Sofia Ferreira Rodrigues1*, Mariana Teves2, João Lopes Dias3, Paula Ambrósio4, Carlos Barros5, Carlos Marques6
1Maternidade Dr. Alfredo da Costa, Centro Hospitalar Universitário de Lisboa Central
2Hospital do Divino Espírito Santo
3Centro Hospitalar Universitário de Lisboa Central
4Maternidade Dr. Alfredo da Costa, Centro Hospitalar Universitário de Lisboa Central
5Maternidade Dr. Alfredo da Costa, Centro Hospitalar Universitário de Lisboa Central
6Maternidade Dr. Alfredo da Costa, Centro Hospitalar Universitário de Lisboa Central
*Corresponding Author: Sofia Ferreira Rodrigues, Maternidade Dr. Alfredo da Costa, Centro Hospitalar Universitário de Lisboa Central.
Abstract
Non-puerperal uterine inversion is a rare condition, generally caused by benign, or more rarely malignant, uterine pathology, that folds the uterine fundus into the vagina. In this report, we present the case of a 19-year-old teenager without coitarche, admitted to the emergency room for abnormal uterine bleeding, pelvic pain, and urinary retention. Pelvic MRI (Magnetic Resonance Imaging) revealed complete uterine inversion, probably originating from an endometrial lesion with 82x66x50mm resected after laparotomic reversion of uterine inversion. The histological diagnosis was embryonal rhabdomyosarcoma.
Keywords: non-puerperal uterine inversion, abnormal uterine bleeding, embryonal rhabdomyosarcoma, magnetic resonance imaging
Introduction
Non-puerperal uterine inversion is a severe condition in which the uterine fundus folds into the endometrial cavity. However, the mechanism for this pathology has not been identified. This condition is scarce and is generally caused by benign, or more rarely, malignant uterine pathology, most frequently submucous myomas (57.2%) [1,2]. The second most prevalent cause is leiomyosarcoma (13.5%) [2]. There is no prevalence data on this condition, but a systematic review found 170 cases reported between 1940 and 2017, with a mean age of 46.5 ± 17.4 years [2]. The inversion can be classified as incomplete when the fundus is in the endometrial cavity or complete when the fundus protrusion through the cervix [3]. The main symptoms of non-puerperal uterine inversion are vaginal discharge, abnormal uterine bleeding, and pelvic discomfort [4]. Symptoms are most likely nonspecific, which leads to a challenging diagnosis. After that, an accurate diagnosis is essential to offer appropriate management.
This article reports a case of non-puerperal uterine inversion associated with embryonal rhabdomyosarcoma. Written informed consent was obtained from the patient for publication of this report and any accompanying images.
Clinical case
A 19-year-old teenager presented at our Gynecology and Obstetrics Emergency Unit with a 3-month history of abnormal uterine bleeding (menorrhagia) and, in the previous three days, urinary retention, vomiting, and pelvic pain. The only relevant condition from the past medical history was a body mass index of 45 kg/m2. Menarche was at 15 years of age, and there was a history of irregular cycles (oligomenorrhea). The patient denied coitarche. Surgical and family history were irrelevant.
The patient was hemodynamically stable (blood pressure 115/72mmHg, heart rate 85 beats per minute), apyretic, and pale. Algaliation was performed, with clear urine output. At gynecological examination (after patient consent), a voluminous exophytic mass at cervix localization with hard consistency and foul-smelling active vaginal bleeding was detected. Laboratory tests showed anemia with hemoglobin 7.4 x 10g/L and hematocrit 23.4%. The urine test showed no leucocytes.
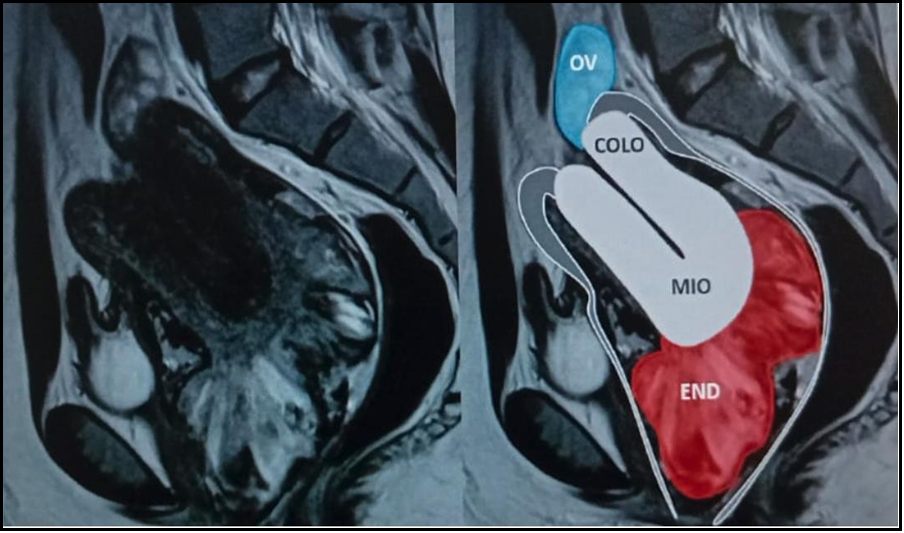
Because of the limitations of pelvic ultrasound, which revealed a heterogeneous endometrial thickening of 29 mm, the patient underwent magnetic resonance imaging (MRI) (Image 1), showing a complete uterine inversion, probably originating from an endometrial lesion with 82x66x50mm. A biopsy of the mass was attempted, but the histopathology result was inconclusive.
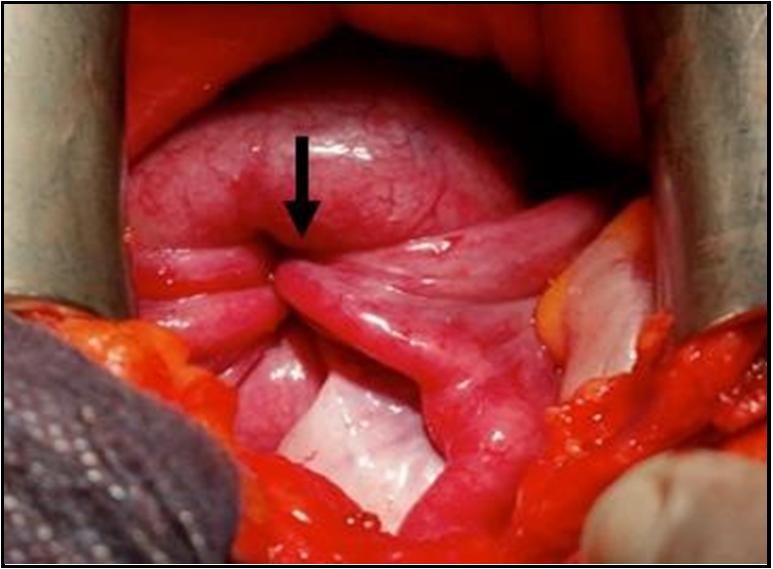
The patient was admitted and received 2U erythrocyte concentrate before surgical correction. An attempt to restore the uterus anatomy vaginally was made (Johnson maneuver - manual pressure applied on the fundus through the vagina), but unsuccessful. The medical team then proceeded to exploratory laparotomy with a Pfannenstiel incision, which revealed the classic “flowerpot” appearance, with a complete inversion with involvement of the uterus, bilateral round ligaments, and fallopian tubes (Image 2). To restore the uterus anatomy, a median incision in the anterior wall was needed, from the isthmus to the fundus, which showed an amorphous and necrotic tumor that was resected and sent for pathology. After the removal of the mass, the uterus restored its natural position, and median hysterorrhaphy in one plane was performed.
The day after surgery, uterine bleeding, and pelvic pain decreased significantly, and the patient began to urinate spontaneously. The patient was discharged from the hospital on day 7 post-op, with 8.6 x 10g/L of hemoglobin. The histological diagnosis was “high-grade malignant mesenchymal neoplasm,” consisting of small, round, and blue cells with infiltrative growth and areas with myxoid stroma.
Neoplastic cells were CKAE1AE3 (-), CAM5.2 (-), Desmin (+), Myogenin (-), Chromogranin (-), and Synaptophysin (-).
Thoracic CT scan and abdomen and pelvic MRI, two weeks after the surgery, revealed a normal uterus position, endometrial thickening of anterior wall in continuity with tumor resection zone; some solid nodules in pre-uterine topography, probably tumor implants, the biggest with 13 x10 mm and 14 x 10 mm; suspicion of peritoneal implants in both adnexal areas, the biggest with 10 x 7 mm; and suspicious adenomegaly in left external iliac chain with 18 x 10 mm. The patient was referred to a specialized oncology center due to the rarity of the tumor. After pathology revision, the final diagnosis was embryonal rhabdomyosarcoma, with probable peritoneal and adnexal metastasis.
Image 1: MRI in sagittal image with complete uterine inversion, probably originating from the endometrium that is thickened and heterogenous, or myometrium. The image shows one ovary above the cervix. END – endometrium, MIO – myometrium, COLO – cervix, OV – ovary.
Image 2: Image from exploratory laparotomy with an arrow indicating the site of uterine inversion with round ligaments and bilateral tubes pulled in - the classic “flowerpot” appearance.
Discussion
Non-puerperal uterine inversion is a scarce condition. The diagnosis is challenging since the presenting symptoms, such as abnormal uterine bleeding and pelvic pain, are nonspecific. If based only on physical examination, the diagnosis is difficult, where a vaginal mass of undetermined origin can be observed, and the uterine fundus cannot be palpable on bimanual examination [5]. Imaging is essential for the diagnosis, but pelvic ultrasound has some limitations. Transabdominal ultrasound can show a mass at the cervicovaginal level, but the uterine morphology is difficult to explore [5], while transvaginal sonography can reveal the mass [3]. MRI is the best imaging modality for the diagnosis of uterine inversion and for characterizing the underlying lesion while studying the surrounding structures [3]. In the gynecological exam, our patient had a voluminous exophytic mass at cervical localization with a stiff consistency. Our differential diagnosis included cervical mass and spontaneous expulsion of a submucosal uterine fibroid. As in other cases found in the literature, the diagnosis of our patient was made by MRI.
In cases of incomplete inversion, particularly in childbearing-age women, conservative treatment should be performed until the final histopathologic diagnosis is done. In the other cases, treatment generally consists of hysterectomy [5]. Although the uterine inversion was complete, our patient was 19 years old and nulliparous, so the surgical team opted to revert the uterus to its normal position, which was only feasible with the opening of the anterior wall and accessing the mass at the fundal level of the uterus.
The histological result was embryonal rhabdomyosarcoma. Rhabdomyosarcoma is a primitive pediatric malignant soft tissue sarcoma of skeletal muscle phenotype originating from a primitive mesenchymal cell [6]. Most cases are diagnosed in children under 6 years old. Embryonal rhabdomyosarcoma is the most prevalent type of rhabdomyosarcomas (60%). This tumor can arise anywhere in the body, and the most common metastatic sites include lung, bone marrow, and lymph nodes [6].
There are three cases of non-puerperal uterine inversion caused by embryonal rhabdomyosarcoma published in the literature (Table 1) in patients between 15 and 22 years old. All cases presented abnormal uterine bleeding, and two presented a vaginal mass. The three instances underwent a total abdominal hysterectomy, chemotherapy, and radiotherapy. The outcome of one case is unknown, and the other 2 cases had a maximum survival time of 20 months after diagnosis.
Table 1: Summary of the literature – non-puerperal uterine inversion cause by embryonal rhabdomyosarcoma
|
Author, year |
Age (years) |
Presentation |
Treatment |
Outcome |
|
Ojwang, 2006 [7] |
16 |
Abnormal uterine bleeding |
Neoadjuvant chemotherapy, total abdominal hysterectomy, radiotherapy |
- |
|
da Silva, 2008 [8] |
15 |
Abnormal uterine bleeding, vaginal mass |
Total abdominal hysterectomy, chemotherapy, radiotherapy |
Death 9 months after surgery |
|
Ambreen, 2019 [9] |
22 |
Abnormal uterine bleeding, vaginal mass |
Total abdominal hysterectomy, bilateral salpingo-oophorectomy, chemotherapy, radiotherapy |
Liver metastasis after 12 months. Survival time - 20 months after diagnosis |
Conclusion
Uterine inversion is a rare event, usually associated with the puerperal period. However, in sporadic cases, it may occur outside this period, generally caused by benign or, more rarely, malignant uterine pathology. Because the symptoms are nonspecific, diagnosis is challenging, but the possibility of an underlying malignant tumor should not be neglected. MRI is the best imaging modality for the diagnosis of uterine inversion.
References
- Liu H, Bi Z, Hu Q, Liu S, Dong Z, et al. (2022) Non-puerperal Uterine Inversion with endometrial polyps in an 11-year-old girl: A Case Report. J Pediatr Adolesc Gynecol. 35(2): 188-191.
- Silva BR, Meller FO, Uggioni ML, Grande AJ, Silva NC, et al. (2018) Non-Puerperal Uterine Inversion: A Systematic Review. Gynecol Obstet Invest. 83(5): 428–436.
- Guerrouj I, Aichouni N, Haddar L, Abbou W, Arghal M, et al. (2023) Magnetic resonance imaging of non-puerperal total uterine inversion due to a leiomyoma. Radiol Case Rep. 18(5): 1821- 1824.
- Gowri V (2000) Uterine inversion and corpus malignancies: a historical review. Obstet Gynecol Surv. 55(11): 703–7.
- Leconte I, Thierry C, Bongiorno A, Luyckx M, Fellah L (2016) Non-puerperal uterine inversion. J Belg Soc Radiol. 100(1): 47.
- Dagher R, Helman L (1999) Rhabdomyosarcoma: An overview. Oncologist. 4(1): 34-44.
- Ojwang SB, Rana F, Sayed S, Aruasa WK (2006) Embryonal rhabdomyosarcoma with uterine inversion: case report. East Afr Med J. 83(3): 110-3.
- da Silva BB, Dos Santos AR, Bosco Parentes-Vieira J, Lopes- Costa PV, Pires CG (2008) Embryonal rhabdomyosarcoma of the uterus associated with uterine inversion in an adolescent: A case report and published work review. J Obstet Gynaecol Res. 34(4 Pt 2): 735-8.
- Ambreen A, Ahmed F, Zafar S, Khan S (2020) A case report of an aggressive rhabdomyosarcoma associated with non-puerperal uterine inversion. J Obstet Gynaecol. 40(3): 434-437.