I. Yazough1*, H. Ouaya2, A. Jbilou1, A. Ahellat1, Y. Agouri1, A. Akjay2, H. Meyiz2, I. Mellouki2, S. Ait laalim1
1Visceral and Endocrine Surgery Department, Mohammed VI University Hospital of Tangier
2Hepato-gastroenterology department, Mohammed VI University Hospital of Tangier
*Corresponding Author: I. Yazough, Visceral and Endocrine Surgery Department, Mohammed VI University Hospital of Tangier.
Abstract
Pancreatoblastoma is a malignant tumor of the pancreas that usually occurs in the pediatric population. The aim of the present study was to highlight this rare clinical entity as well as the description of this double location never described in the literature, by emphasizing the means of preoperative diagnosis and the absence of guidelines in terms of management strategy in adults. Preoperative diagnosis of BP based on radiographic features can be difficult, as imaging features are nonspecific. In addition, cytology can also be misleading.
The aggressive nature of pancreatoblastoma is associated with a poor prognosis in adult patients, but with well-adapted surgical treatment and rapid multidisplin management gives patients good luck.
Introduction
Pancreatoblastoma (PB) is a rare epithelial tumor of the pancreas, usually occurring in the pediatric population, since the first case was published in 1957, more than 200 cases have been described in children, while 70 cases have been reported in adult patients [1,2,3] the location at the level of the head of the pancreas and the most common, whereas the dual location has never been described until today.
Pancreatoblastoma (BP) is a malignant and aggressive tumor, characterized by high rates of local invasion, recurrence, and distant metastatic potential. In addition, adult patients with BP have a poorer prognosis compared to pediatric patients [4]. The associated symptoms are usually vague and the radiological features are nonspecific. Therefore, diagnosis is largely based on the identification of characteristic squamous corpuscles on histopathological examination, which present as whorled nests of flat cells.
Due to its rarity, there are currently no guidelines on protocols for the management of BP. Surgery is considered the main treatment strategy, although the role of radio-chemotherapy remains uncertain and the significant benefits of currently used treatment regimens are limited [4]. This study presents the case of a 17-year-old patient diagnosed with BP with a dual cephalic and caudal location, and it also includes a brief review of the relevant literature. Written informed consent was obtained from the patient's family.
Presentation of the case:
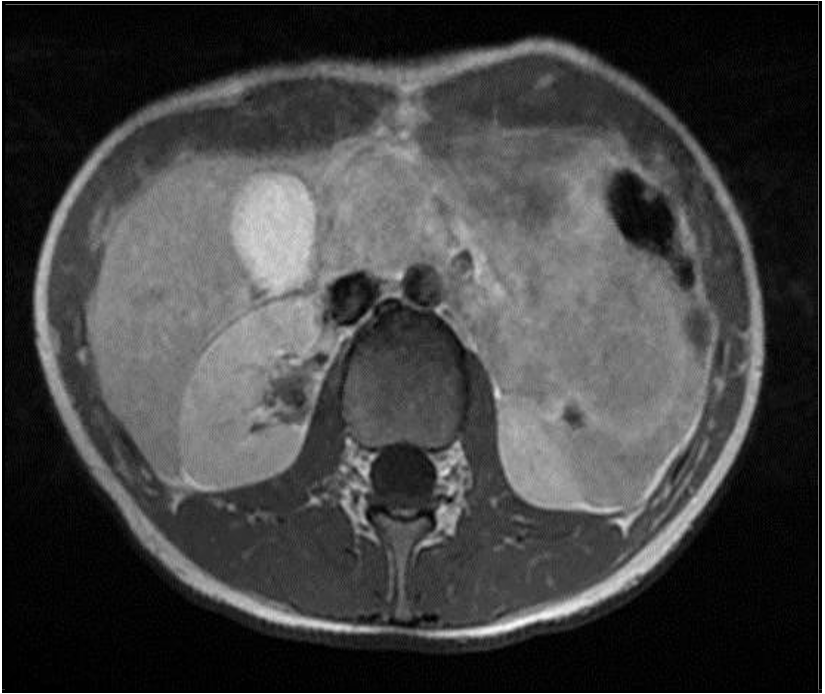
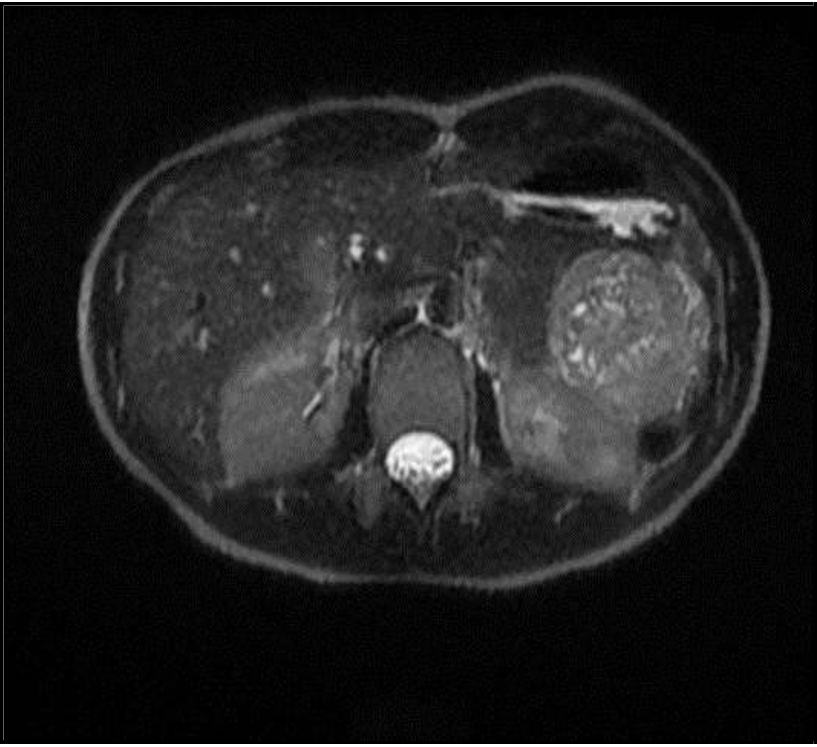
This is a young patient aged 17, with no history, who consulted for left epigastric and hypochondriac pain that had been evolving for 2 months, associated with unquantified weight loss. On clinical examination, epigastric tenderness was noted in a patient in good general condition. A TAP CT revealed pseudocystic formations involving the entire pancreas, the largest measuring 5 cm in the caudal (75 U.H), well limited with thin walls, taking the contrast agent without partitions or micro-calcifications (Figure 1). An MRI confirmed an appearance probably related to a pancreatoblastoma with a double cephalic and caudal location (Figure 2, 3).
Figure 1: T1 MRI image
Figure 2: T2 MRI image
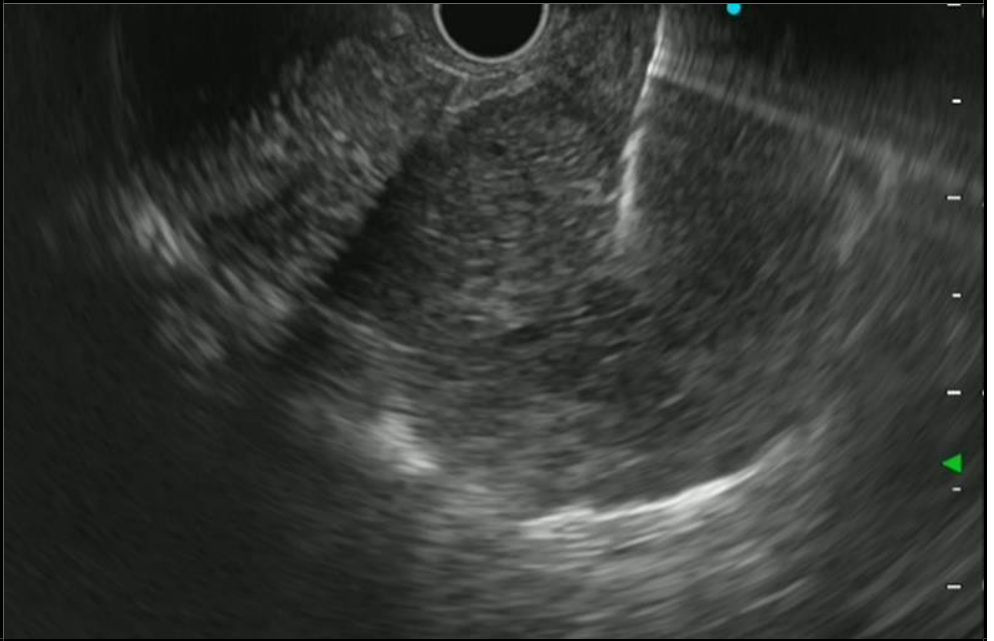
Figure 3: Endoscopic echo image
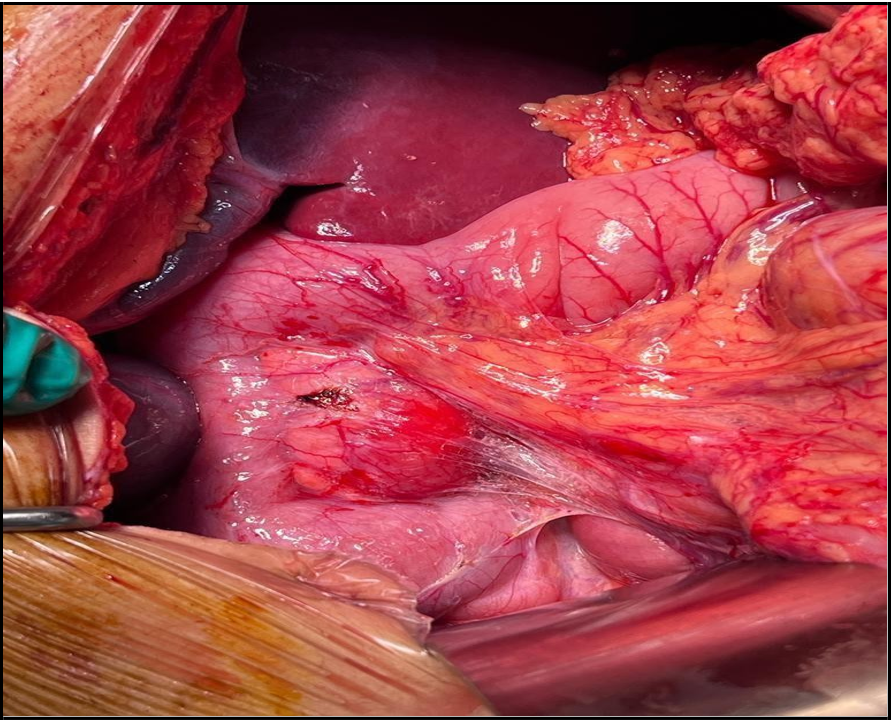
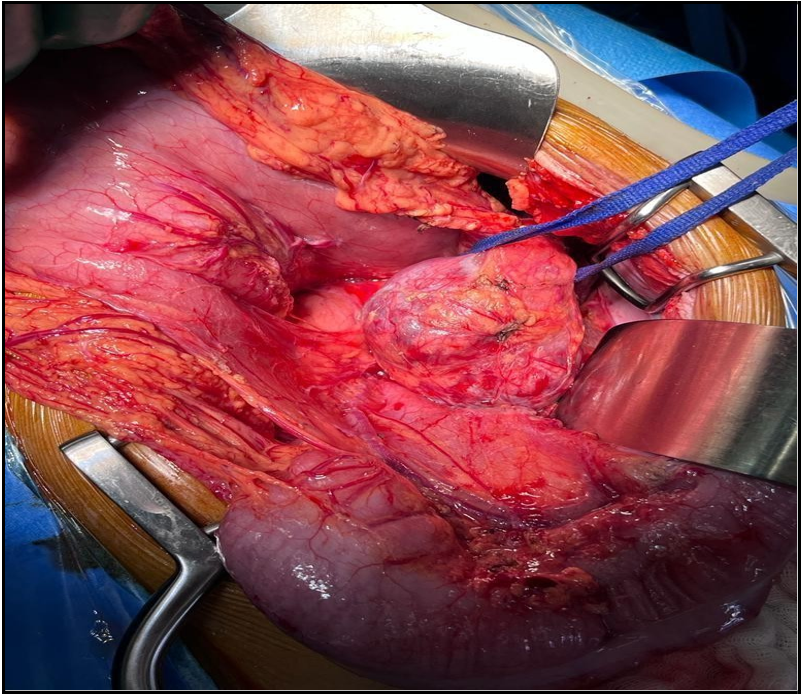
Figure 4a: Intraoperative image of the cephalic lesion of the pancreas
Figure 4b: Intraoperative image of pancreatic caudal lesion
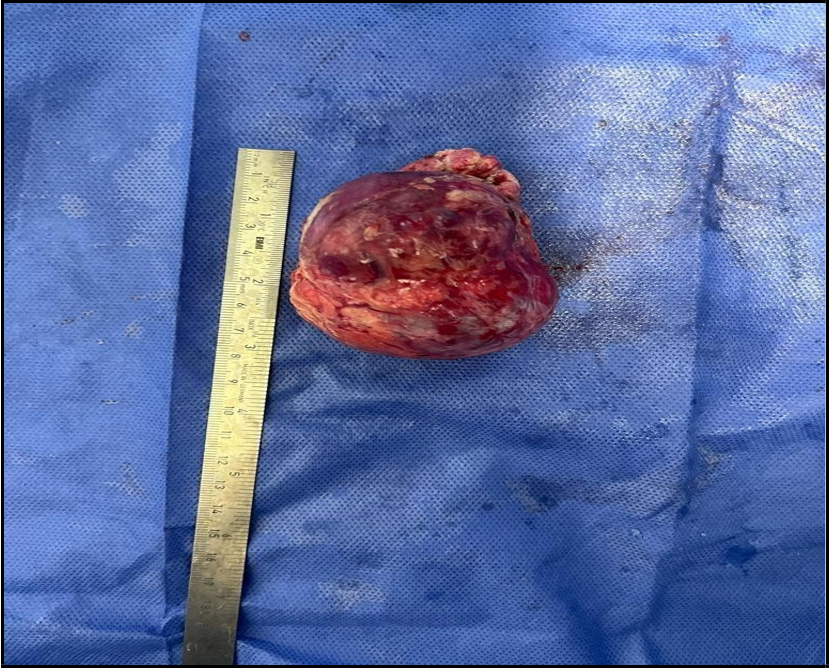
Figure 4c: Operative specimen of the DPC
Figure 4d: Operative specimen of caudal pancreatectomy
Endoscopic ultrasound with biopsy showed:
A well-limited 27 mm nodular lesion at the level of the head of the pancreas, heterogeneous, isoechoic to the pancreas, with mixed content (tissue and fluid), with posterior reinforcement, without vascular invasion or compression of the VBP or Wirsung's duct. No intra-lesional calcifications. A large 56 mm lesion at the corporeo- caudal junction, with similar characteristics to the cephalic lesion (Figure 3).
The histopathological study with immunohistochemistry confirmed pancreatoblastoma. Following a multidisciplinary consultation meeting, the decision was made to operate on the patient. She underwent a cephalic duodenopancreatectomy and a caudal pancreatectomy in the operating room (Figure 4: a; b; c; d). The postoperative follow-up was simple, with a follow-up in consultation and a follow-up of 8 months without any complications.
The patient's file was discussed at the multidisciplinary consultation meeting, where the post-operative monitoring decision was adopted.
Discussion
Pancreatoblastoma (BP) is a rare epithelial tumor of the pancreas, typically accounting for less than 0.5% of exocrine pancreatic tumors [4]. Originally described by Becker in 1957 as a tumor of the infantile pancreas, the term "pancreatoblastoma" was coined by Horie et al in 1977 [1,5].
MUAC has a bimodal age distribution, with modal peaks at 2.5 years and 40 years, and affects both sexes equally (male-to-female ratio, 1:1) [4,6]. Although the majority of cases are sporadic, some are associated with inherited syndromes such as Beckwith-Wiedemann syndrome and familial adenomatous polyposis [7].
Symptoms of BP are usually vague and nonspecific [3, 8, 9, 10]. Adult patients often present with abdominal pain, palpable mass, weight loss, and anorexia. In cases where the tumor is in the head of the pancreas, biliary obstruction and jaundice may occur, and symptoms of endocrine abnormalities may also be present [11].
A review of the literature indicates that the head of the pancreas is the most common tumor site, observed in 20 of the 38 patients studied (53%), followed by the tail, body and ampulla of Vater. In our case, a double localization of the MUAC, never described before, is observed [12].
Distant metastases most often occur in the liver, diagnosed in 25% of cases during the initial work-up [13, 9, 10]. However, bone, lung, peritoneal, cerebral and mediastinal metastases have also been reported [13,14].
In children with BP, high levels of AFP and CEA are common, while in adults, these tumor markers are usually within normal limits [1, 4]. Serum AFP levels can be used to monitor clinical response to treatment or recurrence in patients whose tumors produce it [8].
Accurate preoperative diagnosis of BP can be difficult due to non- specific radiographic features. The majority of BP tumors are well- defined, large and heterogeneous on transverse imaging, with a mixed solidocystic appearance. The differential diagnosis includes several other benign and malignant pancreatic conditions [4,7].
Macroscopically, the BP lesions are usually large, partially encapsulated, grayish or beige in color, and have areas of focal necrosis. Immunohistochemistry may be useful in characterizing different components of the tumor [4].
Although the optimal treatment strategy is not standardized due to the rarity of MUC, surgical resection remains the primary treatment strategy in adults [4,9]. Treatment outcomes, including overall survival, vary, and the role of adjuvant chemotherapy and radiotherapy remains controversial due to the limited number of patients treated to date.
Conclusion
Pancreatoblastoma with a double location is rare and little studied, surgery remains the only curative treatment. The effects of chemotherapy and radiotherapy have not been adequately studied due to the limited number of cases.
Conflict of interest: All authors declaring no ties of interest
References
- Becker WF (1957) Pancreatoduodenectomy for pancreatic carcinoma in an infant; case report. Ann Surg. 145(6): 864-870; Discussion, 870-872.
- Argon A, Celik A, Onız H, Ozok G, Barbet FY (2014) Pancreatoblastoma, a rare tumor in children: about a case. Turk Patoloji Derg 11: 15.
- Omiyale AO (2021) Adult pancreatoblastoma: Current concepts in pathology. World J Gastroenterol. 27(26): 4172-4181.
- Salman B, Brat G, Yoon YS, Hruban RH, Singhi AD, et al. (2013) The diagnosis and surgical treatment of pancreatoblastoma in adults: a case series and a review of the literature. J Gastrointest Surg. 17(12): 2153-2161.
- Horie A, Yano Y, Kotoo Y, Miwa A (1977) Morphogenesis of pancreatoblastoma, an infantile carcinoma of the pancreas: about two cases. Cancer. 39(1): 247-254.
- Gringeri E, Polacco M, D'Amico FE, Bassi D, Boetto R, et al. (2012) Liver autotransplantation for the treatment of unresectable hepatic metastasis: an uncommon indication-a case report. Transplantation Proceedings. 44(7) : 1930-1933.
- Hammer ST, Owens SR (2013) Pancreatoblastoma: a rare adult pancreatic tumor with multiple faces. Arch Pathol Lab Med. 137(9): 1224-1226.
- Du E, Katz M, Weidner N, Yoder S, Moossa AR, et al. (2003) Ampullary pancreatoblastoma in an elderly patient: a case review and a review of the literature. Arch Pathol Lab Med. 127(11): 1501 1505.
- Cavallini A, Falconi M, Bortesi L, Crippa S, Barughola G, et al. (2009) Pancreatoblastoma in adults: a review of the literature. Pancreatology. 9: 73-80.
- Balasundaram C, Luthra M, Chavalitdhamrong D, Chow J, Khan H, et al. (2012) Pancreatoblastoma: A rare tumor still evolving in its clinical presentation and histology. OJ. 13(3): 301-303.
- Abraham SC, Wu TT, Klimstra DS, Finn LS, Lee JH, et al. (2001) Distinctive molecular genetic alterations in pancreatoblastomas associated with sporadic and familial adenomatous polyposis: frequent alterations in the APC/betacatenin pathway and chromosome 11p. Am J Pathol. 159(5): 1619-1627.
- Zouros E, Manatakis DK, Delis SG, Agalianos C, Triantopoulou C, et al. (2015) Adult Pancreatoblastoma: A Case Report and Literature Review Oncol Lett. 9(5): 2293–2298.
- Rosebrook JL, Glickman JN, Mortele KJ (2005) Pancreatoblastoma in an adult female: ultrasound, CT scan, and gadolinium-enhanced MRI features. AJR Am JRoentgenol. 184(Suppl): S78-S81.
- Charlton-Ouw KM, Kaiser CL, Tong GX, Allendorf JD, Chabot JA (2008) Revisiting metastatic pancreatoblastoma in adults. A case study and a review of the literature. OGP. 9(6): 733 738.
- Montemarano H, Lonergan GJ, Bulas DI, Selby DM (2000) Pancreatoblastoma: imaging results in 10 patients and literature review. Radiology. 214(2): 476482.
- Comper F, Antonello D, Beghelli S, Gobbo S, Montagna L, et al. (2009) Expression pattern of claudins 5 and 7 distinguishes between solid pseudopapillaries of pancreatoblastoma, acinar cells and endocrine tumors of the pancreas. Am J Surg Pathol. 33(5): 768 774.