Adriaan Louw, PT, PhD1*, Jason Soncrant, DPT, SCS, FAAOMPT2, Terry Cox PT, DPT, OCS, FAAOMPT3
1Evidence in Motion, 618 Broad Street, Suite B, Story City, IA 50248
2South College Knoxville Campus, 400 Goodys Lane, Knoxville, TN 37922
3Southwest Baptist University, Davis Physical Therapy Building, 1600 University Ave, Bolivar, MO 65613
*Corresponding Author: Adriaan Louw, PT, PhD, Evidence in Motion, 618 Broad Street, Suite B, Story City, IA 50248.
Abstract
Background: Pain neuroscience education (PNE) is gaining clinical popularity and increasing evidence of its ability to yield positive clinical outcomes. Delivery methods for PNE are constantly expanding, and to date, it has never been explored if PNE can be successfully delivered via sign language.
Objective: To determine if PNE delivered via sign language can positively influence pain knowledge, fear-avoidance of physical activity, and beliefs regarding pain.
Design: Case series with pre- and immediate post-intervention measurements.
Methods: A convenience sample of adults proficient in sign language attended a community educational session featuring a 30-minute, 32-slide PNE PowerPoint™ presentation via sign language. Before and immediately after PNE, pain knowledge, fear of physical activity, and a series of pain beliefs (Likert scale) were assessed.
Results: Seven participants (4 females), with a mean age of 70.6 years, attended the session. Five participants were completely deaf, and the mean comfort level with sign language (0 = not at all; 10 = very comfortable) was 8. Immediately following PNE, pain knowledge improved by 28.5 % (p = 0.003). Fear avoidance improved but failed to reach significance (p = 0.41). All pain beliefs improved after PNE, but only one (Your brain decides if you feel pain, not your tissues) reached significance (p = 0.012).
Conclusion: PNE delivered via sign language can significantly improve pain knowledge in older adults. Future studies, including clinical trials on patients presenting with pain, should be explored to see if these results can be replicated in patient populations and lead to clinical benefits associated with pain relief and decreased disability.
Keywords:
- Pain neuroscience education
- Sign-language
- Deaf
- Pain knowledge
- Social determinants of health
Introduction
In physical therapy, pain neuroscience education (PNE) is emerging as an evidence-based, biopsychosocial approach to treating pain, especially with movement-based treatment such as exercise [1-3]. Strong evidence shows that PNE can positively influence self-reported pain ratings, disability, fear avoidance, pain catastrophizing, limited movement, and healthcare utilization [3,4]. Most data pertains to chronic pain, with PNE now part of the current practice guidelines for chronic low back pain [5]. Emerging research also points to PNE as potentially beneficial in those with acute and sub-acute pain, especially when high fear avoidance and pain catastrophizing are present [6].
PNE uses metaphors, examples, and images to teach patients more about the underlying biology and physiology of their pain experiences [7]. Modern pain science focuses on central and peripheral sensitization of the nervous system, functional and structural changes in the brain amid a pain experience, and endogenous mechanisms to influence a pain experience via inhibition and facilitation. It is conveyed to patients in easy-to-understand concepts, metaphors, and stories [8]. It is proposed that by learning more about these neuroscience processes, patients reconceptualize their pain experience, decrease fear and catastrophizing, move more, and adopt healthier beliefs about pain [9]. This newfound understanding of pain directly contrasts prevailing biomedical models that tie a person's tissue health to their pain experience [10]. A growing body of literature shows the limited correlation between tissue health and a human's pain experience, especially chronic pain [8,10,11]. To date, PNE has been applied to a variety of different chronic pain conditions and various clinical settings and has been successfully used in children, adults, and older adults [4,12,13]. It is effective even in adults with mild traumatic brain injury [14].
At the heart of PNE is the ability of a patient to learn the new concepts of pain science. Current education delivery methods include one-on-one verbal education, group therapy, and telehealth [4]. Recent evidence shows that one-on-one, therapist-led PNE is superior to group PNE regarding outcomes, while group PNE yields potentially significant cost-savings [4]. As PNE expands, barriers are also encountered. For example, PNE, to fully impact the global pain epidemic, must reach beyond language, culture, geography, etc. In clinical practice, clinicians often encounter patients who need to be more fluent in English, and PNE must be relayed to patients via interpreters, be it legal services or via family. One barrier includes patients who are deaf and require sign language and lip-reading to communicate, including receiving healthcare information. In the United States, it's currently estimated that 10 million Americans are hard of hearing, while at least 1 million are classified as functionally deaf [15]. In this scenario, if a deaf patient experiences chronic pain, how can PNE be delivered? To date, no study has explored if PNE provided by sign language yields comparable outcomes to one-on-one verbal educational sessions led by a physical therapist. This study aims to deliver PNE to a sample of deaf participants to determine if PNE via sign language can yield similar results to verbal one-on-one or vocal group PNE.
Methods
Study
Before the study, institutional review board approval was obtained at Southwest Baptist University. Participants were asked to provide written consent for participation in the study, and the study followed the Helsinki Declaration of Ethics for medical research. The study was a case series with pre- and immediate post-intervention measures with no personally identifiable information collected.
Participants
To deliver PNE to a cohort of deaf participants, a healthcare provider familiar with PNE and fluent in sign language was recruited. The largest post-professional organization in the United States teaching physical therapists (evidenceinmotion.com) was asked to notify their post-professional educator's database to see if they met the requirements (n = 239). Inclusion criteria were in line with previous PNE studies delineating a minimum requirement to be proficient with PNE, including having attended 15 hours of post-professional education in PNE, scoring >80 % on the neurophysiology of pain questionnaire (NPQ), and using PNE regularly in clinical practice [16]. Additionally, the clinician had to be fluent in sign language and use it regularly. Two therapists replied to the request, both meeting the minimum PNE requirements. One therapist has been trained in sign language but does not use it regularly, while the second therapist (JS) is fluent and uses it regularly since his mother is deaf.
In line with the study's aim, participants had to be formally diagnosed as being deaf and use sign language (with or without lip reading) as a primary method of communication. Previous PNE studies have been done on patients (individuals seeking care for treatment) and community members interested in learning more about pain but have yet to seek care [3,17] actively. Therapist JS's mother is deaf and, due to her disability, has developed a community of older adults that meet regularly for social interaction as part of a church group and use sign language for communication. These meetings are in-person. The social group members were asked to participate in the study, including completing pre- and post-PNE surveys. Participation in the study was entirely voluntary, and participants were provided a gift card each for their time to complete the pre-and post-PNE questionnaires. The goal of the pilot study was to recruit 6-8 participants.
Educational Content
Previous studies have described the PNE content for this presentation in detail [12,13]. The lecture was an abbreviated 30-minute, 32-slide PNE PowerPoint™ presentation used in previous studies, allowing ample time for survey completion before and following the PNE lecture. The presentation's main themes include a discussion of peripheral sensitization, central sensitization, bio-psycho-social factors associated with pain, threat appraisal of the brain, nociception, stress, and endocrine responses in pain various therapeutic endogenous strategies to ease pain [12,18]. Multiple images, metaphors, and examples convey the PNE to the participants [7]. Following the formal presentation and completion of the post-PNE surveys, participants were encouraged to ask questions. The production did not specifically address or target any questions in the outcome measures.
Outcomes
Participants agreeing to be part of the study were asked to complete a demographic survey to describe the cohort of participants, but no personally identifiable information was gathered. Demographic data included age, gender, years being deaf, information about pain (if any) – present, if so, a pain rating using a Numeric Pain Rating Scale (NPRS), location and specific pain diagnoses; occupation, the highest level of education, income level, frequency and comfort using sign language. Four formal outcome measures were used for the participants to assess changes associated with PNE:
- Pain Knowledge: Pain knowledge was measured using the revised neurophysiology of pain questionnaire (NPQ). The NPQ is based on a current pain science text [19] and was used in a previous study measuring the neurophysiology knowledge of patients and healthcare personnel [20]. The original NPQ is a 19-item questionnaire requesting 'true'; 'false'; or 'not sure' answers to statements, with higher scores indicating more correct answers. Since the developmentof the NPQ, a statistical analysis of the NPQ has led to the development of an abbreviated NPQ with 12 questions, which removed ambiguous questions [21]. The revised 12-question NPQ was used in this study. The questionnaire was adapted similarly to previous studies to make it easier for non-medically trained people to understand, e.g., "nociception" was replaced with "danger messages" [20]. No data on patients or healthy controls are available on what constitutes a meaningful shift. Adult and older-adult studies (ages 18 and above) have shown NPQ mean improvements after a PNE session to typically range between 25-30 % [11, 22, 23].
- Fear Avoidance Beliefs of Physical Activity (Fear Avoidance Beliefs Questionnaire - FABQ): The FABQ is a 16-item questionnaire designed to quantify fear and avoidance beliefs in individuals with low back pain. The FABQ has two subscales: 1) a 4-item scale to measure fear-avoidance beliefs about physical activity and 2) a 7-item scale to measure fear-avoidance beliefs about work. Each item is scored from 0 to 6, with possible scores ranging between 0 and 24 and 0 and 42 for the physical activity and work subscales, respectively, with higher scores representing increased fear-avoidance beliefs. To accurately measure the fear of physical activity (PA), the FABQ-PA scale was used in this study. Since the survey intended to ascertain fear of PA in the presence of pain, the wording was altered to ask about PA if/when they have pain versus currently experiencing pain. This has been done in previous PNE studies [13,24]. The FABQ has demonstrated acceptable levels of reliability and validity in previous studies [25-27]. The presence of avoidance behavior is associated with an increased risk of prolonged disability and work loss. It is proposed that FABQ-PA >14 is associated with a higher likelihood of not returning to work or activities of daily living [28,29].
- Pain rating (NPRS): The study's intention was not to precisely determine the efficacy of PNE for patients that are deaf and experiencing pain. NPRS was included before and after the PNE intervention due to higher rates of pain prevalent in older adults. The NPRS is often used in studies for chronic pain [30-33]. The minimal clinically significant difference (MCID) for the NPRS for acute/sub- acute pain is reported to be 2.0 [34], and for chronic musculoskeletal pain, 1.0 [35].
- Pain Beliefs: The healthcare provider's attitudes and beliefs regarding chronic pain are often measured with the Health Care Provider's Pain and Impairment Relationship Scale (HC-PAIRS) [36]. This scale is typically not used for non-medically trained people but has recently been used in middle school children's PNE studies [13,24]. Upon review of the HC-PAIRS and the aims of the study, a series of numeric rating scale questions pertaining to beliefs about pain was established by the authors for this study and used in previous studies. The numeric rating scale was anchored between 0 (strongly disagree) and 10 (strongly agree). Five questions were established to allow surveys to be completed before and following the PNE session in the allotted time. Beliefs statements were:
- Pain is normal; without being able to feel pain, you will not survive.
- Pain means something is wrong with your tissues.
- Pain always means you must stop what you are doing.
- You can control how much pain you feel.
- Your brain decides if you feel pain, not your tissues.
Statistical Analysis
Upon completion of the study, participant intake forms from pre and post-treatment were collected for analysis. There was no attrition during the study, and all participants were accounted for in the post-treatment analysis. Summary statistics were generated in tables to understand the study sample's demographics better. A series of Student paired, one-sample t-tests with df = 6 were used to test for significant differences in Pain Knowledge, Fear-Avoidance, and Pain Beliefs. Due to the benchmarking nature of this study, it should be noted that the sample size leaves the research and the following results underpowered but merits further investigation of any possible phenomena on a larger sample and using more robust analysis techniques.
Results
Seven community members fluid in sign-language attended the PNE session and completed the pre- and post PNE measures (Table 1).
Table 1: Study participants
|
|
Patients (n = 7) |
|
Mean age (years) |
70.6 (range 57.8 – 83.3) |
|
Female (%) |
4 (57.1) |
|
White Non-Hispanic (%) |
7 (100 %) |
|
Educational background: - Graduate (%) - Postgraduate (%) - High School (%) |
3 (42.8) 2 (28.6) 2 (28.6) |
|
Annual income - $50k - $100k (%) - < $10k (%) - $10k - $50k (%) |
4 (57.1) 2 (28.6) 1 (14.3) |
|
Completely deaf (%) - Mean duration of being completely deaf (years) |
5 (71.4) 59.84 |
|
Mean comfort with sign language (0 = not at all; 10 = very comfortable) |
8 |
|
Currently experiencing pain (%) - Mean pain score |
6 (85.7) 3.6 |
|
Experiencing any long-lasting pain (> 6 months) (%) |
2 (28.6) |
Pain knowledge
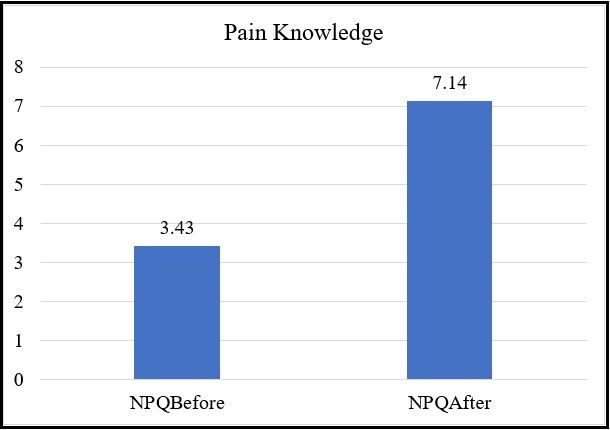
Prior to the PNE lecture, the mean NPQ score was 3.43 (26.4% accuracy). Immediately following the lecture, the mean PNE score increased by 28.5 % (7.14) (p = 0.003) (Figure 1).
Figure 1: NPQ scores before and after PNE via sign language
Fear-Avoidance
Prior to PNE, the mean FABQ-PA score was 12.14, with two participants (28.6%) exceeding the cut-off for a high FABQ-score (> 15). Immediately after PNE, the mean FABQ-score decreased to 9 (p = 0.41), and all participants scoring below the cut-off for a high FABQ-PA score.
Pain Beliefs
Only one pain belief (Your brain decides is you feel pain, not your tissues) shifted significantly after sign-language-delivered PNE (p = 0.012) (Table 2).
Table 2: Pain beliefs before and after PNE
|
Statement |
Before PNE |
After PNE |
Significance |
|
Pain is normal; without being able to feel pain, you will not survive |
6.43 |
4.71 |
0.418 |
|
Pain means something is wrong with your tissues |
7.57 |
5.14 |
0.125 |
|
Pain always means you have to stop what you are doing |
5 |
4.14 |
0.29 |
|
You can control how much pain you feel |
7.29 |
8.57 |
0.163 |
|
Your brain decides if you feel pain, not your tissues |
6 |
8.86 |
0.012* |
(* indicates significant difference P < 0.05)
Discussion
The results of this study show that PNE can be successfully delivered via sign language and is effective in improving pain knowledge, fear avoidance, and various beliefs regarding pain. This is the first study exploring using sign language to deliver PNE.
PNE is best delivered using metaphors, examples, and pictures [4]. PNE delivery, to date, has used various senses to help in the process of learning more about pain. In verbal education (one-on-one, group, or telehealth) [4,11,37,38], auditory and visual reception is vital for patients and clinicians to learn more about the neuroscience of pain. In other studies, patients have been tasked with reading PNE content to enhance pain beliefs and knowledge [39,40]. A growing body of evidence shows that PNE increases pain knowledge in various patient diagnoses, clinical conditions, and age groups but assumes senses to be optimal. In this study, albeit a small sample, it was shown that pain knowledge improved by 28 %, which is at the upper end of the enhanced pain knowledge spectrum seen in adult and older-adult studies (ages 18 and above), which typically range between 25-30 % [11,22,23]. The results indicate that PNE can be successfully delivered via sign language in a cohort of adults proficient in sign language and deaf. To further put these results in perspective, the 28 % improvement in this cohort of older adults (mean age 70.6 years) is far superior to other PNE studies in older adults where PNE was delivered verbally, including Watson et al. [12] (11 %) and Alnwick et al. (submitted for publication – 2023) (16 %).
In this study, FABQ-PA did shift positively but not significantly. This result concurs with the study by Watson et al., who conducted a community center delivery of PNE to older adults [12]. It can be argued that this may be because the FABQ-PA was not designed for this purpose – asking people to report their fear of physical activity “in the presence of pain” versus being in pain and facing impending physical activity, i.e., physical therapy, work or leisure activities [28]. Another factor to consider is that the study did not target people presenting with high FABQ-PA scores. In this study, only two participants displayed FABQ-PA scores exceeding the cut-off score for a high FABQ [28]. The results of this study may indicate that a clinician delivering PNE via sign language to a patient displaying high levels of fear avoidance may obtain clinical benefit from such an approach and allows much-needed pain education for deaf patients attending rehabilitation.
Regarding pain beliefs, all beliefs shifted positively, with only one being significant (“Your brain decides if you feel pain, not your tissues” - p = 0.012). This result is in line with other PNE studies showing positive shifts in beliefs [4,12], albeit various studies show different opinions being altered with no consistent views being shifted. This warrants future studies to determine which ideas are more easily targeted with PNE versus others.
This study contains various limitations. First, the case series design is commonly used in exploratory analyses, but the results are limited given that there is no control group to compare the interventional group to. Second, this is not a patient sample, but rather adults meeting inclusion criteria willing to sign up for the study, making its application to patients presenting with pain hypothetical. Third, the outcomes were only measured immediately following intervention with no intermediate or long-term follow-up, which is needed to determine the true efficacy of the intervention. Finally, the outcome measures chosen were based on a previous community older-adult PNE study to determine if similar results can be obtained with sign language. Given the unique challenges of being deaf, and the ability to learn PNE, it can be argued that better outcome tools could have been explicitly used to assess comprehension of the content delivered.
Conclusion
PNE delivered via sign language can significantly improve pain knowledge in older adults. Future studies, including clinical trials on patients presenting with pain, should be explored to see if these results can be replicated in patient populations and lead to clinical benefits associated with pain relief and decreased disability.
References
- Louw A, Puentedura EJ, Denninger TR, Lutz AD, Cox T, et al. (2022) The clinical impact of pain neuroscience continuing education on physical therapy outcomes for patients with low back and neck pain. PLoS One. 17(4):e0267157.
- Louw A, Sluka KA, Nijs J, Courtney CA, Zimney K (2021) Revisiting the Provision of Pain Neuroscience Education: An Adjunct Intervention for Patients but a Primary Focus of Clinician Education. J Orthop Sports Phys Ther. 51(2): 57-59.
- Watson JA, Ryan CG, Cooper L, Ellington D, Whittle R, et al. (2019) Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J Pain. 20(10): 1140.e1-1140.e22.
- Louw A, Zimney K, Puentedura EJ, Diener I (2016) The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiotherapy Theory and Practice. 32(5): 332-355.
- George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, et al. (2021) Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther. 51(11): CPG1-CPG60.
- Louw A, Farrell K, Choffin B, Foster B, Lunde G, et al. (2019) Immediate effect of pain neuroscience education for recent onset low back pain: an exploratory single arm trial. J Man Manip Ther. 27(5): 267-276.
- Louw A, Zimney K, O'Hotto C, Hilton S (2016) The clinical application of teaching people about pain. Physiotherapy Theory and Practice. 32(5): 385-95.
- Moseley GL (2007) Reconceptualising pain acording to modern pain sciences. Physical Therapy Reviews. 12: 169-178.
- Malfliet A, Kregel J, Coppieters I, De Pauw R, Meeus M, et al. (2018) Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA Neurol. 75(7): 808- 817.
- Nijs J, Roussel N, Paul van Wilgen C, Köke A, Smeets R (2013) Thinking beyond muscles and joints: therapists' and patients' attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther. 18(2): 96-102.
- Moseley L (2003) Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. 4(4): 184-189.
- Watson S, Louw A, Wingood M, Rico D, Podolak D, et al. (2021) Pain Neuroscience Education for Older Adults. Physical & Occupational Therapy In Geriatrics. 40(1): 50-63.
- Louw A, Landrus R, Podolak J, Benz P, DeLorenzo J, et al. (2020) Behavior Change Following Pain Neuroscience Education in Middle Schools: A Public Health Trial. Int J Environ Res Public Health. 17(12): 4505.
- Benedict TM, Nitz AJ, Abt JP, Louw A (2021) Development of a pain neuroscience education program for post-traumatic stress disorder and pain. Physiother Theory Pract. 37(4): 473-485.
- Mitchell RE (2006) How many deaf people are there in the United States? Estimates from the Survey of Income and Program Participation. J Deaf Stud Deaf Educ. 11(1): 112-9.
- Louw A, Diener I, Landers MR, Puentedura EJ (2014) Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1- year follow-up. Spine. 39(18): 1449-57.
- Louw A, Zimney K, Puentedura EL (2016) Retention of pain neuroscience knowledge: a multi-centre trial. New Zealand Journal of Physiotherapy. 44(2): 91-96.
- Moseley GL, Nicholas MK, Hodges PW (2004) A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clinical Journal of Pain. 20(5): 324-330.
- Wall, P.D, Melzack R (2005) Textbook of Pain. 5th edn ed. London. Elsevier.
- Moseley L (2003) Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. Journal of Pain. 4(4): 184-189.
- Catley MJ, O'Connell NE, Moseley GL (2013) How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. The Journal of Pain. 14(8): 818-27.
- Meeus M, Nijs J, Van Oosterwijck J, Van Alsenoy V, Truijen S (2010) Pain Physiology Education Improves Pain Beliefs in Patients With Chronic Fatigue Syndrome Compared With Pacing and Self-Management Education: A Double-Blind Randomized Controlled Trial. Arch Phys Med Rehabil. 91(8): 1153-1159.
- Van Oosterwijck J, Meeus M, Paul L, De Schryver M, Pascal A, et al. (2013) Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia: a double-blind randomized controlled trial. The Clinical journal of pain. 29(10): 873-82.
- Louw A, Podolak J (2019) A Randomized controlled trial of different single pain education sessions in middle school students: Immediate effects. Journal of the Physiotherapy Pain Association. 2019(47): 14-24.
- Cleland JA, Fritz JM, Childs JD (2008) Childs, Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Am J Phys Med Rehabil. 87(2): 109-17.
- Grotle M, Vøllestad NK, Brox JI (2006) Clinical course and impact of fear-avoidance beliefs in low back pain: prospective cohort study of acute and chronic low back pain: II. Spine. 31(9): 1038-46.
- Poiraudeau S, Rannou F, Baron G, Henanff LA, Coudeyre E, et al. (2006) Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 124(3): 305-11.
- Fritz JM, George SZ (2002) Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 82(10): 973-83.
- Burton AK, Waddell G, Tillotson KM, Summerton N (1999) Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 24(23): 2484-91.
- Moseley GL (2003) Joining forces - combining cognition- targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap. 11(2): 88-94.
- Moseley L (2002) Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 48(4): 297-302.
- Moseley GL (2005) Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 51(1): 49-52.
- Cleland JA, Childs JD, Whitman JM (2008) Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 89(1): 69-74.
- Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 30(11): 1331-4.
- Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W (2004) Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 8(4): 283-91.
- Latimer J, Maher C, Refshauge K (2004) The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain. 20(1): 45-50.
- Louw A, Vogsland R, Marth L, Marshall P, Cox T, et al. (2019) Interdisciplinary Pain Neuroscience Continuing Education in the Veteran's Affairs: Live Training and Live-Stream with 1-year Follow-up. Clin J Pain. 35(11): 901-907.
- Zimney K, Louw A, Puentedura EJ (2014) Use of Therapeutic Neuroscience Education to address psychosocial factors associated with acute low back pain: a case report. Physiotherapy theory and practice. 30(3): 202-9.
- Rufa A, Beissner K, Dolphin M (2018) The use of pain neuroscience education in older adults with chronic back and/or lower extremity pain. Physiotherapy theory and practice. 35(7): 603-613.
- Gallagher L, McAuley J, Moseley GL (2013) A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. The Clinical journal of pain. 29(1): 20-5.