Niare Ndour1*, Assane Diop2, Fallou Niang3, Mamadou Ba1, Ahmadou Gaye1, Fatimata Ly2
1Department of Internal Medicine and Dermatology, Cheikh Ahmadoul Khadim Hospital, Touba, Senegal
2Dermatology Department, Institute of Social hygiene, Dakar, Senegal
3Oto-rhino-laryngology (ORL) Department, children's hospital Albert Royer, Dakar, Senegal
*Corresponding Author: Niare Ndour, Department of Internal Medicine and Dermatology, Cheikh Ahmadoul Khadim Hospital, Touba, Senegal.
Abstract
Herpes zoster is a viral disease caused by reactivation of the varicella-zoster virus (vzv), which is mainly described in adults with compromised immune systems, and the elderly. Involvement of children in general, and infants in particular, is rarer. We report a new case of herpes zoster in a two-year-old immunocompetent infant of intercostal topography.
This was a 2-year-old infant from a full-term pregnancy with no family history of varicella. This child was admitted to our department, accompanied by his mother, with a non-febrile rash that had been evolving for about 3 days. Questioning did not reveal any behaviour suggesting pain, such as incessant crying or unusual agitation. On examination, the child was in good general condition, had no fever and other vital signs were normal. Examination of the hairless skin revealed vesicular lesions with an erythematous base, not pruritic, arranged in clusters in the left intercostal space, following a path well bounded by the anterior and dorsal thoracic midline. The diagnosis of intercostal herpes zoster was thus made in view of this very characteristic clinical presentation. The child was treated with local care, including antiseptic baths and the application of desiccants to the lesions. No antiviral medication or antibiotics were administered. The lesions healed well after ten days, leaving a few hypochromic macules. There was no post-herpetic pain after healing.
Introduction:
Herpes zoster is a viral disease caused by reactivation of the varicella- zoster virus (vzv), which remains quiescent in sensory nerve ganglia after primary varicella infection. This condition is mainly described in adults with compromised immune systems and in the elderly. Involvement of children in general, and infants in particular, is rarer, and most cases are reported in series or as isolated clinical cases [1,2,3,4]. Although the semiology of the rash is identical in adults, there are nevertheless some clinical and evolutionary particularities in children. We report a new case of herpes zoster in a two-year-old immunocompetent infant of intercostal topography.
Observation:
This was a 2-year-old infant from a full-term pregnancy with unremarkable birth features. There was no family history of varicella.
Indeed, the mother had not developed chickenpox or shingles, either during pregnancy or in the post-partum period. Her father also had no known pathology. There had been no cases of varicella in the family since the child's birth. This child was admitted to our department, accompanied by his mother, with a non-febrile rash that had been evolving for about 3 days. Questioning did not reveal any behaviour suggesting pain, such as incessant crying or unusual agitation.
On examination, the child was in good general condition, had no fever and other vital signs were normal.
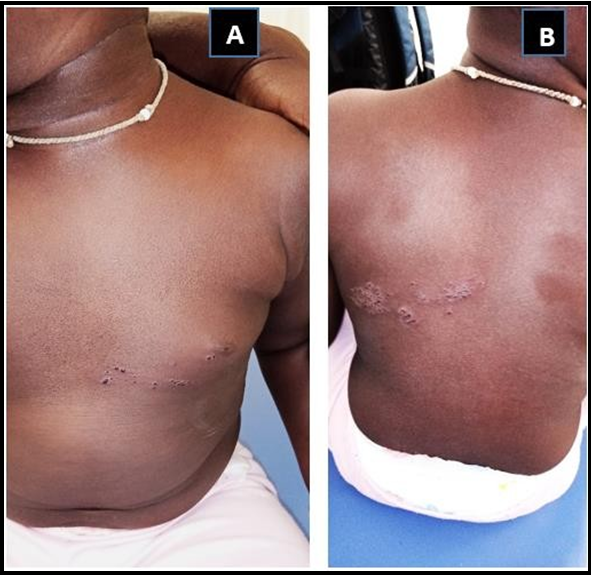
Examination of the hairless skin revealed vesicular lesions with an erythematous base, not pruritic, arranged in clusters in the left intercostal space, following a path well bounded by the anterior and dorsal thoracic midline (Figure 1).
Figure 1: intercostal shingles in a 2-year-old infant
A: front view B: posterior view
The rest of the physical examination was normal. The diagnosis of intercostal herpes zoster was thus made in view of this very characteristic clinical presentation. Biological tests for acquired immunodepression were negative.
The child was treated with local care including antiseptic baths and the application of desiccants to the lesions. No antiviral medication or antibiotics were administered.
The lesions healed well after ten days, leaving a few hypochromic macules (Figure 2). There was no post-herpetic pain after healing.
Figure 2: Favourable evolution of herpes zoster lesions after 7 days of treatment, leaving a few hypochromic macules
A: front view B: posterior view
Discussion
Herpes zoster is a viral disease caused by reactivation of the varicella- zoster virus (vzv), which remains quiescent in nerve ganglia. This is a double-stranded DNA virus with an outer envelope and a tropism for the skin and nervous system. After primary infection, vzv migrates into the dorsal root neurons of nerve ganglia, where it remains in a latent state, expressing only a small proportion of their glycoproteins. Node colonization can occur via retrograde transfer or viremia from skin lesions [5]. VZVs reactivated in the nerve ganglia will colonize the epidermis in a metameric distribution after migration. These are responsible for the characteristic shingles rash. The host immune system plays an important role in maintaining the virus in a latent state, acting via cellular immunity. Reactivation of the virus that causes shingles only occurs when cellular immunity fails, even temporarily [6]. This explains its frequency in the elderly and immunocompromised. In immunocompetent children, the development of shingles is thought to be due to the immaturity of the immune system at the time of varicella infection. Varicella contracted before the age of 1 increases the risk of shingles in infants. The younger the age at which chickenpox is contracted, the shorter the average time to onset of shingles, particularly during the first year of life [7]. Transmission of VZV to the child or fetus can occur during the antenatal, perinatal or postnatal period. In the antenatal period, transmission occurs via the transplacental route when the mother has chickenpox, particularly in cases of high viremia, especially during the first 36 weeks [8]. This transmission is all the more important when the maternal rash occurs 5 days before delivery. This exposes the newborn to the risk of severe neonatal varicella, due to the absence of protection by maternal antibodies, which are only produced 7 days after the rash [9].
Transmission can occur in the postnatal period, particularly during the first few weeks, with the greatest risk occurring within 2 days of delivery [9]. It can be transmitted via the respiratory or cutaneous route from varicella lesions in the mother or a close relative. Thus, neonatal varicella presents a very heterogeneous spectrum of clinical expression, depending on the timing of the rash in the mother in relation to the term of pregnancy, and ranges from benign forms that can go undetected to malignant, sometimes fatal forms.
In our case, no history of chickenpox was found, either in the infant, the mother or another family member. However, given the age of onset of herpes zoster, at 2 years, we cannot be certain of the absence of varicella, even benign, during the preceding months.
The incidence of herpes zoster in the paediatric population varies from one study to another and according to the populations studied. The incidence is estimated at 0.74 and 1.38 cases per 1000 inhabitants per year, for the age groups between birth and 9 and 10 and 19 respectively [10]. The incidence of herpes zoster is higher in children with cancer, the most commonly reported being acute leukemia [11].
Clinically, unlike in adults, shingles in infants is not very symptomatic, generally characterized by the absence of neurological signs, particularly neuropathic pain. However, the cutaneous picture is similar, in the form of an eruption of vesicles grouped in clusters along a dermatome, sometimes associated with fever. These vesicles may coalesce into bullae, whose initially clear contents become cloudy and ulcerate, forming crusts. Intercostal topography is the most common, but other sites such as the ophthalmic region can be affected [12,2]. In our case, herpes zoster was of intercostal topography and no symptoms were noted at the time of diagnosis.
Treatment of herpes zoster in infants is essentially symptomatic and rarely requires antiviral therapy. The most widely used is aciclovir at a dosage of 20 mg/kg/d for approximately one week [13]. However, in the case of herpes zoster ophthalmicus or in immunocompromised children, antiviral treatment is essential [14].
Complications include bacterial superinfections, anterior uveitis, encephalitis and meningoencephalitis. Post-herpetic neuralgia is exceptional [7].
To date, the prevention of shingles by vaccination has no indication for infants, but is still indicated for high-risk newborns, particularly those whose mothers have had chickenpox 5 days before and 2 days after delivery. This vaccination reduces symptomatic and severe forms of the disease by 50% [15].
Conclusion:
Our case corroborates previous studies on the existence of herpes zoster in infants. It is unusual in that the mother did not suffer from varicella or herpes zoster during pregnancy or after delivery. Any vesicular eruption, even if asymptomatic, should be considered in infants.
References
- Sah CM, Shrestha S, Chaudhary N (2020) Herpes zoster in an 11‐ month‐old immunocompetent infant: A rare case report. Clinical Case Reports. 8(8): 1483‑1485.
- Ikhlef M, Saadi S (2023) Ophthalmic herpes zoster in an immunocompetent five-year-old child. J Fr Ophtalmol.
- Agharbi FZ (2019) Herpes zoster in children: about two cases. Pan Afr Med J. 32: 199.
- Meziane M, Ismaili N, Benzekri L, Senouci K (2023) Zona: mise au point et traitements actuels.
- Floret D (2020) Varicelle et zona de l’enfant. Journal de Pédiatrie et de Puériculture. 33(2): 52‑68.
- Arvin AM, Pollard RB, Rasmussen LE, Merigan TC (1978) Selective impairment in lymphocyte reactivity to varicella-zoster antigen among untreated lymphoma patients. J Infect Dis. 137(5): 531–540.
- Leung AK, Robson WL, Leong AG (2015) Herpes Zoster in Childhood. OJPed. 20(5): 300-3.
- Enders G, Miller E, Cradock-Watson J, Bolley I, Ridehalgh M (1994) Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 343(8912): 1547–1550.
- Methlouthi J, Mahdhaoui N, Bellalah M, Ayache H, Nouri S, et al. (1998) Infections à VZV. Formes de la femme enceinte et du nouveau-né. Médecine et Maladies Infectieuses. 28(11): 782‑90.
- JIM.fr [Internet]. 00:00:00+01 [cité 13 déc 2023]. ZONA DANS LE L’ ENFANCE.
- Lin HC, Chao YH, Wu KH, Yen TY, Hsu YL, et al. (2016) Increased risk of herpes zoster in children with cancer: A nationwide population-based cohort study. Medicine. 95(30): e4037.
- Fatima-Zahra A (2019) Zona de l’enfant: à propos de deux cas. The Pan African Medical Journal [Internet].
- LaRussa PS, Marin M (2011) Varicella-Zoster Virus Infections. In: Nelson Textbook of Pediatrics [Internet]. Elsevier. p. 1104- 1110.e1.
- Nikkels AF, Nikkels-Tassoudji N, Piérard GE (2004) Revisiting Childhood Herpes Zoster. Pediatric Dermatology. 21(1): 18‑23.
- Blumental S, Lepage P (2019) Management of varicella in neonates and infants. BMJ Paediatr Open. 3(1): e000433.