V. S. Sakthivel 1, *, Caroline Rajprabhu2, V. Rajprabhu3, C. Gokula Krishan4
1MDS OMFS, Velss dental care, Chennai, India.
2MDS periodontics, Mylai dental and implant centre, Mylapore Chennai, India.
3MDS OMFS, Mylai dental and implant centre, Mylapore, Chennai, India.
4MDS OMFS, C.R. Dental and implant centre, Valasaravakkam, Chennai, India.
*Corresponding Author: V. S. Sakthivel, MDS OMFS, Velss Dental care, Chennai, India.
Abstract
Salivary gland tumors are rare and account for 2–3 % of tumors occurring in the head and neck. Pleomorphic adenoma is a benign neoplasm that is commonly encountered in the parotid gland and other major salivary glands. At times they can also develop in minor salivary glands of the palate. The majority of minor salivary gland tumors are malignant. This case report describes a case of a mixed tumor in a minor salivary gland of the hard palate.
Keywords: pleomorphic adenoma, minor salivary gland tumor, palate.
Introduction
Pleomorphic adenoma (PA), which is the most common tumor of salivary glands, is a benign neoplasm consisting of cells exhibiting the ability to differentiate between epithelial cells and mesenchymal cells. The parotid gland is the most common site (90 %). Approximately, 8 % of PA involves the minor salivary glands. As far as intraoral salivary glands are concerned, palate (42.63 %) is the most affected site followed by lip (10 %), buccal mucosa (5.5 %), retromolar area (0.7 %), and lastly affecting the floor of the mouth. Palatal PA presents clinically as a painless, slow-growing mass found on the junction of the hard and soft palate which extends in a posterolateral direction that does not cause ulceration of the overlying mucosa. But these tumors are known to cause underlying bone erosion. Pleomorphic adenomas may occur at any age, but mainly they affect patients in the fourth, fifth, and sixth decades. Forty percent of them are male, sixty percent are female. The potential risk of the PA becoming malignant is about 6 %.
Case report
A 45-year-old male patient came to the Velss Dental care with the complaint of pain, sensitivity, and swelling in the right upper first molar region. History reveals that the patient had severe attrition in the right upper first molar with swelling in the palate which gradually increased in size. As there was no difference in swelling after the extraction of the upper right first molar, the patient reported back. His intraoral examination revealed a painless swelling in the palate (right side) which was oval-shaped, circumscribed, measuring about 1.5cm in diameter extending from the mesial aspect of canine to mesial aspect of the first permanent molar, 4-5mm below the marginal gingiva in the palate till the mid palatine raphe. On Palpation it was smooth, firm in consistency, and fixed to underlying mucosa. The overlying mucosa was not ulcerated but stretched and appeared to be shinier than other aspects of the palate.
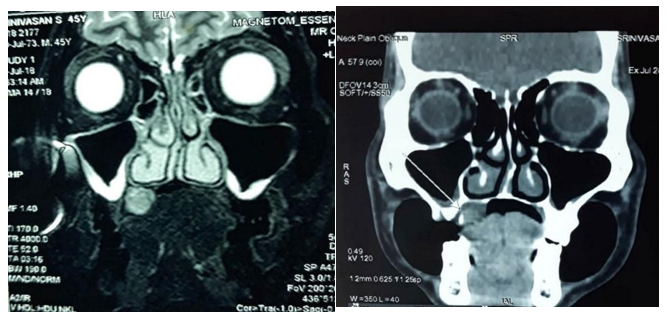
CT scan and MRI revealed a 16mm × 14mm spherical lesion with a small bone defect in the medial aspect of the alveolus at the level of the first molar region adjacent to the lesion with no evidence of erosion of hard palate or extension into the maxillary sinus or nasal cavity. The nasal septum deviated to the left.

Figure1: Preoperative intra oral view showing swelling in the right side of palate
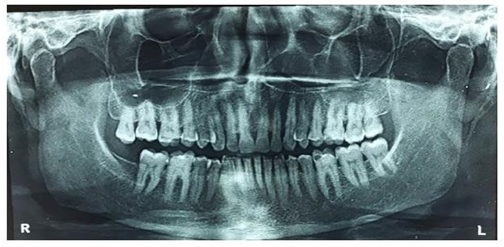
Figure 2: OPG Revealing radiopaque lesion in relation to 16, 17 The differential diagnosis for this case includes palatal abscesses, odontogenic and non-odontogenic cysts, soft tissue tumors such as fibroma, lipoma, and lymphoma as well as other salivary gland tumors. Histology suggested benign salivary gland neoplasm.
Figure 3: (a & b). MRI showing no evidence of erosion of hard palate and extension into maxillary sinus or nasal cavity

Figure 4: Postoperative intraoral view showing excision of the swelling
The lesion was treated by surgical excision and the excised tissue was sent for histopathological examination which further confirmed the diagnosis.
Discussion
The diagnosis of PA is established based on history, physical examination, and histopathology. CT scan and magnetic resonance imaging can provide information on the location and size of the tumor and extension to surrounding superficial and deep structures. The treatment is strictly wide local excision with the removal of periosteum or bone if they are involved. Minor salivary gland tumors are detected and treated earlier than major salivary gland tumors because of difficulty in mastication, speech, and swallowing. If the overlying mucosa is ulcerated malignancy is suspected which is not seen in the present case.
Conclusion
Since the majority of minor salivary gland tumors are reported to be malignant, careful history, patient evaluation, histopathological and radio imaging are advised. With adequate surgical excision, the tumor usually does not recur. Hence, most recurrences can be attributed to inadequate surgical techniques. A long-term follow-up is warranted because of the recurrence even after several years of initial excision.