Nadia Faria Lopes Tavares Matta1, Marcelo Antonini1*, Isabela Bastos Maia1, Anelisa Pinotti Oliveira2, Odair Ferraro1, Reginaldo Guedes Coelho Lopes1
1Mastology Department of Hospital do Servidor Público Estadual – Francisco Morato de Oliveria, São Paulo, Brazil.
2Mastology Departmente of Universidade Federal de São Paulo – UNIFESP
*Corresponding Author: Antonini Marcelo, Mastology Department of Hospital do Servidor Público Estadual – Francisco Morato de Oliveria, São Paulo, Brazil.
Abstract
Introduction: Breast cancer is the most common malignancy in women. However, paraneoplastic neurological syndromes associated with breast cancer are rare and represent a diagnostic and therapeutic challenge. Diagnosing paraneoplastic neurological syndromes is challenging due to the heterogeneity of symptoms, the timing of presentation, and the absence of antibodies. About 80% of patients who develop paraneoplastic neurological syndromes due to breast cancer do not have a cancer diagnosis at the time of presentation.
Case presentation: We describe a 51-year-old patient with bilateral amaurosis who, during etiological screening, tested positive for anti-fishing antibodies, which are rare antibodies associated with paraneoplastic syndrome. The final diagnosis confirmed invasive breast carcinoma of the left breast associated with metastases to contralateral axillary lymph nodes (stage IV - T1N0M1), with bilateral amaurosis resulting from a paraneoplastic syndrome. Systemic treatment for breast cancer was initiated with an aromatase inhibitor (anastrozole), cyclin inhibitor (palbociclib), and ovarian suppression (goserelin). The patient maintained bilateral amaurosis during follow-up, and her oncological condition remained stable without signs of disease progression.
Conclusion: Paraneoplastic neurological syndromes are rare, and often the diagnosis is delayed, as in this case. Anti-fishing antibodies facilitate the diagnosis of this syndrome, and early-stage treatment can provide a good prognosis.
Keywords: Breast cancer, Paraneoplastic neurological syndromes, Bilateral amaurosis, Bilateral optic neuritis.
Introduction
Breast cancer is the most common cancer in women, accounting for 10.4 % of all cancers among women worldwide. The mortality rate has decreased by 34 % over the last 30 years, indicating significant improvements in diagnosis and treatment [1,2]. However, paraneoplastic neurological syndromes (PNS) present a diagnostic and therapeutic challenge in managing breast cancer.
Paraneoplastic syndromes are rare systemic manifestations in approximately 0.01 % to 1 % of cancer patients. PNSs occur in patients with malignancies through an autoimmune mechanism, and these manifestations are not explained by local tumor invasion or metastases. They can present with cerebellar symptoms such as ataxia, nystagmus, and dysarthria, as well as peripheral neuropathies, stiff-person syndrome, encephalomyelitis (including limbic encephalopathy), and paraneoplastic retinopathy. Breast cancers associated with paraneoplastic syndromes are more aggressive and have poor prognoses [3].
Diagnosing paraneoplastic syndromes is difficult due to the heterogeneity of symptoms, the time of presentation, and the absence of antibodies, and it usually occurs before the diagnosis of breast cancer in 80% of patients who develop PNSs [4].
The pathophysiology of paraneoplastic syndromes is a consequence of the natural immune response against neoplastic antigens. Ophthalmic involvement is mainly related to anti-Hu, anti-Yo, anti-CV2/CRMP-5, anti-Ri, anti-Ma2, and anti-amphiphysin antibodies, and their detection is pathognomonic of this syndrome. Paraneoplastic manifestations with ophthalmic involvement are associated with tumors of the lung, breast, ovary, uterus, colon, pancreas, prostate, bladder, and lymphomas. Symptoms include photophobia, decreased visual acuity, decreased color vision, photopsia, central and peripheral scotomas, and night blindness, and may precede malignancy for months or years [5].
We describe a 51-year-old woman with bilateral amaurosis resulting from severe bilateral optic neuritis, which was subsequently diagnosed with breast cancer with metastasis to the contralateral axilla and the presence of anti-amphiphysin antibodies. This case report was approved on February 1, 2023, by the Research Ethics Committee, under CAAE number 64675822.5.0000.5463.
Objective
To report a rare and atypical presentation of breast cancer, diagnosed due to a paraneoplastic syndrome, highlighting the impact of the disease on the patient's quality of life and the importance of suspicion and early diagnosis.
Indeed, here's a translation and some improvements to the writing quality:
Case Report
A 51-year-old premenopausal Caucasian woman with a medical history of hypertension and hypertriglyceridemia presented with severe bilateral optic neuropathy. She had experienced bilateral blurred vision and painless, progressive worsening of visual acuity over a year, which had left her dependent on others for daily activities. Ophthalmologic examination revealed photoreactive isochoric pupils, relative afferent pupillary defect on the left, and bilateral optic disc atrophy, worse on the right. Her visual acuity was 20/70, but her ability to perceive light and colors was better in the left eye. Confrontation, and visual field testing, showed a total scotoma for near objects and a tubular field for distant objects.
Neurological examination was routine, as were breast examinations.
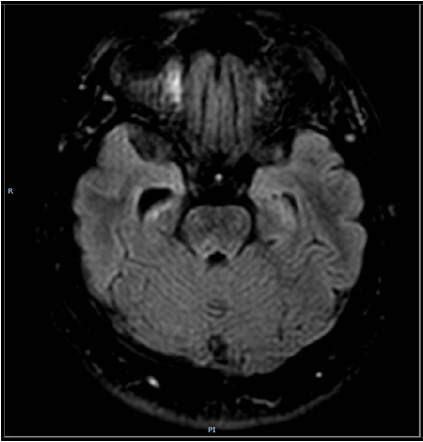
Brain magnetic resonance imaging (MRI) revealed signal changes in the right hippocampus, reduced brain volume, and microangiopathic glucose in the white matter of both cerebral hemispheres (Figure 1). Optical coherence tomography showed ganglion cell loss in the macula, sparing the fovea, and more significant temporal nerve fiber layer loss in the right eye. Orbital MRI showed signal changes in the left intraorbital optic nerve pathway without contrast enhancement, which could be related to optic neuritis without signs of inflammatory activity (Figure 2).
Figure 1: Cranial magnetic resonance imaging showing right hippocampus signal alteration, brain volume reduction, and microangiopathic glucose in the white matter of both cerebral hemispheres.
Figure 2: Orbital magnetic resonance imaging: signal alteration in the left intraorbital optic nerve pathway, without contrast enhancement, which may be related to optic neuritis without signs of inflammatory activity.
Infectious, metabolic, toxic, ischemic, and demyelinating causes were ruled out in the etiological investigation. Routine laboratory tests, antibody evaluations, and cerebrospinal fluid evaluations were standard, except for a positive Anti-Amphiphysin antibody, raising the possibility of paraneoplastic syndrome.
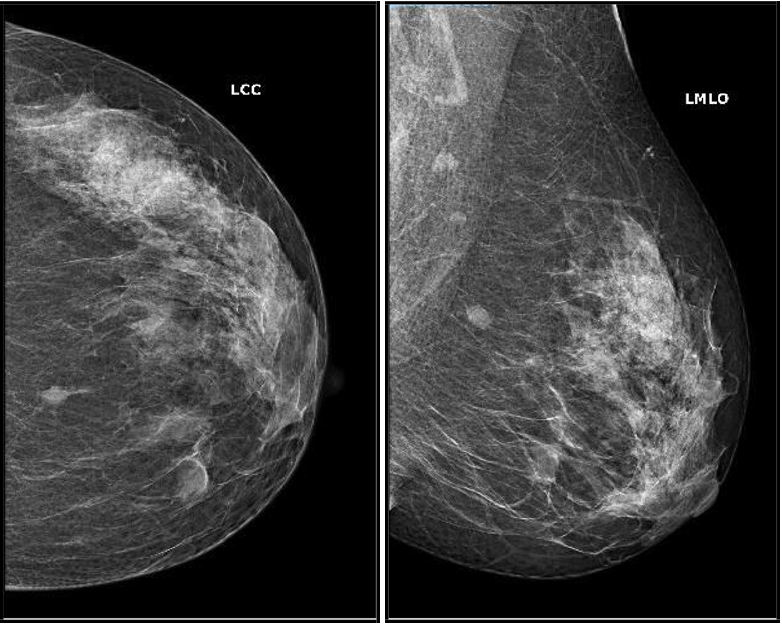
In investigating the primary site of neoplasia, computed tomography of the chest, abdomen, and pelvis, thyroid ultrasound, transvaginal ultrasound, and cervical-vaginal cytology showed no abnormalities. Mammography showed two oval-shaped nodules in the left breast, with partially defined margins: one measuring 1.3 cm in the middle third of the inferomedial quadrant and the other measuring 0.9 cm in the posterior third, at the junction of the medial quadrants (Figure 3). Breast ultrasound revealed a hypoechoic oval nodule with lobulated contours, located in the superomedial quadrant of the left breast at 11 o'clock, measuring 0.9 x 0.7 x 0.5 cm (Figure 4). This was associated with a prominent right axillary lymph node with regular and defined contours measuring 3.1 x 2.6 x 1.3 cm, with signs of cortical thickening and tapering of the central echogenic hilum. A biopsy of the breast nodule revealed invasive breast carcinoma of the non-special type in the left breast, with immunohistochemical evaluation consistent with luminal A tumor (ER+/PR+/Ki67 5%/Her2 negative). A right axillary lymph node biopsy confirmed carcinoma infiltration with the primary site in the breast. PET-CT revealed indeterminate lymphadenopathy in the right axilla, with no other suspected neoplastic sites.
The final diagnosis confirmed invasive breast carcinoma of the left breast, luminal A subtype, with metastasis to the contralateral axilla, stage IV (T1N0M1), associated with the paraneoplastic syndrome of bilateral amaurosis due to severe bilateral optic neuropathy. Systemic treatment for breast cancer was initiated with an aromatase inhibitor (Anastrozole), a cyclin inhibitor (Palbociclib), and ovarian suppression (Goserelin), as the patient was in the premenopausal period. Throughout follow-up, the patient maintained the stability of the oncologic condition, without signs of disease progression, but did not improve her ophthalmologic symptoms, maintaining bilateral amaurosis.
Figure 3: Mammography: 2 oval-shaped nodules with partially defined margins in the left breast: one in the middle third of the inferomedial quadrant, measuring 1.3 cm, and another in the posterior third, at the junction of the medial quadrants, measuring 0.9 cm.
Figure 4: Breast ultrasound: oval-shaped hypoechoic nodule, with lobulated contours, located in the superomedial quadrant of the left breast at 11 o'clock, measuring 0.9x0.7x0.5cm.
Discussion and Conclusion
Paraneoplastic syndromes (PNSs) were first described in 1968 and are rare, occurring in an estimated 0.01 % of cancer patients [5]. PNSs related to breast cancer are rare, with only 56 cases reported in the past 20 years at the Mayo Clinic in the United States [6]. The average age of affected patients was 50 years, and the majority had hormone receptor-positive, HER2-negative breast cancer at stage II [6]. The clinical presentation of PNSs includes paraneoplastic cerebellar degeneration, opsoclonus-myoclonus syndrome, stiff-person syndrome, paraneoplastic neuropathy, and paraneoplastic encephalomyelitis. These syndromes are characterized by antibodies, including anti-Hu, anti-Yo, anti-CV2, anti-Ri, anti- Ma2, and anti-amphiphysin [7].
Diagnosing PNSs can be particularly challenging due to the variability of symptoms and the different onset times. Antibodies are detected in only 70-80 % of patients, and the lack of antibodies does not exclude the presence of PNSs [8]. For this reason, a consensus of neurology experts has defined precise diagnostic criteria. These criteria include the presence of neurological symptoms, a cancer diagnosis within 4 years of the onset of neurological symptoms, exclusion of other neurological syndromes, and at least one of the following: inflammation with negative cytology in the cerebrospinal fluid, magnetic resonance imaging showing a lesion in the temporal lobe, and the presence of epileptic activity in the temporal lobes as determined by electroencephalogram [9,10].
The underlying immune mechanism of SPNs has yet to be well understood. It is well-documented that breast cancer is highly immunogenic, and several shared tumor antigens have been identified [11]. Several studies have confirmed that the loss of the tumor suppressor p53 allows for uncontrolled cell division and the expression of mutant or misfolded proteins ordinarily invisible to the immune system. The presentation of aberrant antigens leads to the expansion of dendritic cells, which carry new antigens through the lymphatic stream after the elimination of cellular debris. Then, the expansion and selection of B and T lymphocyte clones occur in lymphoid organs, ultimately leading to self-recognition and the development of autoimmune and paraneoplastic syndromes [12]. A recent study reported that the tumor microenvironment plays a decisive role in developing humoral paraneoplastic syndromes. Patients with self-reactive T lymphocytes presented higher levels of interferon-alpha and interleukin-12 than autoantibody-negative patients. It is believed that interferon alpha, in particular, supports the expansion and proliferation of T lymphocytes, contributing to the development of SPNs [13].
In SPNs, treatment of the underlying neoplasm is essential. Immunosuppressive therapies can help; however, in some patients, neurological symptoms progress despite treatment. Other immunomodulatory therapies, such as intravenous immunoglobulin and plasmapheresis, have achieved limited benefits in most patients [14].
We report a rare case of a woman with breast cancer and bilateral amaurosis resulting from a paraneoplastic syndrome of severe bilateral optic neuropathy associated with positive anti-amphiphysin antibodies. The neurological symptoms, characterized by blurred vision and progressive low visual acuity, preceded the discovery of breast cancer by 1 year and simulated non-paraneoplastic or neurodegenerative inflammatory syndromes. The breast lesion was, in fact, impalpable on examination and asymptomatic due to its small size. Magnetic resonance imaging showed nonspecific inflammatory signals characterized by signal alteration of the right hippocampus, brain volume reduction, and microangiopathic glucose in the white matter in both cerebral hemispheres. In addition, this subtype of breast cancer (ER+ and HER2-) is the main one associated with SPNs.Parte superior do formulário
The present case illustrates that, although rare, suspicion and recognition of SPNs are essential since neurological symptoms almost invariably precede the direct symptoms of the primary tumor, and early treatment can provide a greater chance of good outcomes. Anti-neural antibodies, such as anti-fifisina, can aid in early breast cancer diagnosis and should be investigated [15]. However, the diagnosis of SPNs is often delayed, as in the presented case. Standard surgical and adjuvant treatments may provide a good prognosis for the patient but may not cure the neurological symptoms.
References
- Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin. 69(1):7–34.
- Mattiuzzi C, Lippi G (2019) Current Cancer Epidemiology. J Epidemiol Glob Health. 9(4): 217–22.
- Piccart M, Lohrisch C, Di Leo A, Larsimont D (2001) The predictive value of HER2 in breast cancer. Oncology. 61(Suppl 2): 73–82.
- Graus F, Dalmau J (2019) Paraneoplastic neurological syndromes in the era of immune-checkpoint inhibitors. Nat Rev Clin Oncol. 16(9): 535–48.
- Darnell RB, Posner JB (2003) Paraneoplastic syndromes involving the nervous system. N Engl J Med. 349(16): 1543– 54.
- Murphy BL, Zalewski NL, Degnim AC, McKeon A, Flanagan EP, et al. (2018) Breast cancer-related paraneoplastic neurologic disease. Breast Cancer Res Treat. 167(3): 771–8.
- Pittock SJ, Kryzer TJ, Lennon VA (2004) Paraneoplastic antibodies coexist and predict cancer, not neurological syndrome. Ann Neurol. 56(5): 715–9.
- Said S, Cooper CJ, Reyna E, Alkhateeb H, Diaz J, et al. (2013) Paraneoplastic limbic encephalitis, an uncommon presentation of a common cancer: case report and discussion. Am J Case Rep. 14: 391–4.
- Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, et al. (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 75(8): 1135–40.
- Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, et al. (2000) Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 123(7): 1481–94.
- Criscitiello C, Esposito A, Gelao L, Fumagalli L, Locatelli M, et al. (2014) Immune approaches to the treatment of breast cancer, around the corner? Breast Cancer Res. 16(1): 204.
- Lu H, Goodell V, Disis ML (2008) Humoral immunity directed against tumorassociated antigens as potential biomarkers for the early diagnosis of cancer. J Proteome Res. 7(4): 1388–94.
- Domschke C, Schuetz F, Ge Y, Rom J, Zorn M, et al. (2011) Determination of paraneoplastic autoimmune responses by tumor cell biology and intratumoral IFN-alpha/IL-12 in breast cancer patients. Cancer Immunol Immunother. 60(3): 401–11.
- Fanous I, Dillon P (2016) Paraneoplastic neurological complications of breast cancer. Exp Hematol Oncol. 5: 29.
- Shams'ili S, Grefkens J, de Leeuw B, van den Bent M, Hooijkaas H, et al. (2003) Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: analysis of 50 patients. Brain. 126(6): 1409–18.