Borys Pavlov*, Volodymyr Romanenko
Neurospine Clinic, Kyiv, Ukraine
*Corresponding Author: Borys Pavlov, Neurospine Clinic, Kyiv, Ukraine.
Abstract
Introduction: Intervertebral disc protrusion is often a cause of radicular and discogenic axial low back pain (LBP), even without compression of the nerve root by disc material. Both components of pain – discogenic axial and radicular - can often be present in a patient with LBP, and it is impossible to distinguish it only on a clinical and visual-diagnostic basis. Thus, invasive treatment of only discogenic axial or radicular pain is unsuccessful. Thermodiscoplasty, or intradiscal electrothermal therapy (IDET), is used for minimally invasive treatment of discogenic axial pain. Pulsed radiofrequency (PRF) of the dorsal root ganglion (DRG) is used as an interventional method for radicular pain elimination. We have proposed the simultaneous combined use of these techniques for the first time.
Objective: Our research aimed to study the dynamics of pain syndrome and disability in patients who have undergone simultaneous combined interventional treatment with the IDET and PRF DRG for chronic therapeutically resistant radicular and discogenic pain associated with intervertebral disc protrusion without spinal root compression, confirmed by motor and sensitive deficit absence.
Materials and Methods: A retrospective analysis of 22 patients treated at the Neurospine clinic (Kyiv) from 2019 to 2020 was carried out. All patients had the degenerative-dystrophic disease (protrusion) of the intervertebral discs L4-L5 and L5-S1 with therapeutically resistant lumbosacral pain. The standard examination included two-plane spondylography, magnetic resonance imaging, as well as an assessment of neurological status. The discogenic axial origin of pain was confirmed by provocative contrasting discography. The involvement of the spinal root (a radicular component of pain) was established by performing selective radicular blockade. The treatment results were assessed using the numerical Rating scale (NRS) and the Oswestry disability index (ODI); statistical processing was carried out using Microsoft Excel and Statistica-10 software.
Results: There were no complications detected. All patients noted a significant reduction in pain and decrease in disability: NRS Median (Me) before treatment = 7.77 ± 1.02, ODI (Ме) before treatment = 70.45 ± 7.85; NRS (Me) immediately after procedure = 2.18 ± 1.13. This trend persisted for six months: NRS (Me) 6 months after procedure = 2.0 ± 0.75, ODI (Me) 6 months after procedure = 30.45 ± 9.98.
Conclusion: The simultaneous combined use of IDET and PRF DRG is an effective and safe treatment for therapeutically resistant chronic lumbosacral pain associated with intervertebral disc protrusion.
Keywords: intervertebral disc protrusion; radicular pain; discogenic axial pain; thermodiscoplasty; pulsed radiofrequency ablation.
Introduction
The prevalence of people suffering from pain in the lower back (LBP) with or without irradiation to the lower extremities in developed countries is similar to the one of a pandemic. It is not only a serious medical problem but also a socio-economic one. In the United States and Western Europe, the prevalence of LBP reaches 40–80 %, and the annual incidence is 5 %. It is the second most frequent reason for visiting a doctor after respiratory diseases and the third one regarding the frequency of hospitalizations [8]. In 85 % of cases, the cause of LBP is nonspecific; in 8 %, it is caused by tumors, metastases, compression fractures, ankylosing spondylitis, in 7 % - spinal stenosis, intervertebral disc degeneration, and radiculopathy [5,25]. In more than 50 % of patients with LBP, the severity of pain decreases after 1 week, and in 40 % of cases, improvement occurs after 8 weeks. The rest of the patients continue to experience pain for more than 6 months. In 70–90 % of patients, pain in the lower back recurs after some time [23]. The relationship between low back pain and irritation of the intervertebral discs was established by C. Hirsch and K. Lindblom in 1948 [11,17]. The attempts to eliminate LBP using intradisk procedures continue.
M.Van Kleef, R., M.Karasek and N.Bogduk [3,13,33] used intradiscal radiofrequency heating as a method of disc dereception. One of the methods of thermocoagulation of discs is IDET thermodiscoplasty (intradiscal electrothermal therapy). The method is based on warming up the disc using an electrothermal catheter inserted into the disc percutaneously through a trocar. In the disc, the catheter is passed in the form of a loop along the inner surface of the lateral and posterior walls of the annulus fibrosus. This significantly increases the area of electrothermal action [24]. The two most probable mechanisms are suggested for the effectiveness of this procedure: thermal denervation (deafferentation) of the disc and thermal restructuring and denaturation of collagen fibers [6,14]. In a healthy intervertebral disc, only the outer layers of the annulus fibrosus receive innervation and vascularization. They are in the area of responsibility of the subvertebral nerve, which is mixed. Intradiscal sensory fibers are mainly nociceptive (Bogduk, 1983). With degeneration of the intervertebral disc, local inflammatory reactions are stimulated. As a result, the cracks of the annulus fibrosus are replaced by granulation tissue with vessels, and nerve fibers grow into deeper layers up to its central sections. This process is accompanied by an increase in the density of disc innervation [25]. Pulse radiofrequency ablation (PRF) of the posterior spinal root ganglion (DRG) is considered in the spectrum of interventional treatment of radicular pain. The usual, continuous radiofrequency exposure to these structures is unacceptable due to the high risk of deafferentation and motor block development. Thus, the non- destructive technique of pulse neuromodulation is the most attractive for potential use. This method consists of the paraneural placement of an electrode connected to a radio frequency generator. The high- frequency current in the pulse mode leads to a partial disruption of the transmission of the nerve signal. The effect is achieved by acting primarily on the C-fibers responsible for the conduction of the pain impulse [4,14]. This significantly reduces radicular pain. Both components of pain - axial and radicular - can often be present in a patient with LBP, and it is impossible to distinguish it only based on a clinical and visual-diagnostic basis. Thus, treating only radicular or discogenic pain is unsuccessful (Scholz et al., 2009). We offer combined interventional radiofrequency treatment for lumbosacral pain caused by intervertebral disc protrusions.
Objective: To study the dynamics of pain syndrome and disability in patients undergone simultaneous combined interventional treatment with the IDET and PRF DRG for chronic therapeutically resistant lumbosacral pain associated with intervertebral disc protrusion [12] without spinal root severe compression, which confirmed motor and sensitive deficit absence.
Materials and Methods
A retrospective analysis of 22 patients was conducted: 16 males (73 %) and 6 females (27 %). They were treated in the Neurospine clinic (Kyiv) from 2019 to 2020 for radicular and discogenic axial therapeutically resistant LBP. Patients were aged 22 to 64 years (Me = 47±13.7). Routine examination included dual plane spondylography, magnetic resonance imaging, and neurologic assessment. The inclusion criterion was the presence of therapeutically resistant chronic lumbar discogenic axial and radicular pain. Before visiting the clinic, patients received drug therapy for at least 12 weeks without any significant effect (Figure 1, Figure 2). The Numerical Rating Scale (NRS) was used to determine the severity of pain. We evaluated the pain syndrome - discogenic axial and radicular pain - in each patient in a complex manner. The NRS scale was used by us to assess the dynamics of pain syndrome before treatment, immediately after it, 1 and 6 months after the procedure. The Oswestry Low Back Pain Disability Questionnaire (ODI), developed by JC Fairbank et al. in 1980, was used to assess patient disability. This questionnaire is rather cumbersome and time-consuming to complete. At the same time, it allows for a broader reflection of the various spheres of the patient's life. The questionnaire includes 10 sections describing complaints and violations in various spheres of the subject's life. Each section contains six descriptions of the possible condition of the patient, of which each first is estimated at 0 points, every sixth - at 5 points. The total assessment is made by dividing the sum of the received points in all sections by the maximum possible (50) with the expression of the received indicator as a percentage.
ODI = ( ): 50 x 100 = %.
We used the ODI questionnaire to assess the patient's disability before the procedure, 1 month after treatment, and 6 months after. The assessment of disability due to disease was also carried out comprehensively, including disability from discogenic axial and radicular pain.
The study did not include previously operated patients, patients with spinal stenosis, instability of the spinal motion segments, or sequestered disc hernias with increasing neurological deficit.
|
Severity of pain (NRS) |
Number of patients |
Percentage (%) |
|
6 |
3 |
13 |
|
7 |
5 |
24 |
|
8 |
8 |
36 |
|
9 |
6 |
27 |
Figure 1: Severity of pain (NRS) before procedure
|
Disability (ODI) |
Number of patients |
Percentage (%) |
|
60 |
6 |
27 |
|
70 |
9 |
41 |
|
80 |
7 |
32 |
Figure 2: Patient`s disability (ODI) before procedure.
The indication for the procedure was the presence of intervertebral disc protrusion up to 6 mm with mild stenosis of the spinal canal according to Bonneville [14], the height of the intervertebral fissure retained at least half, and the presence of no more than two symptomatic discs (Figure 3).
Figure 3: MRI. Patient G. (F, 29 y.o.). Protrusion L4L5, chronic therapeutically resistant lumbosacral (L4 and L5 left) pain.
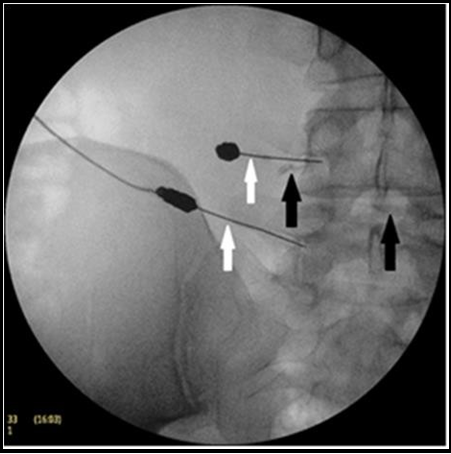
Clinical signs of radicular pain were presented by relevant irradiation: along the front surface of the hip and the medial surface of the lower leg - for the L4 root; on the posterolateral surface of the hip, the lateral surface of the leg, the medial edge of the foot up to 1- 2 toes - for the L5 root; along the back of the hip and lower leg to the lateral edge of the foot - for the S1 root. All patients had a positive Lasegue symptom (straight leg raising test). There were no significant motor and sensory deficits found. Spinal root involvement was confirmed by selective radicular block with 5.0 ml of 0.5 % lidocaine solution; in a result radicular pain disappears. Affected intervertebral disc was verified by provocative discography with 30 % iohexol solution at a pressure < 50 psi (3.4 atm) and a volume of < 3 ml. It was done to confirm the clinical significance of discogenic axial pain’s source. The procedure of thermodiscoplasty (IDET) underwent 9 (40 %) intervertebral discs at the L4-L5 level and 11 (50 %) at the L5-S1 level. In 2 (10 %) cases, the procedure was performed on both levels. Our proposed technique consists in the simultaneous combined use of IDET and PRF DRG. This method is protected by the Patent of Ukraine UA 128574 U [28]. The procedure was performed in the following terms. The patient was placed in a prone position on an X-ray transparent operating table. Under radiological control (C-arm), a 17G cannula was inserted from the paravertebral approach into the intervertebral disc using local anesthesia with 5.0 ml of 0.5 % lidocaine solution. Provocative discography was performed, while the level of damage and the integrity of the disc ring were clinically confirmed: the positive effect was manifested by provocation of discogenic axial pain. Then, the electrode with a working tip of 40 mm in length was inserted into the cannula. The catheter with electrode were attached to a radiofrequency generator (Radionics RFG 3C Plus). Using the tunnel imaging technique, a 22G cannula with a 5 mm working tip was inserted into the intervertebral foramen directly next to the dorsal root ganglion. To prevent motor deficits, testing was carried out in sensory (frequency - 50 Hz, pulse - 1 ms, voltage - 0.4–0.6 V) and motor (frequency - 2 Hz, pulse - 1 ms, voltage - 0.8–1,2 V) mode. During testing, the patient noted paresthesia in the corresponding dermatome, and there was no motor activity. This was an indication of the correct positioning of the electrode. To avoid intrathecal or intravascular positioning of the electrode, 0.5–1.0 ml of an X-ray contrast solution (Iohexol 35 %) was injected into the cannula in the fluoroscopy mode. The next step was radiofrequency treatment (Figure 4).
Figure 4: Patient G. (F, 29 y.o.). IDET L4-L5 and PRF DRG L4 and L5 (left).
Procedure`s field (black arrows indicate an intradiscal catheter for thermodiscoplasty, white arrows indicate an electrode for radio frequency pulse ablation of the posterior spinal root ganglion).
The protocol for its implementation consists of two parts, which were performed simultaneously. The first part was to perform thermodiscoplasty (IDET). A high frequency current (500 kHz) was applied to the intradiscally installed catheter electrode in a continuous mode. In this case, the working part of the catheter was heated in steps: 50° C for 120 s, 55° C for 120 s, 60° C for 120 s and 65° C for 240 s. Thus, thermal modification of collagen fibers and deactivation of nociceptors was achieved (Figure 5).
Figure 5: Patient G. (F, 29 y.o.). Lateral intraoperative fluorogram: sequential advancement of the IDET catheter into the intervertebral space.
The traces of X-ray-positive solution (indicated with white arrow) for provocative discography are visualized in the intervertebral space.
The second part (PRF DRG) was performed in a pulse mode, which, due to the effect primarily on the nerve C-fibers, provides a decrease in the conduction of the pain impulse. Two series of 120 seconds each were performed, during which the temperature of the electrode tip should not exceed 42° C. Pulses had a frequency of 500 kHz and the duration of each is 2 ms. (Figure 6).
Figure 6: Patient G. (F, 29 y.o.). AP intraoperative fluorogram: white arrows indicate electrodes for pulse radio frequency; black arrows mark traces of a contrast agent in the intervertebral space (right) and near the L4 root (left).
The procedure was completed by removing the electrodes with cannulas and applying an aseptic dressing for 5-6 hours. Post- procedural observation with bed rest lasted 1.0–1.5 h. During this observation, the dynamics of pain syndrome were assessed, and the general somatic state (blood pressure, pulse, temperature, oxygen saturation) and neurological status (motor and sensory functions in the lower extremities) were monitored. The criteria for the adequacy of the treatment were a decrease in pain by more than two-thirds immediately after the procedure in the absence of motor and sensory deficits of the corresponding root.
Results
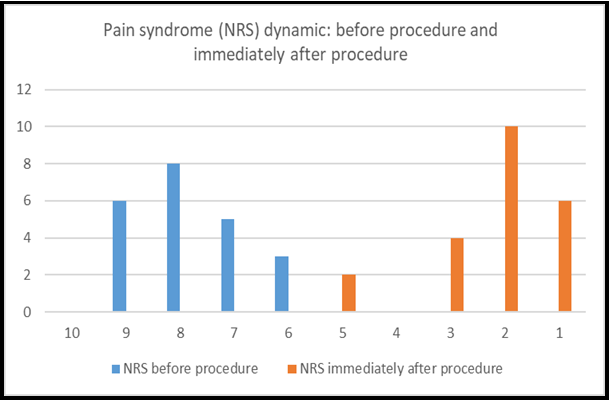
Complications during the procedure and after them were not observed. A significant analgesic effect was observed immediately right after the procedure. Most patients in the pre-procedure period characterized pain sensations as “terrible, leading to distress,” assessing them by NRS from 6 to 9 (Me = 7.77 ± 1.02). Moreover, on the first day after the procedure, the maximum number of patients described the pain as “weak but bothering,” corresponding to NRS from 1 to 5 (Me = 2.54 ± 1.01). Those uncomfortable feelings were often myogenic, caused by the inevitable trauma of soft tissue during access (Figure 7).
Figure 7: The severity of pain before and immediately after the procedure (numerical rating scale NRS, 1987). The abscissa axis is the severity of pain, the ordinate axis is the number of patients.
The results of treatment 1 month after the procedure testified to the persistence of a tendency towards a decrease in pain syndrome: more than 60% of the treated patients noted an almost complete absence of bothering sensations, and about a third of patients characterized pain as “weak” (NRS Me = 2.18 ± 1.01). A similar pattern persisted for 6 months, after which the subjects rated their pain according to NRS from 1 to 3 (Me = 2.0 ± 0.75) (Figure 8).
Figure 8: The severity of pain before procedure and 1 month and 6 months after procedure (numerical rating scale NRS, 1987). The abscissa axis is the severity of pain, the ordinate axis is the number of patients.
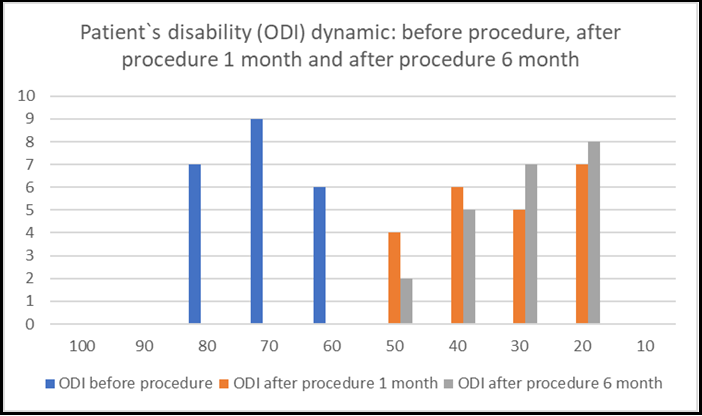
Noteworthy, in our opinion, are the data obtained using the Oswestry Low Back Pain Disability. Before the procedure, patients determined their disability in the range from 60 to 80 points according to ODI (Me = 70.45 ± 7.85), which corresponds to a rather low vital energy. One month after the procedure, most of the patients could stay in an upright position for much longer, which allowed them to take part in public life, as well as take long trips.
Many of the patients were able to care for themselves without taking analgesics. A significant part of the subjects noted the normalization of sleep (Me ODI = 33.18 ± 11.29). This trend persisted after 6 months: by the end of our observation period, patients characterized the degree of their social adaptation according to ODI in the range from 20 to 50 points (Me = 30.45 ± 9.98) (Figure 9).
Figure 9: Dynamics of patient`s disability indicators before procedure and 1 month and 6 months after procedure according to ODI (Oswestry Low Back Pain Disability Questionnaire, 1980). The abscissa axis is the disability index (%); the ordinate axis is the number of patients.
Discussion
Our research's aim - is to study the dynamics of pain syndrome and disability in patients who have undergone simultaneous combined interventional treatment with the IDET and PRF DRG for chronic therapeutically resistant radicular and discogenic axial LBP associated with intervertebral disc protrusion without spinal root compression, which was confirmed by motor and sensory deficit absence. Based on this, the working hypothesis was that the proposed combined interventional radiofrequency technique (PRF DRG and IDET) has a sufficient clinical effect in the form of prolonged analgesia and patient disability reduction.
We took the liberty of comparing our results with colleagues' data in separate positions (PRF DRG and IDET) because the complex radiofrequency technique we proposed was applied for the first time. Immediately after the procedure, the decrease in pain by NRS was significant (p < 0.05) on average 4 times. A similar picture was recorded one month after treatment, the median (Me) decreased to almost a minimum. It should also be noted that one month after the procedure, NRS did not have significant differences (p = 0.13) with similar indicators immediately after the procedure (Figure 8). Results similar to ours were obtained by A. Teixeira, M.Grandinson, and ME.Sluijter, using pulsed radiofrequency ablation of the dorsal root ganglion in the lumbar spine, achieved a significant (p < 0.01) reduction in pain from 7.83 to 2.25 according to VAS within 4 weeks [29]. The same result was presented in the work of SJ.Kim: Using PRF DRG, they noted a significant (p = 0.033) reduction in pain ≥ 50 % in half of the cases [15]. M.van Kleef et al., using IDET in patients with chronic LBP, report adequate pain relief in 54 % of patients within 8 weeks after the procedure [33]. At the next stage of this study, it seems appropriate to assess the effectiveness of combined radiofrequency exposure in terms of the patient's disability according to the ODI scale (Figure 9). As the obtained data shows, the procedure significantly reduced the disability of patients in the early stages. This is evidenced by a significant decrease in the ODI index by 2.7 times within a month after treatment (p = 0.009). K.van Boxem and his coauthors came to similar conclusions, proclaiming PRF DRG as a valuable option in treating chronic radicular pain [30,31]. At the same time, based on a review of the literature on the interventional treatment of lumbar radicular pain, M.J.DePalma and L.Manchikanti conclude that PRF DRG and IDET are of limited feasibility [2,18]. Y-C.Kim, recognizing the mechanism of action of PRF is not completely clear, nevertheless recommends it for the treatment of radiculopathies and, at the same time, obtains impressive results: a decrease in pain according to VAS from 9/10 to 5/10 and a significant improvement in the patient's quality of life [14]. B. Morlion is skeptical about any intradiscal procedures for treating LBP and about IDET in particular [21]. The assessments of the indicators carried out 6 months after the procedure can be conditionally attributed to the long-term treatment results. Given the peculiarity of chronic pain and the course duration of discogenic radiculopathies, these data are of particular interest. According to the information received (Figure 6), pain sensations 6 months after the procedure continued to remain at a low level. Thus, the obtained analgesic effect was retained for up to six months (NRS Me = 2.0 ± 0.75). F.M.Philips and C.Lauryssen have achieved impressive results using IDET to treat LBP: pain reduction according to VAS decreased from 7.4 ± 1.9 before treatment to 1.4 ± 1.9 by the third month after procedure [22]. These numbers largely correlate with our results. This is even more important because the above authors, like us, carried out multilevel IDET procedures. In a study A.Kircelli and coauthors, the first month after IDET, were not convincing enough regarding pain relief by VAS. However, the six- month results demonstrated a significant (p < 0.0001) pain regression of 57.39 % and an improvement in ODI by 47.16 % [16]. Using PRF DRG for the treatment of discogenic lumbosacral radiculitis, T.T. Simopopulos achieved a significant analgesic effect (70 % reduction in pain intensity) for periods ranging from 3 months to one year [27]. At the same time, J.W. Geurts and colleagues, presenting a similar methodology, showed no difference in results with the placebo group (p = 0.43). His study showed that after 3 months, only 16 % of patients were successful with manipulation [9]. Van Boxem confirms the high efficiency of PRF DRG: pain reduction by 50 % within 6 months in 22.3 % of subjects [31,32]. The comparative analysis of the treatment results regarding the patient's disability allowed us to establish that the proposed method after 3 months shows high efficiency since it improves the ODI score by 2 times. Similar results persist after 6 months, which once again emphasizes the high efficiency of radiofrequency interventional treatment. V. Mehta and his colleagues analyzed the results of PRF DRG in patients with radicular pain due to lumbar extrusions from 1 week to 3 months after treatment. Improvement of ODI and VAS indicators was noted at least twofold. The authors explain this by normalizing peripheral and central sensitization [20]. R. Derby and coauthors have found impressive IDET results in 62.5 % of patients with chronic discogenic pain: 4.82 points of pain reduction by VAS in 6 months. These authors emphasize that the correctness of the discography assessment and the procedure is largely determined by its effectiveness [3]. M.Karasek and N.Bogduk, having studied the results of the use of IDET, came to the following conclusions: by 6 months after surgery, 60 % of patients had a decrease in pain according to VAS by half, and 53 % of patients refused to take analgesics and started professional duties [13]. According to K. Thompson, functional improvement after IDET was noted on average by 15.8 points for SF-34. The same results were published by B. Liu and V. Singh. J.S. Saal and J.A. Saal reported a VAS pain reduction six months after IDET, from an average of 6.57 to 3.71. G.B.J. Andersson and S.Ahuja emphasize that 81% of their patients are satisfied with the IDET results, and 61 % fully recovered their ability to work [24]. On the other hand, B.J. Freeman and colleagues did not find convincing evidence of disability reduction in people who underwent IDET. In their study, the following ODI dynamics were observed: from 41.42 on average before IDET to 39.77 6 months after the procedure. There was no significant difference in these results compared with the placebo group (ODI = 40.74 and ODI = 41.58, respectively), which allowed the authors to conclude that this procedure was ineffective [6]. E. Veizi and S. Hayek also consider the benefits of IDET very questionable, criticizing both the selection of patients and controversial evidence of electrothermal effects on the biomaterial of the intervertebral disc [34]. The results of B. Webster and Coauthors were also modest: 23 % of patients after IDET required surgery, 55 % continued to take analgesics, 37 % underwent lumbar blockade, and only 39 % of patients started work. T. Davis also concluded that IDET was ineffective: Six months after the procedure, 97 % of patients had lumbar pain, and six had to undergo fusion. The analgesic effect was noted only by 39 % of patients, while in 29 %, the intensity of the pain syndrome remained the same, and in 29 %, it increased. Moreover, at the same time, half of the patients were completely satisfied with the treatment result. We did not find convincing evidence of the effectiveness of IDET presented by M. Spruit and W.C.Jackobs. They found that the outcome of the procedure varied from complete elimination of pain and functional disorders to a clear increase in these indicators, although on average, the severity of the analgesic effect increased significantly (p = 0.046) in 6 months after IDET [24]. While recognizing, in general, the positive results obtained in our work, the following limitations should be emphasized: a small number of observations (only 22 patients), the absence of a control group, and a relatively short period of retrospective analysis (up to 6 months).
Conclusion
The combined simultaneous use of IDET and PRF DRG is an effective and safe treatment option for chronic lumbosacral pain associated with intervertebral disc protrusion without spinal root severe compression.
There is no conflict of interest in this work.
References
- Chistik T (2015) Low back pain: algorithms for diagnosis and effective treatment. [Чистик, Т. Боль в нижней части спины: алгоритмы диагностики и эффективного лечения]. Bol'. Sustavy. Pozvonochnik. 3(19): 43-45.
- DePalma MJ, Bhargava A, Slipman CW (2005) A critical appraisal of the evidence for selective nerve root injection in the treatment of lumbosacral radiculopathy. Arch Phys Med Rehabil. 86(7): 1477–1483.
- Derby R, Eek B, Chen Y, O'neill C, Ryan D (2000) Intradiscal electrothermal annuloplasty (IDET): A novel approach for treating chronic discogenic back pain. Neuromodulation. 3(2): 82-88.
- Erdine S, Bilir A, Cosman ER, Cosman ER (2009) Ultrastructural changes in axons following exposure to pulsed radiofrequency fields. Pain Pract. 9(6): 407-417.
- Eun IS, Park WW, Suh KT, Kim JI, Lee JS (2009) Association between osteoprotegerin gene polymorphism and bone mineral density in patients with adolescent idiopathic scoliosis. Eur Spine J. 18(12): 1936-1940.
- Freeman BJ, Walters RM, Moore RJ, Fraser RD (2003) Does intradiscal electrothermal therapy denervate and repair experimentally induced posterolateral annular tears in an animal model? Spine (Phila Pa 1976). 28(23): 2602-2608.
- Freeman BJ, Mehdian R (2008) Intradiscal electrothermal therapy, percutaneous discectomy, and nucleoplasty: what is the current evidence? Curr Pain Headache Rep. 12(1): 14–21.
- Freynhagen R, Baron R, Gockel U, Tölle TR (2006) PainDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Current Medical Research and Opinion. 22(10): 1911-1920.
- Geurts JW, van Wijk RM, Wynne HJ, Hammink E, Buskens E, et al. (2003) Radiofrequency lesioning of dorsal root ganglia for chronic lumbosacral radicular pain: a randomised, double-blind, controlled trial. Lancet. 361(9351): 21–26.
- Helm Ii S, Simopoulos TT, Stojanovic M, Abdi S, El Terany MA (2017) Effectiveness of thermal annular procedures in treating discogenic low back pain. Pain Physician, 20(6): 447- 470.
- Hirsch C (1948) An attempt to diagnose the level of disc lesion clinically by disc puncture. Acta Orthop.Scand. 18(1-4): 132– 140.
- Ho AL, Desai AM (2016) Intervertebral disc degeneration. Prevalence, risk factors and treatments. Nova Science Publishers, Inc., New York. 283 pp.
- Karasek M, Bogduk N (2000) Twelve-month follow-up of a controlled trial of intradiscal thermal anuloplasty for back pain due to internal disc disruption. Spine (Phila Pa 1976). 25(20): 2601-2607.
- Kim DH, Kim Y-C, Kim K-H (2011) Minimally invasive percutaneous spinal techniques. Elsevier Saunders, Philadelphia PA. 486 pp.
- Kim SJ, Park SJ, Yoon DM, Yoon KB, Kim SH (2018) Predictors of the analgesic efficacy of pulsed radiofrequency treatment in patients with chronic lumbosacral radicular pain: a retrospective observational study. Journal of Pain Research. 26(11): 1223–1230.
- Kircelli A, Coven I, Cansever T, Sonmez E, Yilmaz C (2017) Patient selection and efficacy of IDET with respect to the Dallas Discogram Score. Turk. Neurosurg. 27(4): 623-630.
- Lindblom K (1948) Diagnostic puncture of intervertebral disks in sciatica. Acta Orthop Scand. 17(3-4): 231-239.
- Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, et al. (2013) An update of comprehensive evidence-based guidelines for interventional technique in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 16(2 Suppl): S49-283.
- Marcia S, Saba L (2017) Radiofrequency treatments on the spine. Springer. Cham, Switzerland. 109 pp.
- Mehta V, Snidvongs S, Ghai B, Langford R, Wodehouse T (2017) Characterization of peripheral and central sensitization after dorsal root ganglion intervention in patients with unilateral lumbosacral radicular pain: a prospective pilot study. Br J Anaesth. 118(6): 924–931.
- Morlion B (2013) Chronic low back pain: pharmacological, interventional and surgical strategies. Nat Rev Neurol. 9(8): 462- 473.
- Philips FM, Lauryssen C (2009) The lumbar intervertebral disc. Thieme, NewYork-Stuttgart. 305 pp.
- Povoroznyuk VV (2011) Pain in the lower back. Prevalence, causes, mechanisms of development and diagnostic features. [Поворознюк, В.В. Боль в нижней части спины. Распространенность, причины, механизмы развития и особенности диагностики] Bol'. Sustavy. Pozvonochnik. 1(01): 120-130.
- Prodan AI, Kutsenko VA, Kolesnichenko VA (2005) Dereception of Intervertebral Discs: Old Idea – New Technologies. Hirurgiâ pozvonočnika. 4: 55-60.
- Roberts S, Eisenstein S.M, Menage J, Evans E.H, Ashton I.K (1995) Mechanoreceptors in intervertebral discs. Morphology, distribution, and neuropeptides. Spine (Phila Pa 1976). 20(24): 2645-2651.
- Romanenko VI, Romanenko IV, Romanenko Yu I (2016) Clinical profiles of patients with chronic lumbosacral pain syndromes. Trauma. 17(2): 78-85.
- Simopoulos TT, Kraemer J, Nagda JV, Aner M, Bajwa ZH (2008) Response to pulsed and continuous radiofrequency lesioning of the dorsal root ganglion and segmental nerves in patients with chronic lumbar radicular pain. Pain Physician. 11(2): 137–144.
- Smolanka V.І, Fedurtsya V.M, Pavlov B.B. Ukrainian Patent No. UA 128574 U.
- Teixeira A, Grandinson M, Sluijter ME (2005) Pulsed radiofrequency for radicular pain due to a herniated intervertebral disc–an initial report. Pain Pract. 5(2): 111–115.
- Van Boxem K, Cheng J, Patijn J, van Kleef M, Lataster A, et al. (2010) Lumbosacral radicular pain. Pain Practice. 10(4): 339- 358.
- Van Boxem K, Huntoon M, Van Zundert J, Patijn J, van Kleef M, et al. (2014) Pulsed radiofrequency: a review of the basic science as applied to the pathophysiology of radicular pain. Reg Anesth Pain Med. 39(2): 149–59.
- Van Boxem K, van Bilsen J, de Meij N, Herrler A, Kessels F, et al. (2011) Pulsed radiofrequency treatment adjacent to the lumbar dorsal root ganglion for the management of lumbosacral radicular syndrome: a clinical audit. Pain Med. 12(9): 1322– 1330.
- Van Kleef M, Barendse G.A.M, Wilmink J.T, Lousberg R, Bulstra S.K, et al. (1996) Percutaneous intradiscal radiofrequency thermocoagulation in chronic non-specific low back pain. Pain Clin. 9(3): 259–268.
- Veizi E, Hayek S (2014) Interventional therapies for chronic low back pain. Neuromodulation. 17(2): 31–45.