H Kalzén1,2, BA Larsson3, L Lindberg4, O Ingemansson5, C Frostell1*, S Eksborg2,6
1Department of Anaesthesia and Intensive Care at Danderyd Hospital, Karolinska Institutet at Danderyd Hospital (KIDS), Stockholm, Sweden.
2Department of Paediatric Anaesthesia, Intensive Care and ECMO services, Astrid Lindgren Children's Hospital, Karolinska Institutet, Karolinska University Hospital Solna, Stockholm, Sweden.
3Department of Physiology and Pharmacology, Section of Anaesthesiology and Intensive Care, Karolinska Institutet, Astrid Lindgren Children's Hospital, Karolinska University Hospital Solna, Stockholm, Sweden.
4Department of Anaesthesia and Intensive Care, Children’s Hospital, Paediatric Intensive Care Unit, University Hospital of Lund, Lund, Sweden.
5Department of Paediatric Intensive Care, The Queen Silvia Children's Hospital, Sahlgrenska University Hospital, Gothenburg, Sweden.
6Childhood Cancer Research Unit, Department of Women's and Children's Health, Karolinska Institutet, Astrid Lindgren Children's Hospital, Karolinska University Hospital Solna, Stockholm, Sweden.
*Corresponding Author: C Frostell, (Orcid ID: 0000-0002-7199-1310), Department of Anaesthesia and Intensive Care at Danderyd Hospital, Karolinska Institutet at Danderyd Hospital (KIDS), Stockholm, Sweden.
Abstract
Aim: This study sought to investigate the hypothesis that children dying outside a pediatric intensive care unit (PICU) after PICU discharge have a limitation of medical treatment (LOMT) order in place, limiting PICU readmission at the time of death.
Methods: A cohort was identified of all children (n=3890; 5019 admissions) treated in a PICU in Sweden over 3 consecutive years between January 1, 2008, and December 31, 2010. Survival was determined up to 4 years post-PICU discharge. For the 268 children who died during the study period, notes were checked for demographic data, LOMT, and place of death in a PICU, in a hospital ward, or at home.
Results: For 252 (94%) of the 268 deceased children, place of death and LOMT status (yes/no) for readmission to PICU care were identified. For 107 of those 252 studied (42%), the place of death was outside a PICU (in hospital or at home). For 80 (75%) of these 107 children, a written LOMT in the patient notes stating "no readmission to PICU care" was recorded. Home as the place of death was found for 36 of the 107 children (34%). For 27 (75%) of these 36 children, a written LOMT in the patient notes stating "no readmission to PICU care" was recorded.
Conclusion: In this study, we found that most children (75%) who died outside a PICU setting (in a hospital or at home) after PICU discharge had a LOMT recorded limiting their readmission to a PICU.
Keywords: PICU, mortality, prognosis, limitation of medical treatment, child, ethics
Introduction
The death of a child has become an increasingly uncommon event in most societies [1]. When this does happen due to an accident or intractable illness, providers and families wish the process to be as dignified as possible. When pediatric mortality is studied and discussed, these fundamental aspects must not be neglected.
When a cure or an acceptable quality of life is no longer possible or expected, the focus of care changes from prolonging life to promoting a dignified death [2]. A limitation of medical treatment (LOMT) order is often implemented to this end. We have previously reported on pediatric mortality in ICU care in Sweden and observed that an increase in late mortality could be seen at least 5 years after admission to an ICU [3]. However, data gathered then would not allow us to define this late mortality further in terms of existing LOMTs. In a second cohort of all children admitted to Swedish pediatric intensive care units (PICU s) from 2008 to 2010 [4], we found that 42% of Swedish children who died up to 4 years after PICU discharge had not been readmitted to a PICU at the time of death. We also explored which diagnostic groups were associated with this mortality, observing that patients belonging to the trauma and postoperative groups did not display significant late mortality. Interestingly—but perhaps not surprisingly—patients with chronic complex conditions (CCCs) and more than one admission to a PICU significantly deteriorated and became deceased compared to patient groups without CCC or a single PICU admission. Some of this late mortality can be anticipated in advance, allowing family members and caregivers time to plan for a terminally ill child.
LOMT orders, do not resuscitate, do not attempt cardiopulmonary resuscitation, and managed death are all examples of attempts to define the limitations of health care. These measures reflect attempts to adapt to the reality of a developing clinical situation and perhaps uphold the Hippocratic oath, "If not able to cure, at least bring comfort and do no harm." LOMT decisions in Sweden are usually made at a multidisciplinary meeting with help from the hospital's ethical board when needed. For children admitted to pediatric intensive care units (PICU), aspects of end-of-life situations and LOMT have been reviewed [5] and described in the literature for European, North and South American, and Asian PICU s [2,6-20]. The concept at present is widely accepted, but some differences in traditions have also been described [20,21]. To our knowledge, the presence of LOMT orders limiting readmission to PICU has yet to be described in detail. In the present study, we looked in more detail at all the 268 deaths identified, searching for possible LOMT orders limiting PICU readmission and place of death.
This study aimed to investigate the hypothesis that children dying outside a PICU after PICU discharge have a LOMT in place, limiting PICU readmission at the time of death.
Patients and Methods
A previously formed cohort was established of all children 0-16 years of age with a Swedish 10-digit personal identity number who were treated in a PICU in Sweden over 3 consecutive years from January 1, 2008, to December 31, 2010 (n=3688, 5019 admissions). Survival was checked up to 4 years post first (index) admission to PICU but no later than January 1, 2012. For the 268 children who passed away during the study period, records were checked for the presence of LOMT decisions stating no readmission to PICU care. The remaining 252 children with a clear y/n LOMT status were put into 3 groups according to the place of death: after being readmitted to a PICU (PICU group), in a hospital, but outside a PICU (Hospital group), or at home (Homegroup). Gender, age, survival time, admission diagnostic group, and the presence of a chronic complex condition (CCC) were identified for each patient. CCC was defined as "Any medical condition that can be reasonably expected to last at least 12 months (unless death intervenes) and to involve either several different organ systems or 1 organ system severely enough to require specialty pediatric care and probably some period of hospitalization in a tertiary care center" [21,22].
Patient admission diagnostic groups
The primary ICD-10 diagnosis stating the reason for index PICU admission was used to assign each patient to 1 of 7 direct admission diagnostic groups. These groups were compiled using the uniform diagnostic coding system used in the Australia and New Zealand Paediatric Intensive Care (ANZPIC) Registry [23]. All patients had one or multiple valid ICD-10 diagnoses registered during their PICU admission.
The diagnostic groups included injury, neurological, postoperative, cardiovascular, gastrointestinal/renal, respiratory, and miscellaneous. The miscellaneous group included sepsis, post-cardiac arrest, malignancies, endocrine disorders, and allergic reactions by the recommendations for the ANZPIC registry. Adjustments had to be made for the retrospective nature of the coding; for example, the ANZPIC registry group postoperative-cardiovascular had to be included in the cardiovascular group since it was impossible to differentiate postoperative admissions from other admissions with cardiovascular diagnoses. The diagnoses of postoperative ear-nose-throat/thoracic, postoperative neurologic, and postoperative other were all included in one group termed "postoperative."
During the study period, specialized PICU care was carried out at three locations in Sweden: The University Hospital of Lund, The Queen Silvia Children's Hospital at Sahlgrenska University Hospital of Gothenburg, and the PICU and ECMO Centres of Astrid Lindgrens Childrens' Hospital at Karolinska University Hospital in Stockholm. Data were collected directly from the three PICU s since the Swedish Intensive Care Registry was under implementation for PICU patients during the study period. For patients dying outside the 3 PICU s in their home hospitals or hometowns, data were provided through contact with the responsible clinicians. Changes to data systems in the hospitals and technical problems in accessing scanned notes were the main reasons for losses in follow-up.
Statistics
Survival for the 3 groups was evaluated using the Kaplan-Meier (K-M) method. Differences between curves were examined by Log-rank (Mantel-Cox) testing with Bonferroni corrections. Descriptive data and statistics, curves, and survival calculations were used using MS Excel (Microsoft Corporation, Redmond, Washington, USA) and GraphPad Prism 5.04 (GraphPad Software Inc., San Diego, USA). Data are presented as median values with interquartile ranges unless otherwise stated. P-values below 0.05 were considered statistically significant (two-sided testing).
Results
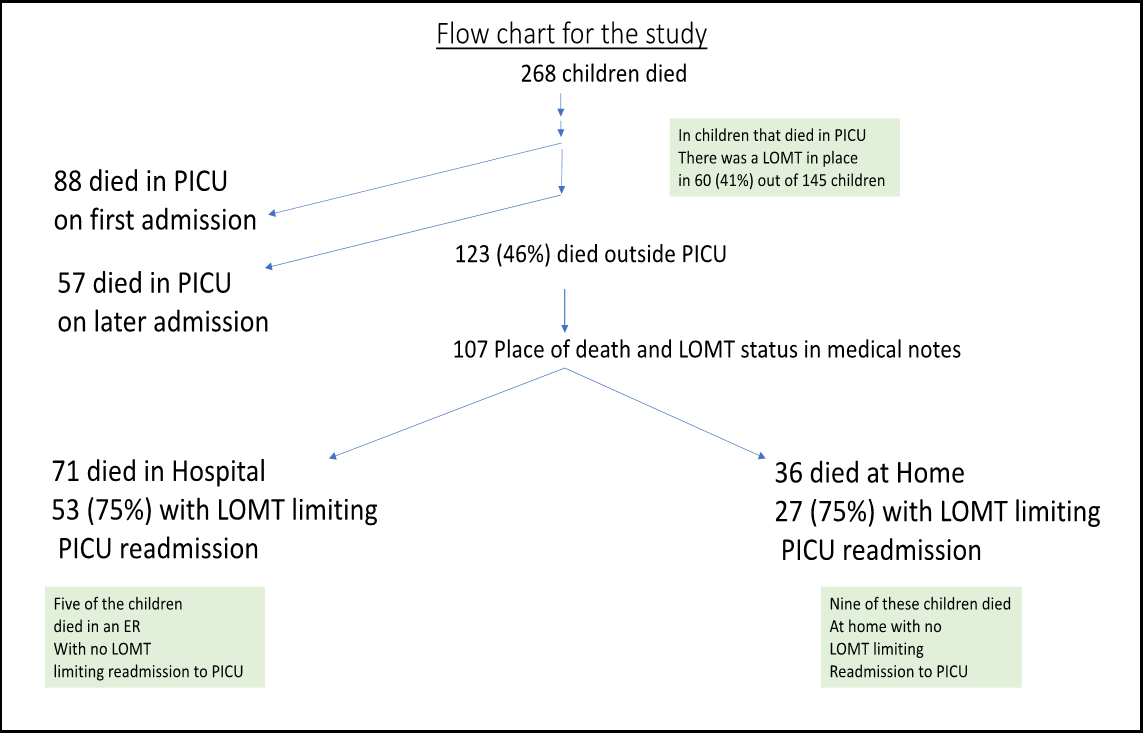
Out of 268 deceased children, place of death and LOMT status (yes or no to PICU care) could be identified for 252 (94%) with a 6% loss to follow-up. Of these 252 children, 107 (42%) died in a hospital but outside a PICU or at home. Of those 107, 80 (75%) had LOMT records limiting PICU readmission. A consort diagram is presented in Figure 1.
Figure 1. Cohort diagram (Flow chart for the study).
Demographic data including LOMT and CCC for the 3 groups are presented in Table 1.
|
Table 1. Demographic data and number of children in the three groups: deceased in PICU, in Hospital, or at Home |
|||
|
Deceased |
|||
|
|
In PICU |
In Hospital Outside PICU |
At Home |
|
Number of patients |
145 (58%) |
71 (28%) |
36 (14%) |
|
LOMT |
60 (41%) |
53 (75%) |
27 (75%) |
|
CCC |
91 (63%) |
51 (72%) |
27 (75%) |
|
Age at first PICU admission (years) |
0.30 (0.02 to 3.70) |
1.0 (0.20 to 7.50) |
1.80 (0.33 to 6.23) |
|
LOS at first PICU admission (days) |
2.66 (0.95 to 9.07) |
2.84 (0.87 to 6.67) |
1.70 (0.80 to 4.58) |
|
Numbers of admissions, median (range) |
1 (1-14) |
1 (1 to 12) |
1 (1 to 11) |
|
LOMT = limitation of medical treatment, CCC = complex chronic condition, LOS = length of stay at first PICU admission, |
|||
|
Age = age at first PICU admission, Admissions = average number of admissions for the children in the group during the study period. |
|||
Survival
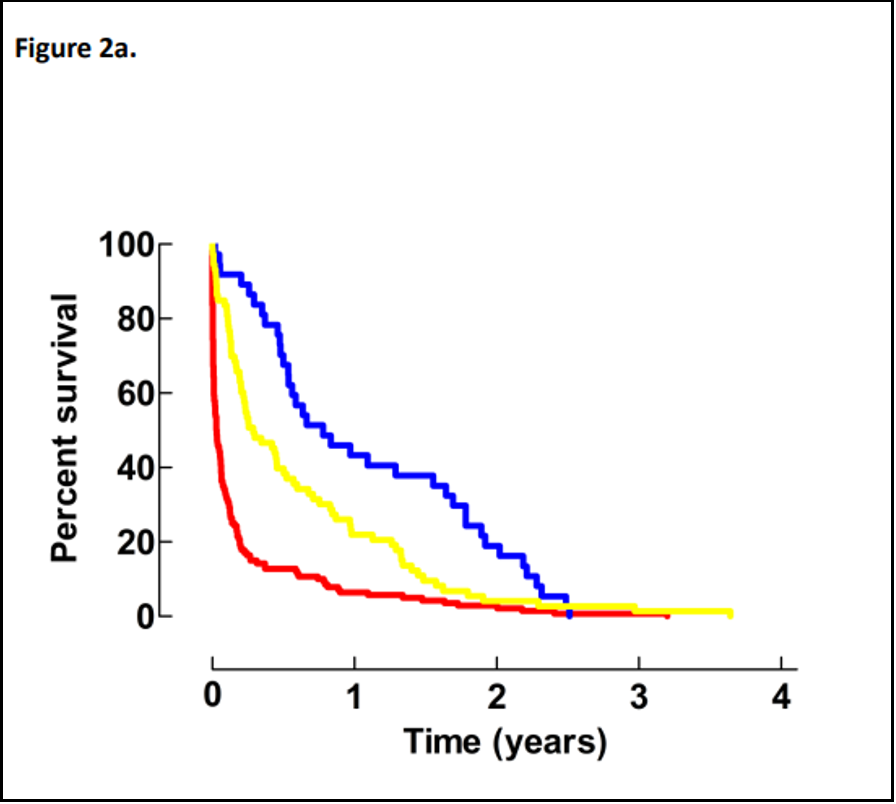
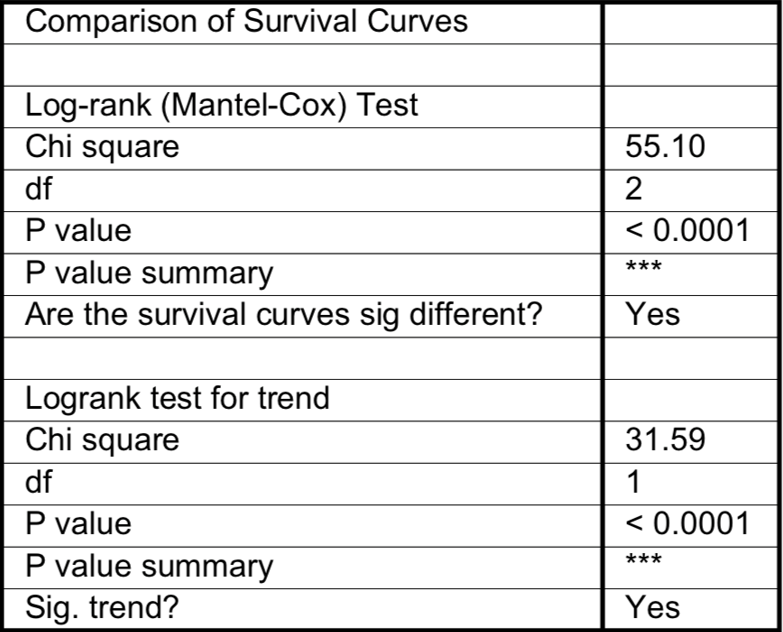
A significant difference in survival was observed between the 3 groups (p<0.0001), as noted in Figure 2a + 2b.
Figure 2a: Survival for the 3 groups over the time of the study. Place of death; red line PICU, yellow line in hospital, blue line at home.
Figure 2b. Statistical analysis with Bonferroni corrections indicated the survival in all groups differed significantly (PICU versus hospital and PICU versus home: p<0.0003; home versus hospital: p=0.0159).
The survival rate for all groups differed significantly after Bonferroni corrections (PICU versus hospital and PICU versus home: p<0.0003; home versus hospital: p=0.0159).
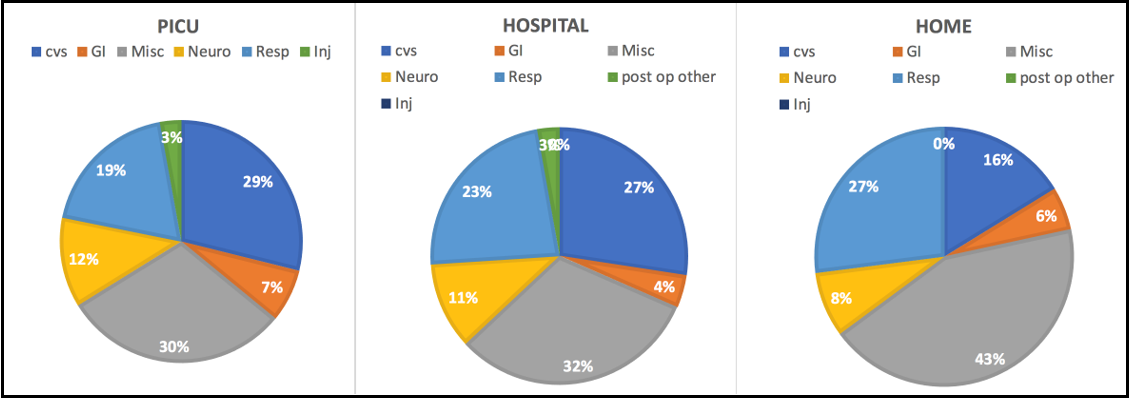
Admission diagnostic panorama
The diagnostic panorama at PICU admission was similar with regard to the place of death. However, children belonging to the cardiovascular and neurological groups appeared most frequently in the PICU group but uncommonly in the home group. Miscellaneous and respiratory patients were most common in the home group, as noted in Figure 3.
Figure 3. Admission diagnostic groups for the 3 locations of death (in PICU, in hospital, or at home).
Gender disposition
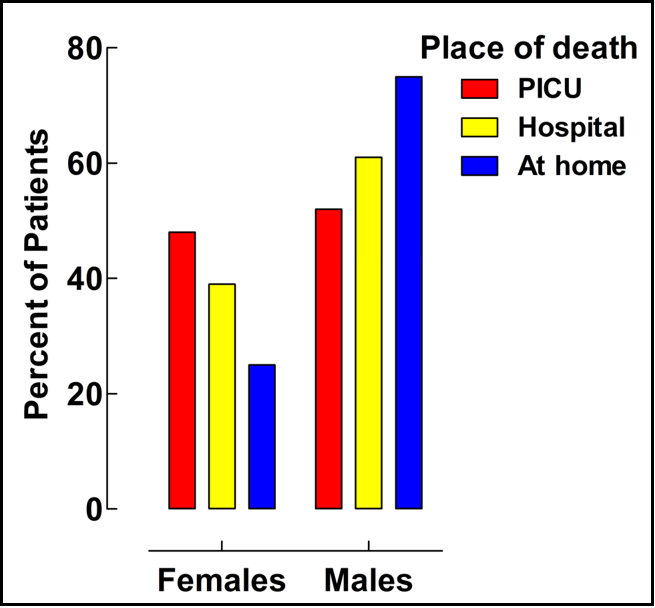
Gender disposition according to the place of death is presented in Figure 4. A higher proportion of boys died at home.
Figure 4: Gender disposition according to place of death.
No LOMT, Hospital, and Home group characteristics
Twenty-seven children died in a hospital or at home without LOMT orders. Their characteristics are presented in Table 2.
|
Table 2. Characteristics of patients who died in hospital or at home with no LOMT limiting readmission to PICU |
||
|
|
Deceased |
|
|
|
In Hospital |
At Home |
|
Female |
11 |
1 |
|
Male |
7 |
8 |
|
Age at first PICU admission (years) |
0.45 (0.02 to 4.58) |
0.90 (0.04 to 2.65) |
|
LOS at first PICU admission (days) |
4.54 (0.83 to 8.04) |
4.60 (1.31 to 6.23) |
|
Numbers of admissions, median (range) |
1 (1 to 12) |
1 (1 to 2) |
|
CCC |
14 |
5 |
|
Admission diagnostic group |
|
|
|
Miscellaneous |
3 |
3 |
|
Respiratory |
2 |
3 |
|
Cardiovascular |
12 |
3 |
|
Neurological |
- |
- |
|
Gastrointestinal |
1 |
- |
LOMT = limitation of medical treatment, CCC = complex chronic condition, LOS = length of stay at first PICU admission.
Median age at first PICU admission, Admissions = average number of admissions for the children during the study period.
Death in the emergency room
Five children (three males) in the Hospital group died in an emergency room without any LOMT record, limiting PICU readmission (CCC 4, cardiovascular 3, respiratory 2). Recorded reasons for death were as follows: left ventricular hypoplasia 1, pulmonary atresia 1, victim organic cordis (VOC) unspecified 1, cerebral malformation and acute airway infection 1, and respiratory insufficiency 1.
Lost to follow-up group characteristics.
For patients in this category, the median age was 2.3 years, slightly younger than the 3 groups studied (PICU /Hospital/Home). The median length of stay was 9 days, longer than that of the 3 groups. Characteristics are presented in Table 3.
|
Table 3. Characteristics of patients lost to follow-up |
|
|
Female |
7 |
|
Male |
10 |
|
Age at first PICU admission (years) |
1.40 (0.08 to 8.33) |
|
LOS at first PICU admission (days) |
2.11 (0.92 to 11.45) |
|
Missing place of death |
10 |
|
Unclear LOMT status |
7 |
|
CCC present |
13 |
|
Admission diagnostic group |
|
|
Miscellaneous |
5 |
|
Respiratory |
5 |
|
Cardiovascular |
4 |
|
Neurological |
2 |
|
Gastrointestinal |
1 |
LOMT = limitation of medical treatment, CCC = complex chronic condition, LOS = length of stay at first PICU admission.
Median age at first PICU admission, Admissions = average number of admissions for the children in the group during the study period.
Discussion
Place of death and LOMT status (yes/no for readmission to PICU care) could be identified in 252 (94%) of the 268 deceased patients. A majority (75%) of Swedish children not readmitted to PICU after discharge, upon developing a terminal illness, had a written LOMT order in place restricting their PICU readmission. Of the children dying at home, 75% had a CCC present, and 75% were male. There was no LOMT recorded for 9 of the children who died at home and 5 of those who died in an emergency room.
Whether a proportion of LOMT orders at 75% should be considered high is debatable. In Sweden, we tend to discuss an eventual LOMT by a broad consensus. A LOMT is decided only if there is a consensus within the pertinent medical group. In general, no LOMT is formed without consensus.
We used the database from a previously published study to identify Swedish children with at least one previous admission to a PICU [4]. This cohort had data for up to 4 years after such an event, with only a few patients (5.3%) lost to follow-up. Aspects of LOMT in the PICU setting have been discussed in the literature. The level of LOMT in the PICU group of our study was the same as that of a European multi-center study, EURYDICE II, showing a “decision to forgo life support” for 41% of the deaths in PICU [21]. We have found no other publications addressing LOMT measures for children who were discharged from PICU care and then died without readmission to a PICU.
A LOMT order can address every aspect of medical care. In its most basic form, it confronts the patient’s family with the imminence of death, the futility of further interventions and care, and the potential for harm from any renewed efforts to treat the patient. The goal of treatment then changes from curative to palliative care.
The direction of care can be refocused toward promoting comfort, optimizing the treatment of pain and anxiety, and striving for closure for grieving family members. Specific treatment options need to be considered, such as ventilator support use (or avoidance). Typically, oxygen and intermittent non-invasive ventilation (NIV) may be an option, but not intubation and invasive ventilation, CPR, hemodialysis, ECMO, or transfer to an AICU/PICU. Care in a hospice context could be considered.
In Sweden, it is of paramount importance that the discussions and agreements reached are documented in the patient journal and that complete transparency is established regarding the family members and all involved in the care of the young patient. The medical team must build confidence between the clinicians and the patient’s family, even when they do not reach the same decision regarding the imposition of LOMT. In addition, in the Swedish PICU context, it must be communicated to family members and staff that the clinicians and not the family have the right to make a formal decision concerning LOMT. However, a LOMT order does not exclude care in an ICU, as already reported for adult ICU patients [24]. We see the same pattern in the present study, in which 60 (41%) patients dying in a PICU had LOMT orders in place. This illustrates an increasing element of ‘managed death’ in a modern ICU, in which the staff and family have some influence in the details of stepping down or not increasing the intensity of care. This PICU palliation is, in some cases, the only way to manage a patient, especially when hospice care is not available. The goal for medical care at the end of life can be similar over different specialties. Duska and colleagues expressed this concept in a way that also holds for PICU care: “Our ultimate goal is not cancer treatment until death; it is the preservation of quality of life, dignity, and individual patient goals of life whenever possible” [25].
For children discharged from a PICU who are suffering from a severe and potentially incurable illness, addressing the situation and forming a LOMT decision are essential steps in reaching these goals. A young doctor on call cannot make this decision at 2 AM when a patient arrives in the emergency department. They will have to initiate non-limited PICU care if there is no LOMT in place. Therefore, the absence of a LOMT can pose considerable consequences for a patient and their relatives.
Statistical considerations with death as an endpoint
The observed findings may be a starting point for questioning the meaningfulness of continuing to use mortality as an index of the quality of ICU care. We maintain that the emerging death of a child is unlikely to degenerate into a practical or economically determined event in the face of overwhelming concern over resource waste about care for patients with a poor long-term prognosis or perceived poor quality of life. Long before, it was stated that physicians are responsible for recognizing the limits of critical care and preventing undue suffering [26-28]. Thus, in our practice, the appearance of a managed death scenario in pediatrics should be viewed as an attempt to defend human dignity and prevent meaningless suffering for family members and patients once the possibility of returning to life is no longer present.
Since these deliberations and decisions must take place in full view of patients’ family members and the public, they need to be handled professionally by experienced, stable teams. We argue further that these needs demand the centralization of terminally ill children in tertiary clinics where at least a minimum of facilities and subspecialties are represented. This will also provide more accumulated experience in managing these delicate cases, as the level of care can be discussed at an optimal point. Otherwise, unwanted emotional and legal complications might arise despite the best efforts in a particular setting.
Limitations
Firstly, the legacy of LOMT varies with cultural traditions and access to health care. Thus, the external validity of our data might need to be stronger. Secondly, the documentation of this decision must be available in the patient’s records to make an evaluation possible. A lack of access to such documents could lead to other conclusions and findings. Furthermore, the proportion of LOMT orders found was likely still underestimated, as a verbally expressed LOMT decision may have been implemented close to the time of some patients’ deaths but never documented in their charts.
Although publications from PICU s in developed countries show a similar pattern of LOMT tradition, as we have reported, we need to bear in mind that these are Swedish data that should be interpreted as such. Over 50% of children in need of ICU care in Sweden are treated in an adult ICU (AICU), as the number of PICU beds nationally has remained low compared to other developed countries [3]. We have no data for these children, as care received in the AICU was not part of this study. We did not find any documented information pointing to the lack of access to a PICU bed as the reason for a child not being readmitted to the PICU.
Strengths
Our study covers all children admitted to PICU care in a single western country over a 3-year, with a median follow-up time of 2.5 years. Only a few (about 5%) patients were lost to follow-up. A total of 268 deaths were documented, and detailed patient records with LOMT status and place of death could be found for 252 (94%) of these events.
Conclusion
Most children (75%) who die outside a PICU after PICU discharge have a LOMT recorded limiting readmission to the PICU.
Abbreviations
AICU: Adult intensive care unit
ANZPIC: Australian and New Zealand Paediatric Intensive Care
CCC: complex chronic conditions
CPR: cardiopulmonary resuscitation
ECMO: extracorporeal membrane oxygenation
IQR: interquartile range
LOMT: limitation of medical treatment
NIV: non-invasive ventilation
PICU: paediatric intensive care unit
Acknowledgement
For collecting complementary patient data, we would like to express our gratitude to the following:
Dr. Johannes Bengner, Barn-och ungdomsmedicinska kliniken, Länssjukhuset Ryhov,
Dr. Per Friskopp Barn-och ungdomsmedicin, Barnkliniken, Gällivare sjukhus
Dr. Isabelle Karlsson, Neonatal avdelningen Sunderbyns sjukhus
Dr. Erik Normann, Uppsala Akademiska Barnsjukhus
Finance:
Financial support was provided to Staffan Eksborg through the regional agreement on medical training and clinical research (ALF), project 20150224, between Stockholm County Council and the Karolinska Institutet. C Frostell Research and Consulting AB provided an unrestricted educational grant for printing and editing. The remaining authors did not receive any financial support.
Conflicts Of Interest
The authors have no conflicts of interest to declare.
References
- Garros D, Rosychuk RJ, Cox PN (2003) Circumstances surrounding end of life in a pediatric intensive care unit. Pediatrics. 112(5): e371-9.
- Kalzén H, Larsson B, Eksborg S, Lindberg L, Edberg KE, et al. (2018) Survival after PICU admission: The impact of multiple admissions and complex chronic conditions. PLoS One. 13(4): e0193294.
- Gullberg N, Kalzén H, Luhr O, Göthberg S, Winsö O, et al. (2008) Immediate and 5-year cumulative outcome after paediatric intensive care in Sweden. Acta Anaesthesiol Scand. 52(8): 1086- 95.
- Moore P, Kerridge I, Gillis J, Jacobe S, Isaacs D (2008) Withdrawal and limitation of life-sustaining treatments in a paediatric intensive care unit and review of the literature. J Paediatr Child Health. 44(7-8): 404-8.
- Mink RB, Pollack MM (1992) Resuscitation and withdrawal of therapy in pediatric intensive care. Pediatric. 89(5): 961-3.
- Lantos JD, Berger AC, Zucker AR (1993) Do-not-resuscitate orders in a children's hospital. Crit Care Med. 21(1): 52-5.
- Vernon DD, Dean JM, Timmons OD, Banner W Jr, Allen-Webb EM (1993) Modes of death in the pediatric intensive care unit: withdrawal and limitation of supportive care. Crit Care Med. 21(11): 1798-802.
- Ryan CA, Byrne P, Kuhn S, Tyebkhan J (1993) No resuscitation and withdrawal of therapy in a neonatal and a pediatric intensive care unit in Canada. J Pediatr. 123(4): 534-8.
- Balfour-Lynn IM, Tasker RC (1996) At the coalface - medical ethics in practice. Futility and death in paediatric medical intensive care. J Med Ethics. 22(5): 279-81.
- Martinot A, Grandbastien B, Leteurtre S, Duhamel A, Leclerc F ( 1998) No resuscitation orders and withdrawal of therapy in French paediatric intensive care units. Groupe Francophone de Réanimation et d'Urgences Pédiatriques. Acta Paediatr. 87(7): 769-73.
- van der Wal ME, Renfurm LN, van Vught AJ, Gemke RJ (1999) Circumstances of dying in hospitalized children. Eur J Pediatr. 158: 560-5.
- Devictor DJ, Nguyen DT (2001) Forgoing life-sustaining treatments: How the decision is made in French pediatric intensive care units. Crit Care Med. 29(7): 1356-9.
- Goh AY, Mok Q (2001) Identifying futility in a paediatric critical care setting: a prospective observational study. Arch Dis Child. 84: 265-268.
- Althabe M, Cardigni G, Vassallo JC, Allende D, Berrueta M, et al. (2003) Dying in the intensive care unit: collaborative multicenter study about forgoing life-sustaining treatment in Argentine pediatric intensive care units. Pediatr Crit Care Med. 4(2): 164-9.
- Devictor DJ, Nguyen DT (2004) Forgoing life-sustaining treatments in children: a comparison between Northern and Southern European pediatric intensive care units. Pediatr Crit Care Med. 5(3): 211-5.
- Zawistowski CA, DeVita MA (2004) A descriptive study of children dying in the pediatric intensive care unit after withdrawal of life-sustaining treatment. Pediatr Crit Care Med. 5(3): 216-23.
- Kipper DJ, Piva JP, Garcia PC, Einloft PR, Bruno F, et al. (2005) Evolution of the medical practices and modes of death on pediatric intensive care units in southern Brazil. Pediatr Crit Care Med. 6(3): 258-63.
- Lago PM, Piva J, Kipper D, Garcia PC, Pretto C, et al. (2005) Life support limitation at three pediatric intensive care units in southern Brazil. J Pediatr (Rio J). 81(2): 111-7.
- Siddiqui NU, Ashraf Z, Jurair H, Haque A (2015) Mortality patterns among critically ill children in a Pediatric Intensive Care Unit of a developing country. Indian J Crit Care Med. 19(3): 147- 50.
- Devictor DJ, Latour JM (2011) Forgoing life support: how the decision is made in European pediatric intensive care units. Intensive Care Med. 37: 1881-7.
- Edwards JD, Houtrow AJ, Vasilevskis EE, Rehm RS, Markovitz BP, et al. (2012) Chronic conditions among children admitted to U.S. pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay. Crit Care Med. 40(7): 2196-203.
- Feudtner C, Christakis DA, Connell FA (2000) Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 106(1 Pt 2): 205-9.
- Slater A, Shann F, McEniery J; ANICS Study Group (2003) The ANZPIC registry diagnostic codes: a system for coding reasons for admitting children to intensive care. Intensive Care Med. 29: 271-7.
- Jäderling G, Bell M, Martling CR, Ekbom A, Konrad D (2013) Limitations of medical treatment among patients attended by the rapid response team. Acta Anaesthesiol Scand. 57(10): 1268-74.
- Duska LR (2015) Acknowledging the limitations of treatment: surrendering to reality. Oncologist. 20(8): 854-5.
- Tilford JM, Fiser DH (1996) Futile care in the pediatric intensive care unit: ethical and economic considerations. J Pediatr. 128(6): 725-7.
- Levetown M, Pollack MM, Cuerdon TT, Ruttimann UE, Glover JJ (1994) Limitations and withdrawals of medical intervention in pediatric critical care. JAMA. 272(16): 1271-5.
- Schaffner KF, Snyder JV, Abramson NS, Bar-Joseph G, D'Alecy LG, et al. (1988) Philosophical, ethical, and legal aspects of resuscitation medicine. III. Discussion. Crit Care Med. 16(10): 1069-76.