Aw Aïssatou*, Sy El Hadji Malick, Mbaye Soda, Ba Alassane, Gaye Serigne Sohibou, Ndiaye Mouhamed, Senghor Ousmane Ndiaga, Ndiaye Lamine, Seyid El Hadji Abdellahi, Diouf Mamadou, Ndiaye Arfang, Diagne Jean Pierre, Ka Aly Mbara, Ndiaye Papa Amadou
Ophthalmology Center of Abass Ndao Hospital, Dakar-Senegal
*Corresponding Author: Aw Aïssatou, Ophthalmology Center of Abass Ndao Hospital, Dakar-Senegal.
Abstract
Introduction: serpiginous choroiditis belongs to the spectrum of fundus white spot syndrome. It is responsible for ischemia and dysfunction of the pigment epithelium and outer retina.
We report a case of serpiginous choroiditis to show its different aspects on multimodal imaging.
Observation: A 59-year-old patient consulted for central scotoma of the right eye. Visual acuity was hand motion on the right and 20/25 on the left. The anterior segment was normal in both eyes and intra ocular pressure was 12mmHg. The fundus was normal on the left and showed a patch of yellowish-white infiltrate on the posterior pole of the right eye. Auto-fluorescence showed damage to the pigment epithelium, associated on optical coherence tomography with damage to the outer retina. OCT-angiography showed ischemia of the choriocapillaris in the affected area.
Discussion: Serpiginous choroiditis is a rare, chronic, relapsing-remitting disease affecting middle-aged subjects with no gender predisposition. In the majority of cases, no etiology is found. Diagnosis is based on clinical appearance and exclusion of alternative diagnoses.
Conclusion: Multimodal imaging is essential for the diagnosis of serpiginous choroiditis. It helps to distinguish it from borderline forms, with which it shares clinical features.
Keywords: fundus white spots, pigment epithelium, outer retina
Introduction
Serpiginous choroiditis (SC), also known as geographic helicoid peripapillary choroidopathy, is a rare, often bilateral inflammatory disease affecting the outer retina and choriocapillaris in middle-aged patients with no gender predilection [1]. The classic form of the disease affects the peri papillary region and progressively extends to the macular area. It is characterized by confluent patches of yellowish-white infiltrates that progress to atrophy [2]. The natural history of SC is characterized by recurrence, usually adjacent to atrophic scars [3]. Multimodal imaging plays a considerable role in the diagnosis and follow-up of this pathology. In fundus autofluorescence (FAF), areas of hyperautofluorescence are an indicator of activity, while hypoautofluorescence shows regression of the inflammatory process, or even atrophy of the retinal pigment epithelium (RPE) [4]. Optical coherence tomography (OCT) shows specific retinal damage, depending on the acute or chronic stage of the disease. OCT A confirms choriocapillary damage, with flow hypodensity. On fluorescein angiography, active lesions are hypofluorescent in the early stages, then become impregnated in the late stages. In indocyanine green angiography (ICG), lesions are hypofluorescent at all times [5].
Case report
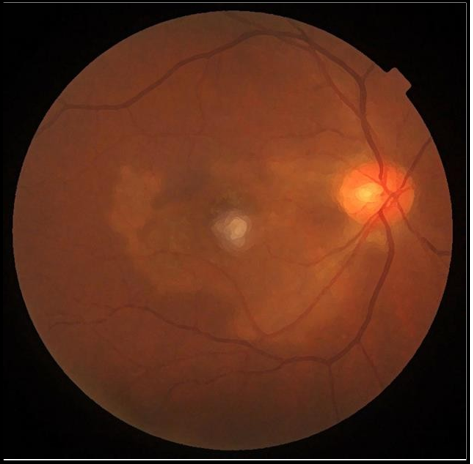
A 59-year-old melanoderma patient presented with a central scotoma in his right eye that had been present for three days. He reported no particular antecedents. On examination, visual acuity (VA) was " hand motion" on the right and 20/25 on the left. Anterior segment and intraocular pressure were normal in both eyes. On the right, the fundus showed a patch of yellowish-white infiltrate in the form of a geographic map (Figure 1), appearing to originate in the peri- papillary region and reaching the macular region without vitreous reaction. Iconography with Topcon's Swept Source OCT Triton showed in FAF, hypo autofluorescence areas surrounded by hyper auto fluorescent borders with a serpiginous appearance (Figure 2). OCT had shown thinning of the outer nuclear layer with atrophy of the photoreceptor layers and thickening of the choroid (Figure 3). OCT-angiography revealed ischemia of the choriocapillaris in the affected area (Figure 4). Examination of the left eye was normal. The patient never returned for follow-up.
Figure 1: Fundus on the right showing yellowish-white central lesions in a geographic map
Figure 2: autofluorescence image showing hypoautofluorescent areas framed by a hyperautofulorescent border, reflecting disease activity.
Figure 3: OCT B scan showing thinning of the outer nuclear layer with alteration of the photoreceptors and thickening of the choroid.
Figure 4: OCT angiography showing ischemia of the choriocapillaris
Discussion
Although the etiology of SC remains largely unknown, it has been the subject of much speculation. Today, the inflammatory/autoimmune etiology is the most widely accepted. Its prevalence is estimated at 0.6% of uveitis cases in tertiary centers in Germany and 5% in the United States [6]. In India, this prevalence is increased to 14.4% [7], probably due to the frequency of tuberculosis. Although initially described in caucasian patients, SC occurs in all types of patients. The disease can appear between 20 and 70 years with a mean age between 35 and 50 years. The prevalence is equal in both genders [8].
The diagnosis of SC is based on clinical appearance and the exclusion of alternative diagnoses. On the fundus, acute lesions are yellow-grey and well-defined, then progress to an atrophic appearance, with lesion margins that may be hyperpigmented. Acute lesions develop on the edges of old lesions. They evolve from the juxta papillary zone towards the periphery, with pseudopod extensions giving a serpiginous or amoeboid appearance [9]. Involvement is classically bilateral but asymmetrical and delayed in time.
In our patient, the damage was unilateral, but bilateralization could not be ruled out as the patient had been lost to follow-up.
Auto-fluorescence has emerged as a valuable tool for assessing and monitoring disease activity in SC patients. Active lesions initially appear hypo-auto-fluorescent due to the masking effect of the adjacent edematous retina. Hyperauto-fluorescence then progressively appears, probably due to the accumulation of phagocytosis debris in the RPE cells. In the scarring phase, lesions are hypo-auto-fluorescent due to atrophy of the RPE. A hyperautofluorescent border is sometimes visible at the edge of the lesion, reflecting damage to the RPE [9].
Structural OCT is an essential examination in the evaluation of SC and its complications. Active lesions result in hyper-reflective areas in the outer retina, with extensive damage to the ellipsoid zone and preservation of the inner retina. The choroid appears thickened, with hyper-reflective intrachoroidal spots. Scarring lesions result in atrophy of the photoreceptor layer, the RPE and the choriocapillaris, with or without fibrotic hyperreflective subretinal lesions [10]. The presence of subretinal fluid in the active phase is classic and should not be confused with a neovascular complication [2].
Few series in OCT-A imaging have been published to date. A factor limiting the use of this device in SC is an unreliable automatic segmentation requiring manual segmentation. In OCT-A, the areas of atrophy of the choriocapillaris are more extensive than the areas of atrophy of the pigment epithelium, indicating the choriocapillaris as the site of primary inflammation. OCT-A confirms the involvement of the choriocapillaris by showing a hypodensity of flow, corresponding to the area in hypofluorescence on ICG angiography. This examination clearly makes it possible to differentiate between a recurrence of the disease which results in the appearance of a new hypodense lesion contiguous to a pre-existing lesion and a neovascular complication which shows an abnormal vascular network [2,9].
El Ameen [11] considers that OCT-A could be very useful for routine monitoring of SC because it is easy to perform and non-invasive, but that during the initial evaluation, ICG angiography remains preferable because it more clearly delineates choriocapillary lesions.
Conclusion
SC is a recurrent and aggressive disease with a poor prognosis. Progression of chorioretinal lesions results in the formation of large atrophic scars. In practice, a multimodal imaging approach is essential for the diagnosis and monitoring of SC and for the detection of possible secondary neovascularization.
References
- Bodaghi Bahram, Creuzot-Garcher Catherine, Delyfer Marie- Noëlle, et al. Retine et vitré. Elsevier Health Sciences, 2018.
- Korobelnik JF (2019) OCT en ophtalmologie. Elsevier Health Sciences.
- Desai R, Nesper P, Goldstein DA, Fawzi AA, Jampol LM, et al. (2018) OCT Angiography Imaging in Serpiginous Choroidopathy. Ophthalmology Retina. 2(4): 351‑359.
- Weber M (2022) Imagerie multimodale dans les uvéites postérieures. Les Cahiers d'Ophtalmologie. 258: 36-40.
- Bousquet É (2021) Syndrome des taches blanches du fond d’œil : rappels et nouveautés. Les Cahiers d'Ophtalmologie. 244:19-23.
- Jakob E, Reuland MS, Mackensen F, Harsch N, Fleckenstein M, et al. (2009) Uveitis subtypes in a German interdisciplinary uveitis center—analysis of 1916 patients. The Journal of Rheumatology. 36(1): 127-36.
- Biswas J, Narain S, Das D, Ganesh SK (1996) Pattern of uveitis in a referral uveitis clinic in India. International ophthalmology. 20(4): 223 - 8.
- Laatikainen L, Erkkilä H (1981). A Follow-up Study on Serpiginous Choroiditis. Acta Ophthalmologica. 59(5): 707‑18.
- Hoogewoud F, Guex-Crosier Y, Bousquet É (2023) Épithéliopathie en plaque, choroïdite serpigineuse et leurs formes frontières. J Fr Ophtalmol. 46(6): 646‑657.
- Abroug N, Khairallah M, Mahmoud A, Messaoud R, Khairallah M (2021) Épithéliopathie en plaques et choroïdite serpigineuse. Réalités Ophtalmologiques.; 284: 2.
- El Ameen A, Herbort CP (2018) Serpiginous choroiditis imaged by optical coherence tomography angiography. Retinal Cases & Brief Reports. 12(4): 279‑85.