Ryan Elshimali MS1, Yahya I. Elshimali MD2, *
1University of California Los Angles (UCLA)
2Charles Drew University of Medicine and Science (CDU)
*Corresponding Author: Yahya I. Elshimali, Charles Drew University of Medicine and Science (CDU)
Abstract
We are reporting a case of papillary carcinoma originating in a branchial cleft cyst (BCC) in an adult patient without evidence of papillary carcinoma in the thyroid gland. Up to our search, there were 11 cases that have been reported in the literature. Whether thyroid carcinoma is originating primarily in BCC or associated with primary thyroid carcinoma or paired with another lateral neck anomaly, all will be discussed in this report as well as a review of the literature.
Keywords: BBC, ectopic thyroid tissue, papillary thyroid carcinoma
Introduction
Branchial cleft cysts are considered the most common masses in the lateral neck and ectopic thyroid tissue within a branchial cleft cyst is an unusual phenomenon. The papillary thyroid carcinoma that arises from this location is extremely rare. Ectopic thyroid tissue can be clinically manifested within all spectra of thyroid nosology, ranging from asymptomatic neck masses to hyperfunctioning ectopic thyroid tissue and thyroid malignancy. The most common location of ectopic tissue is at the base of the tongue, although various cervical or remote sites have been reported. Based on this concept, an ectopic thyroid tissue can be identified on a pre-existing benign branchial neck cleft cyst [1,2,3,4,5].
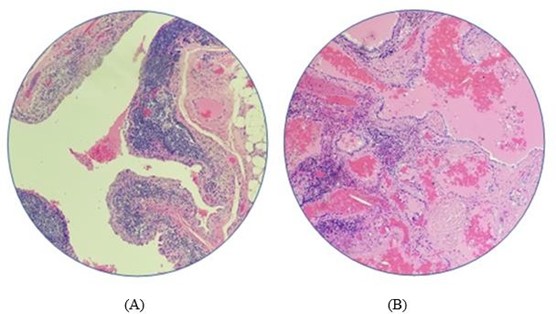
Figure 1: Bronchial Cleft Cyst, A. with normal ectopic thyroid follicles and, B. subepithelial lymphoid aggregate.
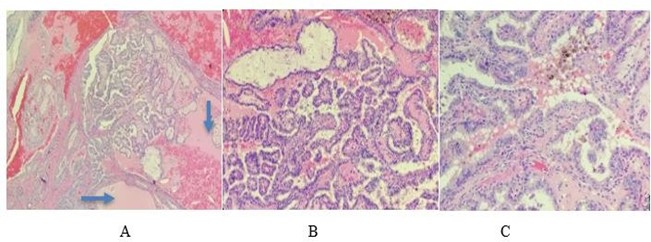
Figure 2: Foci of papillary thyroid carcinoma adjacent to dilated normal thyroid follicles in the wall of the (BCC), A. (x4) Normal (arrows), B. (x10), and C. (x20) Papillary Carcinoma.
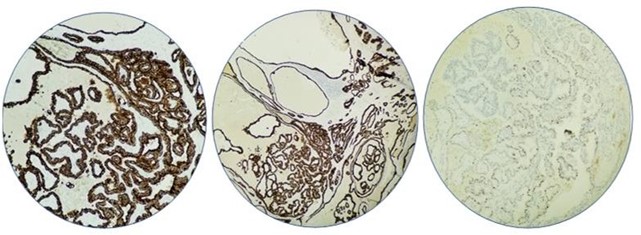
Figure 3: Immunohistochemistry staining for, A. CK19 positive. B. TTF1 Positive, P63 Partially positive
Clinical History
This is a 41-year-old female presented with left supraclavicular cervical lymphadenopathy. The patient noticed induration at the left neck started 6 months ago before presentation and mass started to increase in size with no fever or pain or any other complaints. There was no past medical history of irradiation or trauma to the head and neck and no family history for congenital malformations. all laboratory findings including thyroid function tests were normal. Chest X-Ray was normal, and Cat Scan showed left asymmetric cervical adenopathy with some irregular nodal calcifications measuring approximately 3.4 X 2.7 X 3.2 cm. and the impression was left supraclavicular mass favour malignment adenopathy. Neither FNA nor ultrasound nor thyroid scanning was obtained for that mass. The patient went through a surgical procedure exploring the left neck soft tissue and excision of the cystic mass with adjacent one lymph node. Gross examination revealed cystic mass measuring 3.5 X 2.5 X 2 cm. and cross-sections revealed cystic and solid appearance with light brown gelatinous material. Microscopic examination revealed cystic walls partially lined by respiratory epithelium, and surrounded by fibrofatty tissue with chronic inflammation, hemosiderin-laden macrophages, and lymphoid aggregates with interrupted areas of attenuated or absent overlying epithelium due to inflammatory changes (Figure.1(A)). Ectopic Thyroid tissue with dilated thyroid follicles is found to be embedded within the cystic walls and filled with thyroglobulin (Figure.1(B)). Adjacent to that follicles there are foci of papillary structures with enlarged nuclei, intranuclear cytoplasmic inclusions, nuclear grooves, and fine chromatin (Figure.2). Immunohistochemical stain shows the tumor cells are positive for TTF-1, CK19, and P63 (Figure.3).
Discussion
Most branchial cleft cysts BCC present in late childhood or early adulthood as a solitary and painless mass. They are most commonly located along the anterior border and the upper third of the sternocleidomastoid muscle. they present in one of three forms: cysts, sinuses, or fistulae. Cysts may not present until adulthood and it is considered a congenital malformation that results from failure of the branchial pouch apparatus arising from the first through fourth pharyngeal clefts. The second cleft is being the most common type and the proximity of branchial arches during development may also explain ectopic tissue [1,5,6]. In this case, the correct diagnosis was missed before the surgery, but metastatic malignancy was in the differential diagnosis. Metastatic papillary carcinoma from thyroid to branchial cleft is not uncommon and, in our case, it is favoured that this lesion is originating from ectopic thyroid tissue in branchial cleft cyst because of the presence of adjacent normal and dilated thyroid follicles [7]. As per Sidhu's criteria for the papillary carcinoma in BCC, they were suggested as [8].
- Epithelial lining layer, subepithelial lymphoid tissue collection
- Normal thyroid tissue adjacent to the focus of papillary carcinoma within the wall.
- No evidence of papillary carcinoma in the thyroid or other area.
All the above criteria have been met in this case.
In addition, immunohistochemical staining for TTF-1 was positive but cannot distinguish between primary and metastatic tumors of BCC. The p63 which is a potentially oncogenic protein contributes to the onset of papillary carcinoma. It was suggested that the detection of p63 in papillary carcinomas of BCC could distinguish from primary BCC or metastatic origin. p63 staining on the papillary area of carcinoma of BCC in our case revealed focal positivity. Papillary carcinoma arising from branchial remnants has the ability to metastasize to regional lymph nodes. Neck node metastases are found in 20 %, but distant metastases were not reported. In this case, one lymph node was received, and it was negative for malignancy. Regardless of etiology, the prognosis of patients with carcinoma in lateral neck cysts without a primary site identified after total thyroidectomy appears to be good. This might suggest that removing the cyst is therapeutic if it represents de novo carcinoma in ectopic thyroid tissue. It could also represent a missed primary in the thyroid secondary to a missed microcarcinoma, and thyroidectomy may be considered appropriate treatment [2]. Nevertheless, the differential diagnosis for a lateral cystic lesion includes, lymphadenopathy, hemangioma, carotid body tumor, cystic hygroma, ectopic thyroid or salivary tissue, vascular neoplasm, congenital malformation, and cat- scratch disease. On the other hand, there are no national guidelines for the management of lateral neck cysts. Itis recommended that cases presented with unusual neck cysts in adult life should be considered with high percussion. A thorough history and clinical examination followed by ultrasound and CT scanning of the neck including the thyroid gland are essential. If ultrasound guided FNA was inconclusive, excisional biopsy is mandatory. The therapeutic approach should include surgical excision of the cyst, total thyroidectomy, and rh-TSH-aided radioiodine ablation when indicated
Conclusion
The definite diagnosis of the thyroidal branchial cleft cyst will be made postoperatively; yet if on the fine-needle aspiration of the cyst a yellowish, the pus-like viscous fluid is aspirated, the branchial cleft cyst should be considered in the differential diagnosis of the thyroid cystic lesion. The early diagnosis and treatment without prolonged delay is an important factor in decreasing the mortality rate in such patients [3, 9,10].
References
-
Coste AH, Lofgren DH, Shermetaro C (2020) Branchial Cleft Cyst. Stat Pearls.
-
Rahmat F, Muthu AKM, Gopal NSR, Jo Han S, Yahaya AS (2018) Papillary Thyroid Carcinoma as a Lateral Neck Cyst: A Cystic Metastatic Node versus an Ectopic Thyroid Tissue. Case Rep Endocrinol.
-
Sarmukh S, Sadhana SM, Anita B, Zaidi Z, Wan Z (2017) A Papillary Thyroid Carcinoma Metastasis Mimicking Brachial Cleft Cyst. A Diagnostic Delima. "How We Do It". Nur Primary Care. 1(6): 1-3.



