A triangular flap was made through an intracellular incision from element 3.4 to 3.7 with distal discharge.
The incision was made with a scalpel, blade 15; periosteal dissection was conducted with Mitchell and Williger, exposing the surgical site. [Figure 5]
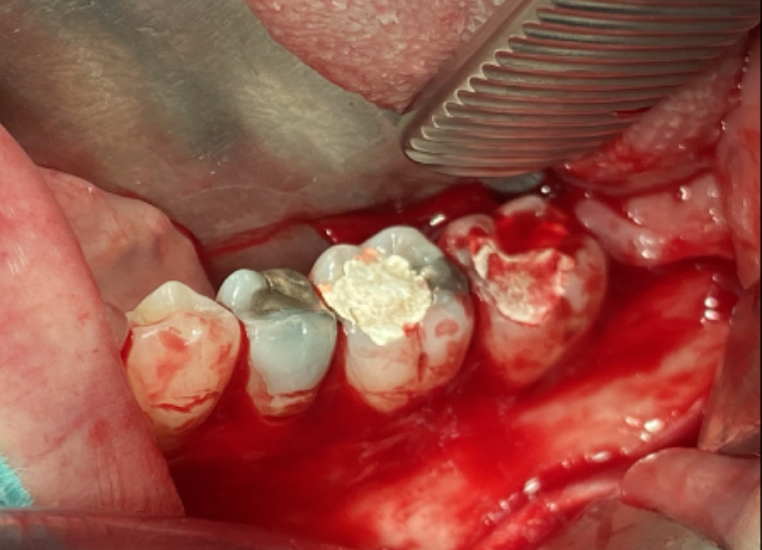
Figure 5: Surgical site after periosteal dissection
The osteotomy followed the fenestration caused by the injury and was performed with a "rosette" bur, used on a low-speed handpiece. The odontology was performed with piezosurgery.
After the odontology procedure, the crown and roots of dental element 3.8 were extracted in two steps.
The lesion was detached from the surrounding bone and enucleated in its entirety. [Figure 6-7-8]The cavity was washed with a physiological solution and the flap was closed with a vicryl 4/0 resorbable suture.
The surgical piece was sent for histopathological examination to the pathological anatomy service of the Mauriziano Hospital.
The postoperative indications were given and a 10-day checkup was performed, simultaneously with the removal of the suture. [Figure 9- 10]
One month after the surgery, the final restorations were made in private dental practice. [Figure 11]
The patient undergoes quarterly follow-ups.An intraoral radiograph was taken during the 6-month follow-up. [Figure 12]
The 1-year control with intraoral radiograph and orthopantomography, confirms almost all of the healing obtained. [Figure 13-14]

Figure 6: Osteotomy following the fenestration
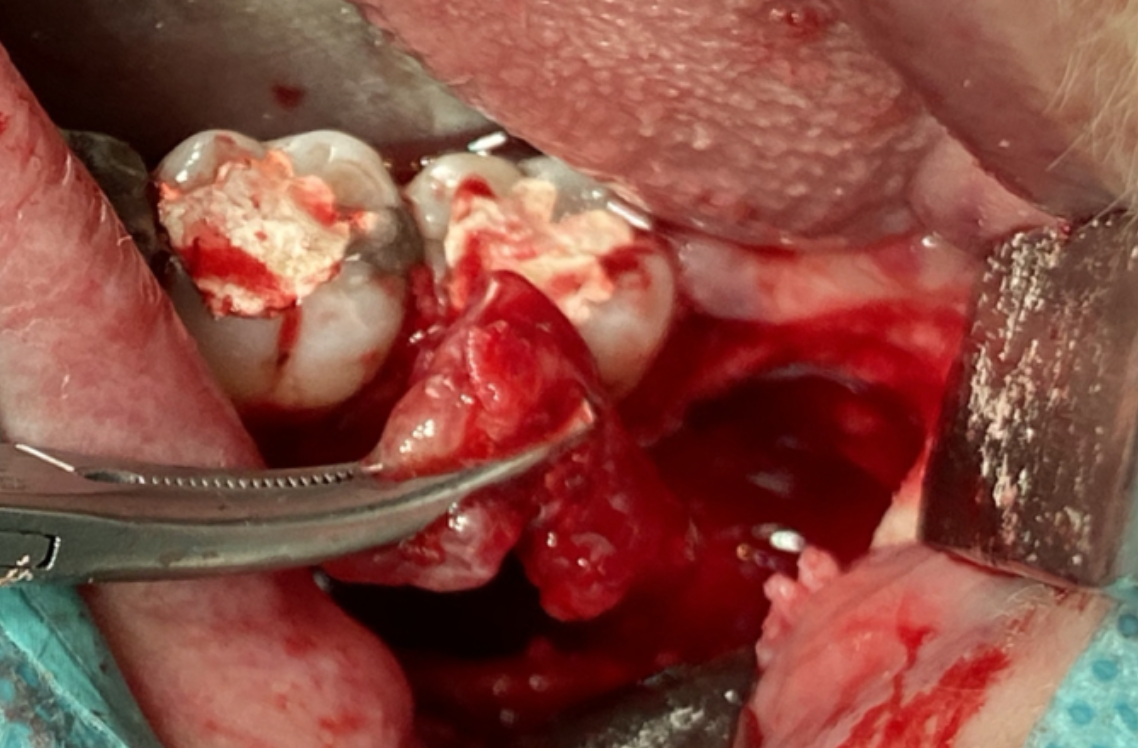
Figure 7: Extraction of the included element 3.8 and the contextual enucleation of the cyst
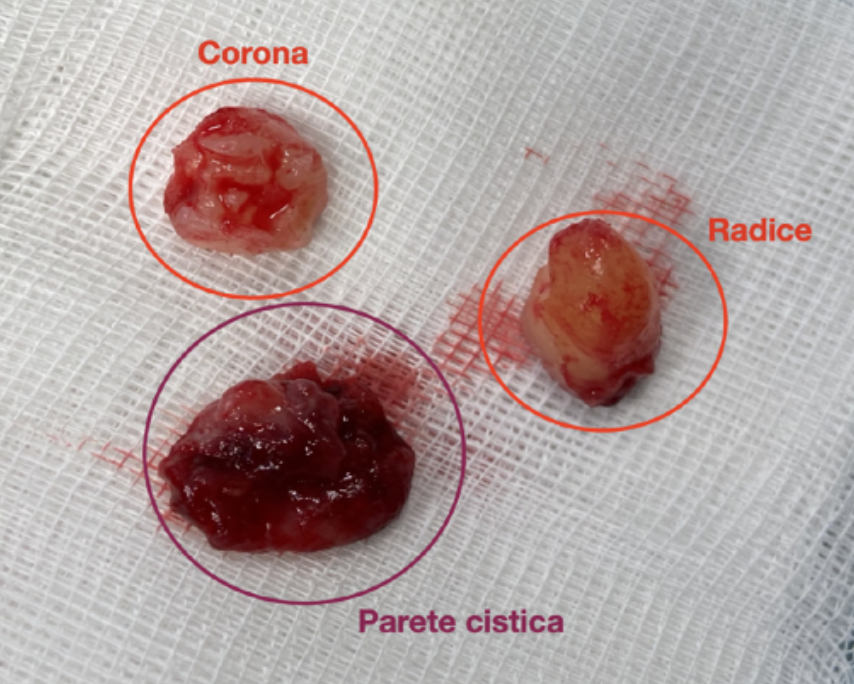
Figure 8: Crown, roots and cystic wall

Figure 9: 10-days control and removal of suture
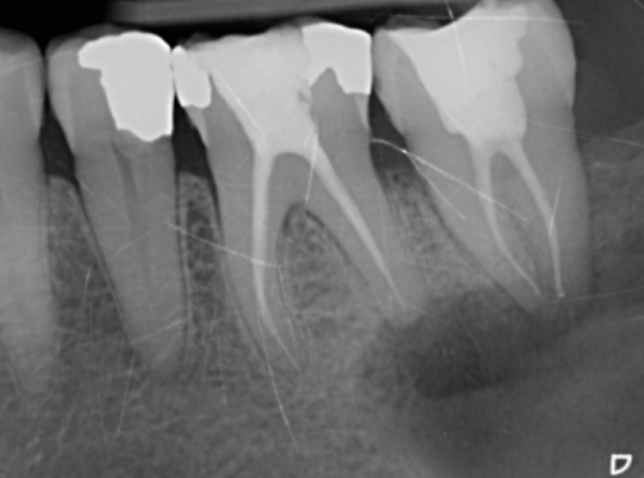
Figure 10: Intraoral radiography

Figure 11: Final restorations of elements 3.6 and 3.7

Figure 12: 6-month control intraoral radiograph

Figure 13: 1-year control intraoral radiograph and orthopantomography.

Figure 14: 1-year control intraoral radiograph and orthopantomography.
Conclusion
Various treatment options have been recommended depending on the size and location of the cyst. The choice of treatment depends on factors such as the extension of the lesion, its relation to the surrounding structures, clinical characteristics of the lesion, and the systemic condition of the patient. Treatment options for radicular cysts may be conventional, nonsurgical root canal treatment when the lesion is confined to a small area or surgical treatment like enucleation, marsupialization or decompression in case of larger lesions, or a combination of these techniques. [13,14] This case report of radicular cyst has been successfully treated by endodontic treatment of elements 36 and 37, extraction of the included element 3.8, and the contextual enucleation of the cyst and curettage.
References
- Riachi F, Tabarani C (2010) Effective management of large radicular cysts using surgical enucleation vs. marsupialization – Two cases report. International Arab Journal of Dentistry (IAJD). 1(1): 44-51.
- Latoo S, Shah AA, Jan MS, Qadir S, Ahmed I, Purra AR. Radicular cyst. JK Sci. 11: 187–9.
- Kolari V, Rao HTA, Thomas T (2019) Maxillary and mandibular unusually large radicular cyst: A rare case report. Natl J Maxillofac Surg. 10(2): 270-273.
- 3rd ed. Singapore: Varghese Publication House; 1992. Mervyn Shear, Cysts of oral regions; pp. 136–70.
- Takiguchi M, Fujiwara T, Sobue S, Ooshima T (2001) Radicular cyst associated with a primary molar following pulp therapy: a case report. Int J Paediatr Dent. 11(6): 452-5.
- Lustig JP, Schwartz-Arad D, Shapira A (1999) Odontogenic cysts related to pulpotomized deciduous molars: clinical features and treatment outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 87(4): 499-503.
- Grundy GE, Adkins KF, Savage NW (1984) Cysts associated with deciduous molars following pulp therapy. Aust Dent J. 29(4): 249-56.
- Sevekar S, Subhadra HN, Das V (2018) Radicular cyst associated with primary molar: Surgical intervention and space management. Indian J Dent Res. 29(6): 836-839.
- Lin LM, Huang GT, Rosenberg PA (2007) Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 33(8): 908- 16.
- Scholl RJ, Kellett HM, Neumann DP, Lurie AG (1999) Cysts and cystic lesions of the mandible: clinical and radiologic- histopathologic review. Radiographics. 19(5): 1107-24.
- Shafer HL. 6th ed. Amsterdam: Elsevier; 2006. Textbook of Oral Pathology.
- Mahesh BS, P Shastry S, S Murthy P, Jyotsna TR (2017) Role of Cone Beam Computed Tomography in Evaluation of Radicular Cyst mimicking Dentigerous Cyst in a 7-year-old Child: A Case Report and Literature Review. Int J Clin Pediatr Dent. 10(2): 213- 216.
- Gonzalez SM, Spalding PM, Payne JB, Giannini PJ (2011) A dentigerous cyst associated with bilaterally impacted mandibular canines in a girl: a case report. J Med Case Rep. 5: 230.
- Mihailova H, Nikolov VL, Slavkov SV (2008) Diagnostic Imaging Dentigerous Cyst of Mandible. J IMAB – Annual Proceeding Scientific Papers.



