Hind Jamal Al-Dabal1,2, Monira AI Zahrani1,2, Hayat Ahmed AI Rabiah1,2, Lubna khan1*
1Department of obstetrics and Gynecology King Abdul Aziz Medical city Riyadh KSA
2IVF and Reproductive medicine, KAMC, Riyadh
*Corresponding Author: Lubna khan, Department of obstetrics and Gynecology King Abdul Aziz Medical city Riyadh KSA.
Abstract
Fertility management including Assisted Reproductive Technology is a well-recognized risk factor for Ectopic pregnancy. Ovarian pregnancy is a very rare complication of both spontaneous and ART-induced pregnancies. The incidence of spontaneous primary ovarian pregnancy ranges from 1:7000 to 1:40,000 pregnancies accounting for 0.5 % - 3.6 % of all ectopic pregnancies [1,2]. General risk factors of ovarian ectopic pregnancy are tubal pathology, previous gynecologic surgery, pelvic inflammatory diseases, and Intrauterine contraceptive device use. Laparoscopic management with resection of ovarian pregnancy while preserving ovarian tissue is considered the gold standard treatment; however, successful medical management with methotrexate has been reported14
Keywords: ovarian ectopic, infertility treatment, Methotrexate vs laparoscopy
Case Report
A 31 years old lady, known to have Primary male factor infertility for 18 years. The couple had multiple cycles of ICSI/ IVF with no resultant pregnancy.
She was not having any medical or surgical history, but she had a BMI of 37(obesity class ii).
she did not have any previous history of PID, Tubal Surgery, and Ovarian Surgery.
Her Day 3 FSH level was 4.76 IU, Estradiol Level was 101pmol/L, LH level was 4.21
IU and the rest of the basic workup were within normal limits. Hysterosalpingogram showed normal endometrium, uterine cavity, and bilateral patent fallopian tubes.
Ultrasonography reveals a normal antral follicle count of 10. Each ovary had ten follicles with an endometrial thickness of 3.4 mm and no other pathology was identified.
Patient had an ICSI cycle with frozen sperm which was started on the 3rd day of the cycle with Gonadotrophin hormone-releasing hormone antagonist Protocol using recombinant FSH of 225 IU daily, Cetrotide 0.25 mg was started on day 5th of stimulation. Treatment continued till the 8th day of stimulation till the Estradiol Level reach 13135pmol/L and at that time a decision was made to reduce the dose of r-FSH to 100 iu. The cycle continues with the reduced dosage till the day of induction when the Estradiol level was 22856 pmol/L and where the ovulation triggering is done with GnRh Agonist (0.2 mg Decapepetyl) because of the risk of ovarian Hyper-stimulation syndrome.
27 eggs were retrieved, 21 were injected with sperm, and out of them three were fertilized with intra-cytoplasmic sperm injection; 2 grade one blastocysts developed (4 cell stage) which were transferred intrauterine on day 5. Progesterone support is used for the luteal phase.
The trend of Bhcg level was as follows:
- 5/1/2020 = 11.4, 7/1/2020 = 35.4, 14/1/20 = 611.4, 16/1/20 = 1029,19/1/20 = 1841
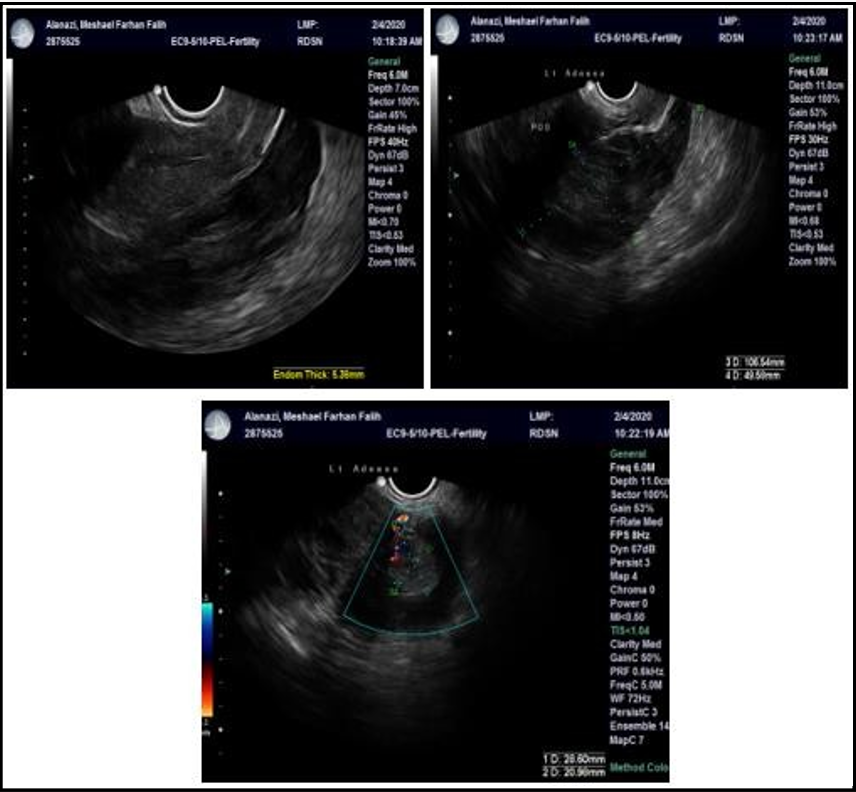
On Ultrasound there was no IUP and a heterogeneous mass was seen above the left ovary which measured 13.3 x11.2x11.4 mm with positive blood flow consistent with ovarian ectopic pregnancy. The patient was counseled regarding the risk and benefit of medical v/s surgical management and a joint decision was made to give methotrexate. Upon follow up there was a suboptimal drop-in on day 4 and day 7 Bhcg which went down from 2689.6 to 2559 IU/L respectively. At that time patient was given another dose of Methotrexate.
Later on, the patient presented with severe Lower abdominal pain, not associated with nausea or vomiting with stable vital signs. On ultrasonography in addition to the previous heterogeneous mass seen above the left ovary, there was heterogenous fluid collection seen in the Pouch of Douglas. Ruptured Ectopic was Suspected and the patient planned for Laparoscopy and informed consent was taken.
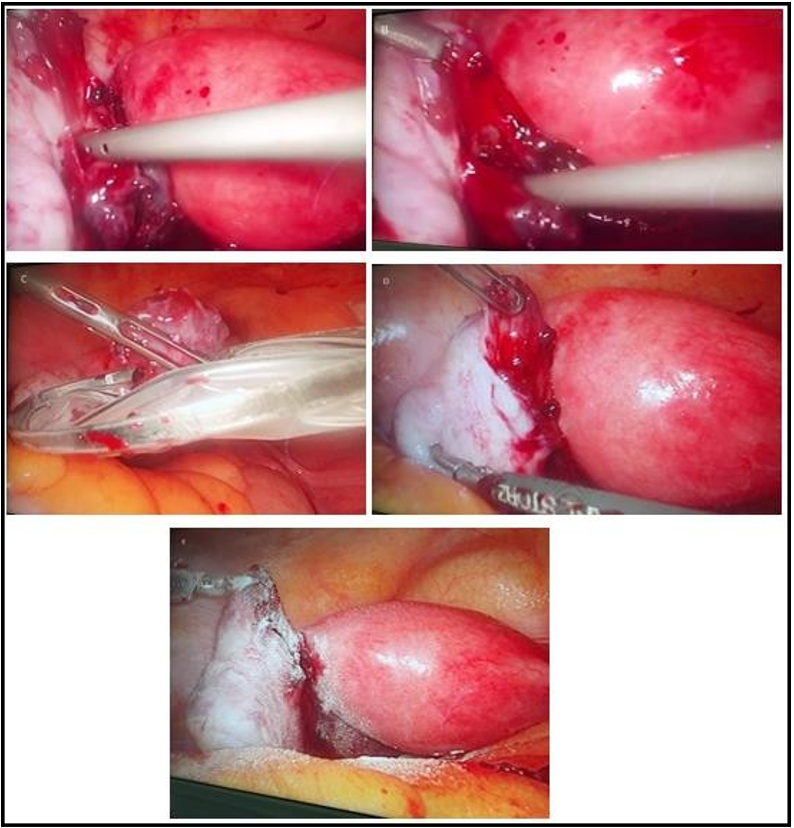
Intra Operatively Uterus was Grossly normal and blood & clots were filling the Pouch of Douglas and the lower part of the pelvis. Both tubes were identified and found normal. The right ovary was normal although the left ovary was seen with ruptured ectopic pregnancy. Ectopic pregnancy was removed with hydro dissection and traction- counter traction technique with ovarian tissue preservation. Hemostasis was secured.
Post-operative Bhcg dropped remarkably, and the patient had an uneventful recovery afterward. The histopathology report confirmed the diagnosis of ovarian ectopic pregnancy with Chorionic villi admixed with decidua and a minimal rim of ovarian stroma.
Patient was followed up in the clinic till her Bhcg level drop down to a non-pregnant value.
Ultrasound showing empty uterus with left adnexal mass with +ve blood flow before receiving the 1st dose of MTX.
Ultrasound showing left adnexal mass with +ve blood flow+ free fluid in POD after receiving the 2nd dose of MTX
Intra-operative finding:
Figure (A &B ): hydro-dissection of ovarian pregnancy
Figure (C) removing of ovarian ectopic using Endo-bag.
Figure (D) the ovary preserved after removing an ectopic pregnancy
Figure (E): hemostatic powder placed over the preserved ovary.
Discussion
Ovarian pregnancy is a rare variant of non-tubal ectopic pregnancy which can be either spontaneous or ART-induced. (1)
One study among IVF patients showed a higher frequency of ovarian pregnancy comprising 4.5 %–6 % of Ectopic pregnancies, However, there may be a detection bias since IVF pregnancies are usually monitored earlier and more carefully than natural pregnancies; and therefore, short-lived IVF-induced ovarian pregnancies have a higher likelihood of being detected.
The mechanisms behind ovarian pregnancy are not completely understood; however, can be classified as primary and secondary. In the primary, there is direct fertilization of a mature egg inside the ovary while in the secondary there is retrograde embryo migration back into the ovary via the fallopian tube. In in-vitro fertilization (IVF), the embryo will be transferred to the uterus under ultrasound guidance, therefore in our case ovarian pregnancy most likely occurs due to secondary retrograde embryo migration. [3,4,5]
Regarding the symptoms of Ovarian pregnancy, it is usually similar to tubal pregnancy symptoms like abdominal pain, vaginal bleeding, and delayed menses; however asymptomatic ovarian pregnancies have been described in the literature.[6]
The diagnostic criteria for ovarian pregnancy have been established by A german gynecologist. the criteria depend on the intraoperative findings:
- the gestational sac is in the same position as the ovary.
- the ovary is connected to the uterus by the utero-ovarian ligament.
- intact fallopian tube on the ipsilateral side.
- the ovarian tissue is present in the wall of the gestational sac. [7] General risk factors of ectopic ovarian pregnancy include tubal pathology, previous gynecologic surgery, pelvic inflammatory diseases, and IUD use.
Possibly the risks have been increased with IVF due to higher volume of the culture medium, higher pressure of injection into the uterus, ovarian surface scars from oocyte retrieval, high estrogen levels, progesterone levels, ovarian hyper vascularity after ovarian stimulation, a high number of transferred embryos, and transfer of blastocyst. [8,9]
Some study results showed more ectopic pregnancies among patients with peak serum estradiol concentration exceeding 4085 pg./mL (15,000 pmol/L)[10] A possible mechanism for the effect of high estradiol level is provided by the following observations: it affects the normal physiology of the fallopian tube including impaired protein secretion, ciliary motion frequency, embryonic motility, and implantation, which increased the likelihood of extrauterine implantation.
Oliveira et al 18 described a possible association between blastocyst transfer and intraovarian implantation, as they had no cases of ovarian pregnancies following the transfer of embryos on days 2nd and 3rd. [11]
By ultrasonography, the ovarian Ectopic Pregnancy mimics corpus luteum, hemorrhagic cyst, and endometriotic cyst of the ovary which delay the diagnosis of ovarian pregnancy, as serum βhCG level and imaging are of limited contribution to the diagnosis of ovarian pregnancy. The American Society for Reproductive Medicine recommends a surgical intervention in any case of suspected ovarian pregnancy, which may begin as explorative laparoscopy for suspected extra-uterine pregnancy.
If ovarian ectopic has been diagnosed the management may include salpingo-oophorectomy, oophorectomy, wedge resection, and removal of gestational product with ovarian tissue preservation.
Laparoscopic management with resection of ovarian gestation and preservation of ovarian tissue is considered the gold standard treatment; however medical management with methotrexate has been reported.[12]
the use of MTX to treat ovarian pregnancy is not as well established, unlike treatment with MTX for tubal pregnancy Mittal et al showed promising results with an intragestational sac MTX injection. [13]
Conclusion
Ovarian ectopic pregnancy poses an ethical and diagnostic dilemma because of the scarcity of clinical presentation and diagnosis. As most of the patients are presenting and diagnosed late, Methotrexate will not be a viable treatment option in most of these cases, therefore Surgical management and removal of the Ectopic is the gold standard modality where experts are available.
Ethical approval:
We obtained permission & a consent from the patients to publish this report with the pictures anonymously and ethical approval was granted by the Ethics Committee of the hospitals.
Conflict of interest: none declared
References
- Joseph RJ, Irvine LM (2012) Ovarian ectopic pregnancy: etiology, diagnosis, and challenges in surgical management. J Obstet Gynaecol. 32(5): 472–474.
- Marcus SF, Brinsden PR (1993) Primary ovarian pregnancy after in vitro fertilization and embryo transfer: report of seven cases. Fertil Steril. 60(1): 167–169.
- Boronow RC, Mcelin TW, West RH, Buckingham JC (1965) Ovarian pregnancy; report of four cases and a thirteen-year survey of the English literature. Am J Obstet Gynecol. 91: 1095–1106.
- Marcus SF, Brinsden PR (1995) Analysis of the incidence and risk factors associated with ectopic pregnancy following in-vitro fertilization and embryo transfer. Hum Reprod. 10(1): 199–203.
- Raziel A, Schachter M, Mordechai E, Friedler S, Panski M, et al. (2004) Ovarian pregnancy-a 12-year experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol. 114(1): 92–96.
- Andrade AG, Rocha S, Marques CO, Simões M, Martins I, et al. (2015) Ovarian ectopic pregnancy in adolescence. Clin Case Rep. 3(11): 912–915.
- Choi HJ, Im KS, Jung HJ, Lim KT, Mok JE, et al. (2011) Clinical analysis of ovarian pregnancy: a report of 49 cases. Eur J Obstet Gynecol Reprod Biol. 158(1): 87–89.
- Marcus SF, Brinsden PR (1993) Primary ovarian pregnancy after in vitro fertilization and embryo transfer: report of seven cases. Fertility and Sterility. 60(1): 167–169.
- Gavrilova-Jordan L, Tatpati L, Famuyide A (2006) Primary ovarian pregnancy after donor embryo transfer: early diagnosis and laparoscopic treatment. JSLS. 10(1): 70–73.
- Wang J, Wei Y, Diao F, Cui Y, Mao Y, et al. (2013) The association between polycystic ovary syndrome and ectopic pregnancy after in vitro fertilization and embryo transfer. Am J Obstet Gynecol. 209(2): 139.e1-9.
- Oliveira FG, Abdelmassih V, Costa AL, Balmaceda JP, Abdelmassih S, et al. (2001) Rare association of ovarian implantation site for patients with heterotopic and with primary ectopic pregnancies after ICSI and blastocyst transfer. Hum Reprod. 16(10): 2227–2229.
- Birge O, Erkan MM, Ozbey EG, Arslan D (2015) Medical management of an ovarian ectopic pregnancy: a case report. J Med Case Rep. 9(1): 290.
- Mittal S, Dadhwal V, Baurasi P (2003) Successful medical management of ovarian pregnancy. Int J Gynaecol Obstet. 80(3): 309-10.