Ikenna Onwuekwe1, Ijeoma Ndionuka2*, Chidimma Orah2 , Chimdi Chuka-Okosa3, Okereke Edith2, Ezeala-Adikaibe B2, Madu Victor4
1Peenok Medical Centre, Enugu, Nigeria
2Neurology Unit, Department of Medicine, University of Nigeria Teaching Hospital, Enugu, Nigeria
3Department of Ophthalmology, University of Nigeria Teaching Hospital, Enugu, Nigeria
4Neurology Unit, Department of Interna l Medicine, Federal Medical Center Yenagoa, Bayelsa State, Nigeria
*Corresponding Author: Ndionuka Ijeoma B, Neurology Unit, Department of Medicine, University of Nigeria Teaching Hospital, Enugu, Nigeria. PMB 01129 Enugu, Nigeria.
Abstract
Background: Internuclear ophthalmoplegia is a known and readily recognizable condition in Neurology. The same cannot be said of posterior internuclear ophthalmoplegia, which is extremely rare and challenging for many clinicians. No case has been reported from Nigeria.
Case Presentation: A 62-year-old obese male, found to be hypertensive on presentation, was referred to the Neurologist by his Ophthalmologist following sudden onset diplopia and lateral rectus palsy in the setting of severe hypertension. Neurological examination was eventful only for features of a right posterior internuclear ophthalmoplegia. Neuroimaging was unremarkable, while hyperlipidemia was discovered. The patient improved with medical management.
Conclusion: This case highlights the need for a high index of suspicion by Neurologists and clinicians for rare and exquisite neurological syndromes of vascular aetiology.
Introduction
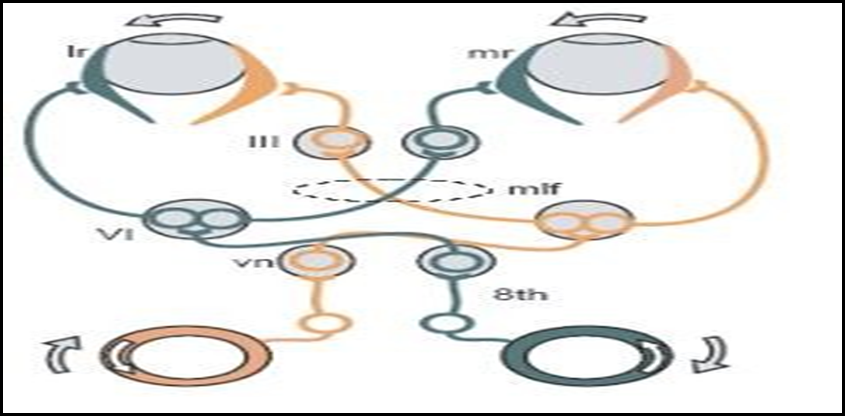
Horizontal gaze requires the yoking together of the two eyes via an intricate relationship whereby abduction of one eye by the 6th cranial nerve nucleus in the pons near the lateral pontine nucleus (the paramedian pontine reticular formation –abducens nucleus complex) is smoothly accompanied by adduction of the other eye via the 3rd cranial nerve in the midbrain. [1] This connection is affected by the medial longitudinal fascicule (bundle), a heavily myelinated tract, and damage to this produces failure of conjugate horizontal gaze (see figures 1 and 2). [1]
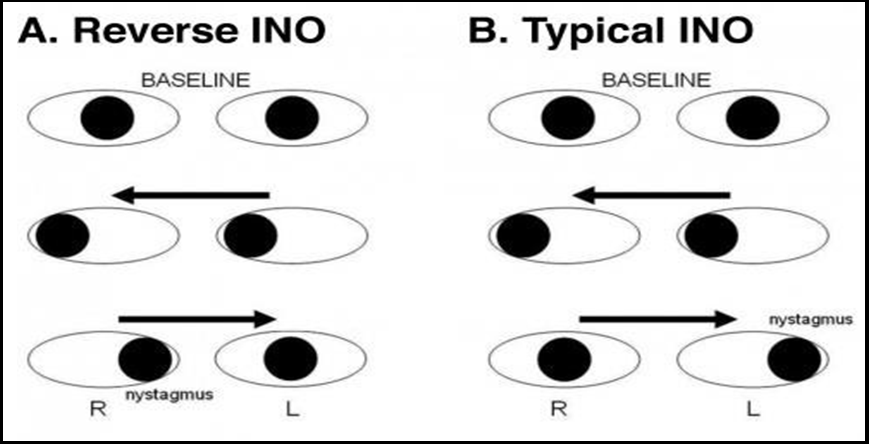
This disconnection between the 6th and 3rd nerve nuclei is called internuclear ophthalmoplegia (INO). Characteristically, there is a loss of adduction (partial or complete) in the eye ipsilateral to the lesion in the fascicule, while abduction in the contralateral eye progresses with ataxic nystagmus. [2] A patient with INO presents with horizontal diplopia in the presence of preserved convergence. The MLF was discovered in the 1870s, while INO was first described in 1903. [3].
Most cases of INO are unilateral and usually are due to ischaemic injury (stroke) in older ages; it can be bilateral and due to demyelination (multiple sclerosis) in children and young people. Other causes exist. [4]
Internuclear ophthalmoplegia (INO) of adduction (Lutz posterior INO, reverse INO, or pseudo abducens palsy) is a rare horizontal gaze palsy. It clinically presents with Abduction limitation and contralateral Adduction nystagmus. [5] This is the reverse of a typical INO with adduction limitation and contralateral abduction nystagmus. Reverse INO can be either unilateral or bilateral.
Figure 1: Horizontal gaze pathway. III, 3rd cranial nerve (oculomotor) nucleus); LR, lateral rectus muscle; MLF, medial longitudinal fasciculus; MR, medial rectus muscle; VI, 6th cranial nerve (abducens) nucleus; VN, 8th cranial nerve (vestibular) nucleus; 8th, vestibular nerve.
Figure 2. Comparison between reverse INO and typical INO (adapted from EyeWiki)
Case Summary
CA, a 62-year-old lawyer, presented to the Neurology Clinic at Peenok Medical Centre, Enugu, South East Nigeria on 9th December 2021 as referred by an Ophthalmologist to whom he had complained about a moderate intensity right temporal and retro-orbital headache of 3 weeks duration (VAS 6/10, throbbing, persistent but intermittently relieved by oral paracetamol). This was associated with blurred vision in the left eye and diplopia when looking to the side. Significant findings by the referring doctor in the eye clinic included changes consistent with glaucoma in the left eye, mildly reduced visual acuity in the left eye (6/12) vs right eye (6/6), weakness of the left lateral rectus muscle and a blood pressure of 178/98mmHg. He was not known to be hypertensive, and the doctor placed him on medications, including valsartan/hydrochlorothiazide.
A day before presenting to the Neurology clinic, he woke up to notice an in-turning of the left eye while other complaints persisted. There was no limb or facial weakness, no speech or swallowing difficulty, and no sphincter or memory challenges.
Other than 2 of his siblings who had diabetes, his personal and family history of hypertension was unremarkable. He was a social drinker and never used tobacco. He was married with children and performed his professional work very well.
General examination was notable only for moderate obesity (BMI 34.1 kg/m2). Vitals were good – random blood glucose 114mg/dL; Temperature 36.40C; respiratory rate 20/min; pulse 70/min, average volume and regular with mildly thickened arterial walls. Blood pressure is 100/80mmHg, and normal heart sounds with mildly heaving apex at 5th LICS just lateral to the mid-clavicular line. Neurological examination was eventful only for a convergent squint with mild left esotropia, left adduction nystagmus, and failure of right eye abduction from right lateral rectus palsy. See the attached video recordings of eye findings at the presentation and one-week follow- up at the Neurology clinic.
A clinical diagnosis of a right posterior internuclear ophthalmoplegia, likely due to a discrete ischaemic event in the right side of the pons, was entertained. Relevant investigations were ordered, including brain magnetic resonance imaging (3.5T), complete blood counts, blood lipids and glucose studies, serum electrolytes, urea, and creatinine.
His treatment consisted of dual antiplatelet therapy (DAPT) with aspirin 75mg od and clopidogrel 75mg od, valsartan/hydrochlorothiazide (160/12.5mg) I daily, alpha tocotrienol 50mg od, rosuvastatin 10mg od, ascorbic acid 500mg tid and citicoline/piracetam (500/800mg) I bid.
The only abnormality in the blood workup was hypercholesterolemia. Brain MRI was utterly unremarkable.
By his next visit to the Neurology clinic a week later, the headache had subsided, vision in the left eye was clearer, and double vision had improved, but the ocular findings were still present but not to the same degree. Their blood pressure control was excellent, and he was happier. He is still being followed up, and a comprehensive weight- reducing program has been started.
Discussion
Posterior internuclear ophthalmoplegia of abduction, also known as reverse INO of Lutz, is a gaze abnormality with impaired horizontal eye movement. It is a brainstem syndrome localized in the medial longitudinal fasciculus in the dorso-medial part of the midbrain.
This condition is characterized by an abduction deficit in one eye and contralateral adducting nystagmus.
Following the clinical diagnosis, brain MRI is cardinal in helping to elucidate the aetiology in up to 75% of cases. Higher capacity MRI (> 3.5T) increases the yield. For demyelinating lesions, proton density imaging is ideal. [4]
The index patient, as described, demonstrated all the features of a posterior INO. Though the MRI was expected, modifiable risk factors for cerebrovascular disease (hypertension, obesity, and hyperlipidemia) strengthen the invocation of a vascular etiology, likely subtle ischaemic pontine infarction. [5]
There is no published case of posterior INO in Nigeria, and there could be unrecognized cases being misdiagnosed by clinicians. This case calls for greater vigilance and a high index of suspicion. Familiarity with neuroanatomy and neuro-ophthalmic examination helps.
There is no specific treatment for the INO of abduction itself. The underlying disease should be worked up and managed appropriately. For symptomatic diplopia, treatment options include fogging one glass lens, patching one eye, a Fresnel prism or ground-in prism glasses, or strabismus surgery. Recovery is more likely if INO is isolated and unaccompanied by other neurological signs. [4] Some clinical recovery was noted one week later in the index patient; double vision resolved, headaches subsided, and ocular findings were slightly improved.
Little is documented regarding the prognosis of INO of abduction due to its rare presentation. Typical INO due to ischemia is expected to resolve in 2-3 months, [6] similar to other vascular cranial neuropathies causing external ophthalmoplegia. INO due to ischemia, multiple sclerosis, or infection can spontaneously resolve over 3-9 months. However, it has been described to persist for more than 12 months in some cases. [4] With the trajectory of recovery seen in the index patient, a favorable prognosis is envisaged.
Conclusion
This case report is intended to highlight the possibility of clinicians encountering rare and obscure neurological disease entities. Prompt referral to the Neurologist is critical for ensuring elucidation and proper management.
Acknowledgment
The authors are grateful for the support of Peenok Medical Centre, Enugu, Nigeria, medical staff in managing this case.
Disclosure: The authors have nothing to disclose.
Ethical approval was obtained from the University of Nigeria Teaching Hospital, Enugu, Nigeria.
References
- Harrison MJG (1996) Clinical skills in Neurology. Butterworth Heinemann. Oxford. 24-28.
- Keane JR (2005) Internuclear ophthalmoplegia: unusual causes in 114 out of 410 patients. Arch Neurol. 62(5): 714-7.
- Feroze KB, Wang J (2022) Internuclear ophthalmoplegia. Stat Pearls Publishing.
- Internuclear ophthalmoplegia. The Lecturio Medical Concept Library. Retrieved 15 December 2021.
- Fiester P, Baig SA, Patel J, Rao D (2020) An Anatomic, Imaging, and Clinical Review of the Medial Longitudinal Fasciculus. J Clin Imaging Sci. 10: 83.
- Caroline W, Al-Zubidi N, Bindiganavile SH, Bhatti T (2022) Internuclear Ophthalmoplegia of Abduction (Lutz Posterior INO). American Academy of Ophthalmologists. EyeWiki.