Cissé Mohamed El Hassimi1*, Diop Abdoulaye2, Koumaré Izoudine Blaise1, Diallo Oumar3, Touré Assa Badiallo4, Diallo Hassane5, Ouologuem Madani5, Diarra amadou Salia1
1Neurosurgery Department of the Mother-Child Hospital Center “Le Luxembourg”, Bamako, Mali
2Neurosurgery Department of the Zinguinchor Regional Hospital
3Ophthalmology Department of the Mother-Child Hospital Center “Le Luxembourg”, Bamako, Mali
4Cardiology Unit of Army Medical-Surgical Center of Bamako, Mali
5Neurology Unit of Army Medical-Surgical Center of Bamako, Mali
*Corresponding Author: Cissé Mohamed El Hassimi, Neurosurgery Department, Luxembourg Mother and Child Hospital Center, Bamako, Mali.
Abstract
Carotid-cavernous fistula (CCF) is an abnormal direct communication between the internal carotid artery (ICA), external carotid artery, and the cavernous sinus. It is a rare vascular complication of TCE, which can jeopardize visual and vital functional prognosis. We report a case of late discovery in our context of a deficient technical platform. A 15-year-old patient presented 3 years after a traumatic brain injury: headaches with pulsatile right eyelid swelling surmounted by collateral venous circulations associated with exophthalmos. CT angiography found a right direct carotid-cavernous fistula Type A of the Barrow classification. In the absence of endovascular embolization in our country, coupled with the patient's financial problems, symptomatic and conservative treatments were carried out without success.
Keywords: Fistula, Carotid-cavernous, TBI, Complications
Introduction
Carotid-cavernous fistula (CCF) is an abnormal direct communication between the internal carotid artery (ICA) and the external and cavernous sinus. FCC can be spontaneous, but in the majority of cases, it is post-traumatic by TBI (Traumatic brain injury) or iatrogenic trauma (endovascular intervention or trans-sphenoidal surgery) [1]. This is a rare vascular complication of TBI, which can be early or late but severe [2]. It can jeopardize visual and vital functional prognosis due to subarachnoid or cerebral hemorrhage [3]. Its clinical manifestations are essentially ophthalmological in a post- traumatic context. Angio - CT (computed tomography) and angio- MRI (magnetic resonance imaging) can help with diagnosis, but the gold standard remains arteriography [1]. Endovascular embolization of the fistula is the ideal therapeutic method that has truly changed the prognosis of FCC [1, 4]. We aim to report a case of a late discovery that we took care of in the context of a deficient technical platform.
Case
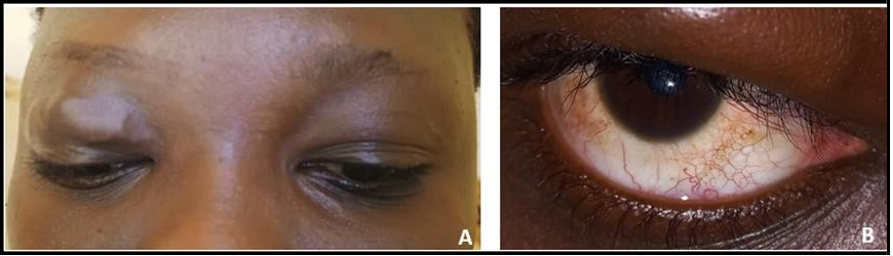
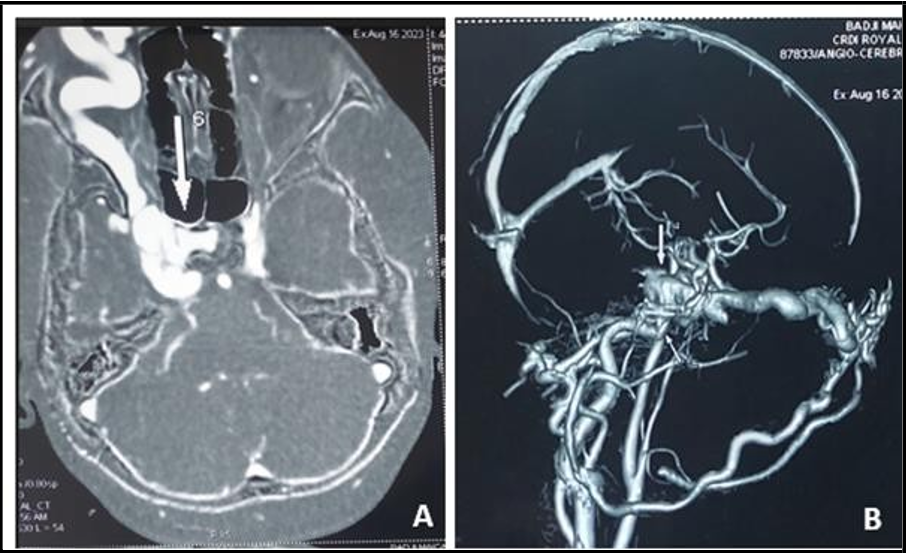
A 15-year-old patient with a notion of TBI and initial loss of consciousness due to a road accident in March 2020, which led to hospitalization in intensive care at the Mopti Regional Hospital for 8 days. She was subsequently transferred to Bamako for further treatment in several hospital centers. She consulted us on August 14, 2023, for moderate chronic headaches with hyperalgesia episodes accompanied by reduced visual acuity, dizziness, and right eyelid swelling of fluctuating volume. These manifestations began approximately 4 months after the trauma and had been evolving for 3 years. The examination found a pulsatile right eyelid swelling surmounted by numerous collateral venous circulations associated with mild exophthalmos without oculomotor disturbance (CF. Figure 1). The ophthalmological examination noted visual acuity 10/10 and normal ocular tone in both eyes. In the right eye, the examination revealed eyelid edema with turgor of the vessels of the right eye and turgor of the retinal vessels. Cerebral angio-CT demonstrated a direct abnormal arteriovenous shunt between the right internal carotid artery and the ipsilateral cavernous sinus at the level of the carotid siphon, responsible for an enlargement of the cavernous sinus, a significant dilatation of the superior ophthalmic vein, its branches, the episcleral veins, and the ciliary veins (Cf. Figure 2). There was grade I exophthalmos. CT angiography confirmed the diagnosis of right direct carotid-cavernous fistula Type A of the Barrow classification. The patient was placed on analgesic treatment while awaiting evacuation for endovascular embolization of the lesion, which is not practiced in our country. Due to a lack of funding for treatment, the evacuation was not carried out. We performed conservative treatment with daily alternative manual compression for 4 weeks without success because the eyelid swelling persisted.
Figure 1: Photograph of the patient showing A: right exophthalmos with eyelid edema and collateral vein circulation. B: dilation of the episcleral veins
Figure 2: Angio – cerebral CT A: enlargement of the cavernous sinus associated with significant dilatation of the right superior ophthalmic vein. B: arteriovenous shunt between the right internal carotid artery and the ipsilateral cavernous sinus at the level of the carotid siphon; responsible for an enlargement of the cavernous sinus, a significant dilatation of the superior ophthalmic vein and the ciliary veins.
Discussion
CCF is an abnormal direct communication between the ICA, the external carotid artery (ECA), and the cavernous sinus [1, 5]. CCF can be classified according to anatomical criteria into direct or indirect (dural) fistula. According to hemodynamic criteria, high-flow CCF is separated from low-flow CCF [1, 6]. Based on angiographic criteria, Barrow et al. [5] established a classification as Type A: direct shunt between the ICA and the cavernous sinus; Type B: dural shunt between the meningeal branches of the ICA and the cavernous sinus; Type C: dural shunt between the meningeal branches of the ECA and the cavernous sinus; Type D: dural shunt between branches. According to pathogenic criteria, spontaneous fistulas are distinguished from post-traumatic fistulas. They can be improvised in almost 30% of cases due to the rupture of an intracavernous aneurysm in a predisposing area such as Ehlers-Danlos disease or fibromuscular dysplasia [1,6]. In the majority of cases, between 70 and 75%, they are post-traumatic [1,3,7]. It is a rare vascular complication of TBI with skull base fracture [2]. Direct or indirect craniofacial trauma may be responsible for a weakening or laceration of the muscular wall of the ICA, causing a vascular shunt from a high-flow artery into a low- flow venous sinus. The fistula is thus formed [6].
Post-traumatic FCC is not exceptional but is rarely reported [2]. Most authors declare only one or two cases [3,4,7,8,9,10,11,12]. Post- traumatic CCF often occurs in young males and is believed to be high- flow fistulas. Our case is female, as in Boukili [8].
Clinically, the time for symptoms to appear varies from a few hours to several months after the trauma [3]. For our patient, this period was 4 months. However, the progression of symptoms before a specialist consultation in our patient (3 years) is very long and reflects the diagnostic delay. This long duration of the evolution of the order of several years is also observed in Boukili [8], Bilong [13], and Ikhloufi [4], who reported 2 years, 3 years, and 5 years, respectively. This is a condition whose symptoms can appear slowly and gradually worsen, which explains patients' negligent or accommodating attitude. The clinical picture is dominated by ophthalmological manifestations [1,3,5]. It is classically unilateral pulsatile exophthalmos accompanied by eyelid edema with dilation of the venous network of the upper eyelid, dilation of the retinal veins, reduced visual acuity, oculomotor paralysis, and the perception of an intracranial murmur by the patient [8]. At an early stage of trauma, these signs may be missing or masked in cases of craniofacial trauma with significant facial edema [10]. CCF will be revealed several months, even several years after the trauma by headaches, ophthalmological manifestations, or more rarely by subarachnoid hemorrhage. In our patient, these were headaches associated with pulsatile exophthalmos, eyelid edema, and turgor of the eye vessels. Ikhloufi et al. [4] also reported headaches associated with ophthalmological manifestations in their patient.
Exploration by medical imaging is an essential element of diagnosis. Color Doppler ultrasound makes it possible to confirm the arteriovenous fistula by showing at the level of the ophthalmic veins an inverted Doppler signal directed towards the face with systolic enhancement. Transcranial Doppler directly visualizes the fistula with a sensitivity of 95% [2, 3]. CT angiography shows indirect signs of CCF, such as dilation of the superior ophthalmic vein on the side of the fistula, enlargement of the cavernous sinus, the presence of bone splinters next to the cavernous sinus, and exophthalmos [1]. Angio-MRI in the T1 sequence shows the dilation of the superior ophthalmic vein and the enlargement of the ipsilateral cavernous sinus. It allows better visualization of the cavernous sinus in the T2 sequence [10]. The "time of flight" sequence of 3D MRI angiography identifies the CCF with a sensitivity of 83% and a specificity close to 100% [2,10]. However, cerebral arteriography remains the gold standard for the definitive fistula diagnosis, and the precise identification of the vessels involved [1]. It also makes it possible to carry out the embolization treatment by endovascular route [1,2,3,10]. In our patient, due to a lack of financial resources and the absence of arteriography in our country, only CT angiography was performed. She confirmed the diagnosis of right direct carotid-cavernous fistula Type A of the Barrow classification. This is the most common type of post-traumatic CCF. In our case, it was thanks to CT angiography that Ben Elhend [9] and Bilong [13] diagnosed CCF.
The standard treatment for CCF is endovascular embolization using interventional radiology [1,6,7,11]. The objective is occlusion of the fistula using releasable intravascular balloons or coils while respecting the patency of the carotid axis. Single-stage arteriography and embolization have considerably improved the prognosis of CCF [3]. Neurosurgical treatment by arterial ligation, clipping, or packing of the cavernous sinus is invasive and risky, with a low success rate of 31% to 79%. Surgical treatment remains difficult to achieve [12]. Conservative therapy with daily alternative manual compression for 4 to 6 weeks is possible in low-flow fistulas to cause thrombosis of the fistula. This method only results in the closure of the fistula in 30% [1]. This is a method that we used without success in our patient due to a lack of financial resources and the availability of endovascular embolization in Mali.
Conclusion
CCF is a rare and potentially dangerous vascular complication of TBI that must be systematically considered in front of exophtalmos and pulsatile eyelid swelling. Cerebral angio-CT, which is an unscrambling examination, allowed us to make the diagnosis in the absence of arteriography. Endovascular embolization, unavailable in Mali, remains the essential therapeutic means for the ideal management of this pathology.
References
- Henderson AD, Miller NR (2018) Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye (Lond). 32(2): 164-172.
- Gagnon N, Debien B, Baccialone J, Perez JP, Pats B (2006) Carotido-cavernous fistula after traumatic brain injury: an unusual vascular complication. Annales Françaises d'Anesthésie et de Réanimation. 25(8): 891-894.
- Hmamouchi B, Rakaa A, Alhyene I, Bouderka MA, Abassi O (2001) Fistules carotido-caverneuses post-traumatiques. Annales Françaises d'Anesthésie et de Réanimation. 20(5): 494-497.
- Ikhloufi ME, Boutimzine N, Cheikh E, El Hassani M, Cherkaoui O (2020) Fistule carotido-caverneuse géante post-traumatique Traumatic Carotid-Cavernous Sinus Fistula. Int. J. Adv. Res. 8(10): 922-925
- Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, et al. (1985) Classification and treatment of spontaneous carotid- cavernous sinus fistulas. J Neurosurg. 62(2): 248-56.
- Fattahi TT, Brandt MT, Jenkins WS, Steinberg B (2003) Traumatic carotid-cavernous fistula: pathophysiology and treatment. J Craniofac Surg. 14(2): 240-6.
- Oulali N, Moufid F, Khoulali M, Sekhsoukh R, Housni B, et al. (2012) Une masse palpébrale révélant une fistule carotidocaverneuse. Pan Afr Med J. 13: 49.
- Boukili K, Elmaaloum L, Allali B, Elkettani A (2021) Exophtalmie tardive révélant une fistule carotido-caverneuse post traumatique: à propos d’un cas. Pan Afr Med J. 39: 153.
- Ben Elhend S, Doulhousne H, Rokhssi R, Mouhsine A (2020) Fistule carotido-caverneuse: à propos d’un cas. PAMJ - Clinical Medicine. 2: 124.
- Gassab E, Krifa N, Tayeb T, Sayah N, Toumi S, et al. (2010) Fistule carotido-caverneuse post-traumatique. J. tun ORL. 25: 76- 80.
- Tokpa A (2020) Fistules carotido-caverneuses directes post - traumatiques : deux cas cliniques. Journal De Neurologie, Neurochirurgie Et Psychiatrie. 1(20): 28–31.
- Oumellal J, Bekaert O, Gallas S, Leguerinel C, Palfi S, et al. (2015) Fistules carotido-caverneuses post-traumatiques à propos d'un cas et revue de la littérature. Pan Afr Med J. 21: 290.
- Bilong Y, Goune CM (2016) Fistule carotido-caverneuse indirecte post traumatique: diagnostic indirect en contexte limitée. Pan Afr Med J. 24: 72.