Wania Rafaey *, Anum Latif, Sehba Shamim and Finza Kanwal
Internal Medicine, Liaquat National Hospital, Karachi, Pakistan
*Corresponding author: Dr. Rafaey W, Internal Medicine, Liaquat National Hospital, Karachi, Pakistan
Abstract
Background
COVID-19 pandemic is the biggest public health challenge that world is facing now a days. It has affected different people in different ways. COVID-19 is a systemic infection with a significant impact on the hematopoietic system and hemostasis. Lymphopenia is considered as cardinal laboratory finding with prognostic potential. However, patients can also present with pancytopenia, affecting all cell lineage.
Case Presentation
We present a case of middle-aged male with no prior co-morbid, presented with complaints of fever, cough, and shortness of breath. COVID PCR was positive. Initial lab workup showed pancytopenia with low retic count that improved gradually over a period of four weeks.
Conclusion
COVID-19 is a serious infection that has led to thousands of cases of severe pneumonia, ARDS, and even deaths across the globe. Like other viral diseases, it can also cause bone marrow suppression leading to pancytopenia. This condition improves gradually over a period of weeks to months with supportive management of iron and vit B12 replacement
Case Presentation
42 years old Asian male with no prior co-morbid admitted with complaints of high-grade fever for one week documented up to 102f associated with generalized body aches, dry cough for last 4 to 5 days and shortness of breath on exertion. He was not able to complete sentence without getting short of breath. On arrival in Emergency room, he was conscious, awake, anemic and in respiratory distress with the vitals of Pulse: 120bpm Blood pressure: 100/70 mmgh R/R : 30 breaths per min Temperature : 102°F. SO2 82 % on room air. Bilateral crepitation on chest auscultation. A systolic murmur heard all over the chest, loudest in mitral area (Table 1).
He was managed conservatively with supportive therapy, steroids, and transfusion. He improved clinically and his oxygen requirement gradually decreased. Follow up labs as shown in table 2. He was discharged home with regular OPD follow-ups.
PERIPHERAL SMEAR:
DIMORPHIC PICTURE OF RBCs SEEN+, MICROCYTES+ HYPOCHROMIC+ ANISOCYTOSIS+ POLYCHROMASIA+ TERGET CELLS+ CRENATED RBCs+ TEAR DROP CELLS + POIKILOCYTOSIS+ ROULEAUX+, as shown in figure 1.
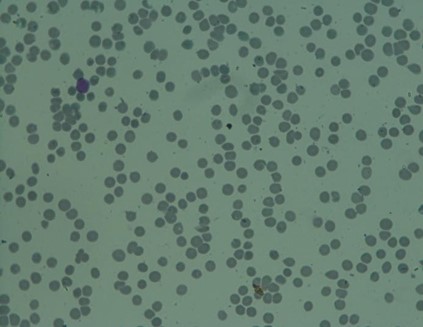
Figure 1: Pathological findings from peripheral smear dimorphic picture of RBCS seen, microcytes, hypochromic, anisocytosis, polychromasia, terget cells, crenated rbcs, tear drop cells, poikilocytosis and rouleaux.
Table 1: Test results
|
Hb |
6.15 g/dl |
|
TLC |
1.72 N 66 % Lymphos 28 % |
|
Platelets |
8 Thousand |
|
MCV |
53.72 |
|
Bilirubin Total |
3.55 Adults: < 1.0 mg/dL |
|
Bilirubin Direct |
1.08 < 0.3 mg/dL |
|
Bilirubin Indirect |
2.47 |
|
ALT |
409 |
|
AST |
428 |
|
D-Dimer |
3.14 |
|
LDH |
421 |
|
High Sensitivity CRP |
17.99 mg/dl |
|
SARS-CoV RNA |
DETECTED |
|
TIBC |
261 [Adults]: 250 - 425 micro gm/dl |
|
Transferrin saturation |
8.00 (30 – 40 %) |
|
Retic count |
0.5 % Normal range: 0.5-2 % |
|
Direct Coombs test |
Negative |
|
Ferritin |
72 Adult F:15-150 ng/ml M:30-400 ng/ml |
Table 2: Follow up test results.
|
Hb |
11.02 11.5 - 15.50 g/dL (F) 13.50 - 17.50 g/dL (M) |
|
MCV |
79.89 (76.0 - 96.0 Fl) |
|
TLC |
6.55 (4.0 - 11.0 x 10^9/L) |
|
Platelets |
166 (150 - 400 x 10^9/L) |
|
Retic count |
1.8 % |
Discussion
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus -2 (SARS-CoV-2). The incubation period of COVID 19 is up to 14 days with an average of 4to 5 days from exposure to symptoms onset [1]. The signs and symptoms of COVID 19 include fever, dry cough, sore throat, shortness of breath on exertion, myalgias, headache, nasal congestion, diarrhea, loss of taste, and loss of smell [2,3]. The severity of illness ranges from mild to critical, mild to moderate disease including mild pneumonia with oxygen saturation ranging from 90-94 % found in 81 %, severe disease includes hypoxia or more than 50 % lung involvement on imaging in 14 % and critical disease includes respiratory failure, shock, or multi-organ system dysfunction in 5 % of the patients [4]. The common hematological complications of COVID 19 include lymphopenia, thrombocytopenia, and increased neutrophil to lymphocyte ratio (N/L ratio) [5]. In literature, no case has been published so far to show the association of COVID 19 with pancytopenia. SARS-CoV-2 virus like other viruses can also causes transient bone marrow suppression that settles gradually over a period of days or weeks.
References
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 382: 1708-1720.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395: 507-513.
- Pan L, Mu M, Yang P, Sun Y, Wang R, et al. (2020) Clinical Characteristics of COVID-19 Patients with Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am J Gastroenterol 115(5):766-773.
- To KK, Tsang OT, Leung WS, Tam AR, Wu TC, et al. (2020) Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis 20(5): 565-574.
- Wu C, Chen X, Cai Y, Xia J, Zhou X, et al. (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180(7): 934-943.



