Ilona Tserediani*
Ivane Javakhishvili Tbilisi State University, Faculty of Medicine, Georgia, Tbilisi
Clinic ‘Vivamedi’ Ophthalmology Department, Georgia, Tbilisi
*Corresponding Author: Ilona Tserediani, Ivane Javakhishvili Tbilisi State University, Faculty of Medicine, Georgia, Tbilisi.
Abstract
Myopia represents the most prevalent form of refractive anomaly. Myopia represents a significant global health concern, with a marked increase in prevalence over the past decade. Notwithstanding the considerable advances made in the investigation of myopia etiology, progressive and complex myopia continues to represent a significant cause of blindness and low vision. It accounts for 35–44% of all cases of visual disability. The medical and social significance of progressive myopia is determined by the impact it has on visual disability, restriction of professional choice, and a sharp decrease or complete loss of working capacity at a young, still able-bodied age. Among the complications associated with myopia, particular attention is given to dystrophy, detachment, and other retinal changes. Prevention and treatment of these complications are of significant importance. In light of the aforementioned, prevention of myopia and its associated complications represents a crucial step in addressing significant social issues. Biomechanical and hemodynamic factors are of primary importance in the pathogenesis of myopia and the progression of myopic chorioretinal dystrophy. The weakening of the scleral capsule, which can be caused by a number of different factors, leads to a stretching of the sclera and an elongation of the anteroposterior axis of the eye. This has a negative impact on the sclera and the retina, which are less plastic than the sclera. In these circumstances, myopia is not merely a refractive anomaly; it is a myopic disease that is accompanied by functional and morphological complications. The objective of this study is to ascertain the residual deformation of the sclera in the 'reading mode.'
The material and methodology employed in the research project are presented herewith. The study has been ongoing since 2016. A total of 250 patients were examined. The patients were stratified into three groups according to age and degree of myopia. In addition to the standard ophthalmological examinations, the patients underwent further examination. Ultrasound biometry utilising an A-scan in 'reading mode'. The results demonstrated a significant increase in the size of the eye in all three groups. In the first group, the eyeball exhibited an increase of 93% in 'reading mode'. In the second group, the eye demonstrated an increase of 91%. Similarly, in the third group, the eye exhibited an increase of 91.5%. The stretching of the sclera capsule in 'reading mode' is caused by the impact of the extraocular muscles and the increase in intraocular pressure. The stretching of the sclera, which results in residual deformations caused by squeezing, can be considered a trigger mechanism for the progression of myopia.
The results of the study revealed that in children, near-vision strain causes scleral tension, deformation of the scleral capsule, elongation of the eye's APO, and, consequently, the development of myopic disease. Based on the data obtained throughout the course of this study, we recommend that the results be used as a foundation for the implementation of prophylactic measures, the administration of medication, or other forms of therapy.
Keywords: Myopia, A-scan, Progressive Myopia, Myopia control, Ultrasound biometry, stretching of the sclera.
Introduction and Relevance
Myopia is the most common refractive anomaly. Near-sightedness has become one of the main public health problems worldwide, with its prevalence sharply increasing over the past decade [17].
Despite significant advances in the study of the pathogenesis of myopia, progressive and complicated myopia remains one of the leading causes of blindness and low vision; its share in the structure of visual disability accounts for 35-44% [2].
The medical and social significance of progressive myopia is determined by the impact on visual disability, restriction of professional choice, and a sharp decrease or complete loss of working capacity at a young, still able-bodied age [5].
Among the problems associated with myopia, particular attention is paid to complications such as dystrophy, detachment, and other retinal changes, as well as issues related to their prevention and treatment. In light of the above, the prevention of myopia development and its accompanying complications is aimed at resolving significant social issues [1].
Biomechanical and hemodynamic factors play a leading role in the pathogenesis of myopia progression and myopic chorioretinal dystrophy [1].
The weakening of the scleral capsule under the influence of various endogenous and exogenous factors is accompanied by a tendency for the sclera to stretch, with an elongation of the anteroposterior axis of the eyeball, which negatively affects the state of the retina and choroid, which are less plastic than the sclera. Under these conditions, myopia is not a refractive anomaly, but a myopic disease accompanied by functional and morphological complications [1].
Refractive anomalies of the eye depend not so much on the power of optical lenses as on the length of the eyeball. In hyperopia, the anteroposterior axis of the eye is shorter, and in myopia, it is longer. Normally, a person is born with hyperopic refraction. Then, throughout childhood and adolescence, the eyeball lengthens slightly, which is accompanied by the disappearance of hyperopia. The maximum decrease is observed in the first year of life. As age progresses, eye growth slows down and eventually stops in adulthood [7,8].
The growth of eyes in individuals occurs differently. With the rapid growth of the eyeball, the decrease in hyperopia occurs faster, and if hyperopia completely disappears during childhood, further growth of the eyeball leads to the development of myopia. In adulthood, the progression of myopia slows down and stops in the vast majority of cases.
The earlier myopia develops, the stronger it becomes, as there is more time for the eyeball to grow. Myopia is more common in individuals with excessive visual strain during childhood and adolescence. Hereditary predisposition to myopia plays a significant role, but it is difficult to determine its extent, as children often inherit not only genes but also lifestyle from their parents.
The aim of the study was to determine residual deformations of the sclera when gazing medially-downward in reading mode.
Global Prevalence:
Asia:
Myopia rates are particularly high in East Asia, with countries like China, Japan, and South Korea reporting prevalence rates of 60% to 90% among young adults.
Europe and North America:
Prevalence rates range from 30% to 50% among young adults, but they are rising.
Africa and Australia:
Generally lower prevalence, though increasing in urban areas. In Africa, the prevalence is still under 10%, but it is rising in cities.
Age Factor:
Myopia often starts in childhood and progresses during school years, stabilizing in early adulthood. By age 18-24, many have already reached their final refractive error.
Urban vs. Rural:
Higher rates are observed in urban areas compared to rural regions, suggesting a correlation with lifestyle factors such as education and screen time.
Forecast:
By 2050, it is estimated that nearly 50% of the world's population will be myopic due to factors like increased near work, reduced time spent outdoors, and rising educational demands.
Etiology (Causes) of Myopia
The development of myopia involves both genetic and environmental factors.
Genetic Factors:
Heritability:
Myopia is highly heritable, with children of myopic parents having a significantly higher risk of developing the condition. Multiple genes are involved in eye growth and refractive development.
Single Nucleotide Polymorphisms (SNPs):
Recent studies have identified several genetic loci linked to myopia susceptibility, though no single gene has been found to cause myopia.
Environmental Factors:
Near Work Activities:
Prolonged activities that involve focusing on close objects, such as reading, using computers, and smartphones, have been associated with myopia development. However, no conclusive evidence links near work directly as a sole cause.
Lack of Outdoor Time:
Insufficient exposure to natural daylight is a significant environmental risk factor. Time spent outdoors during childhood is inversely correlated with myopia onset and progression, possibly due to the influence of light on eye growth and dopamine release.
Education:
Higher levels of education, which typically involve more near work, are associated with increased rates of myopia.
Other Risk Factors:
Urbanization:
Myopia rates are higher in urbanized societies, which may be linked to lifestyle changes such as increased indoor activities and less outdoor exposure.
Socioeconomic Status:
Higher socioeconomic groups often have higher myopia prevalence, possibly due to more intense academic environments.
Nutrition:
Although not a major factor, some studies suggest that a lack of specific nutrients involved in eye development may play a role, but this is still under investigation.
Myopia is a complex condition influenced by an interplay of genetic predispositions and modern environmental factors, with significant public health implications.
Materials and Methods
A total of 250 patients were examined, divided into three groups depending on age: Group I - 90 patients aged 5 to 19 years, Group II- 80 patients aged 13 to 19 years, Group III - 80 patients aged 19 years and older. All examined patients had varying degrees of myopia. The age criteria used in the study were based on the anatomical development of the eyeball. Normally, the eye size at the age of 5-12 years varies between 20.5 mm and 23 mm; from 13 to 18 years - 23-24 mm, from 19 years - 24.5 to 24.9 mm, with a tolerance of ± 0.5 mm [6-10].
In addition to standard ophthalmological examinations, the patients underwent ultrasound biometry of the eyeball [Alcon. A-scan]. It is planned to repeat the above-mentioned examinations over a period of 3 years.
Ultrasound biometry was conducted as follows: for each patient, the surface of the ultrasound probe was brought into contact with the same point on the equator in three positions of the eyeball: the anteroposterior axis of the eye (APO), the length of the APO during medial gaze, and during medial-inward gaze (reading mode).** **
Results and Discussion
The analysis of the data obtained from the studies revealed that in all age groups, there is an elongation of the APO of the eyes in reading mode due to scleral stretching. During convergence, accompanied by an increase in intraocular pressure (IOP), the scleral contour stretches toward the posterior pole, resulting in an ellipsoidal shape of the posterior hemisphere of the eyeball. This shape becomes fixed in eyes with axial myopia after the appearance of residual scleral deformations [1]. Scleral thinning associated with myopia may reduce the tolerance of the sclera and optic nerve to elevated IOP, further inducing axial elongation of the sclera and causing optic nerve damage [1-17].
With weakened accommodative ability, intensive visual work at close distances becomes an overwhelming burden for the eyes, leading to an elongation of the eye's APO. Furthermore, once the posterior pole of the eye takes on a more convex shape, it becomes the point of least resistance [1].
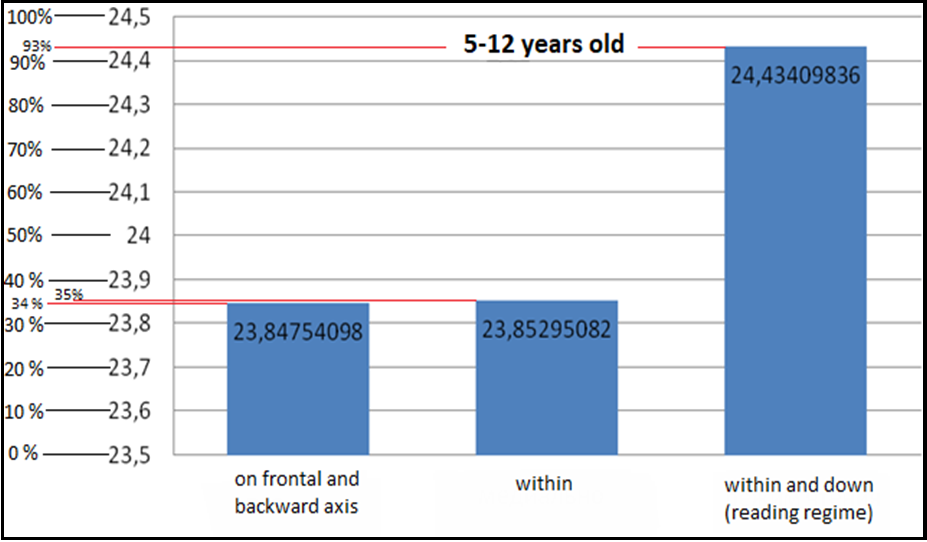
The results of ultrasound biometry of the eyeball are presented in Diagrams 1-3.
Diagram 1: Ultrasound Biometry Data for Patients Aged 5 to 12 Years (Average Values)
Diagram 1 presents data from 90 patients (180 eyes) aged 5 to 12 years. The results show that in this age group, 93% of the subjects exhibited elongation of the scleral capsule in reading mode.
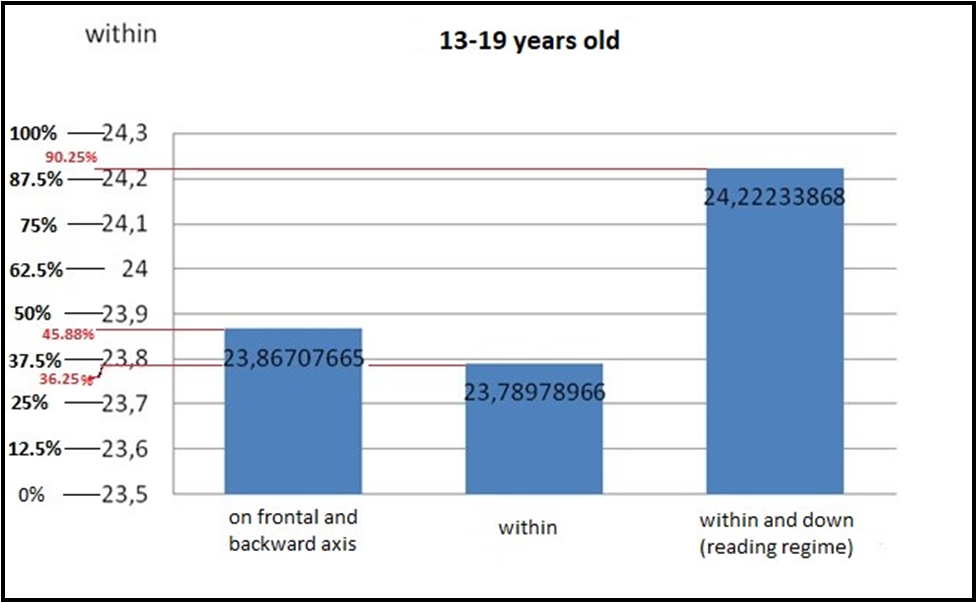
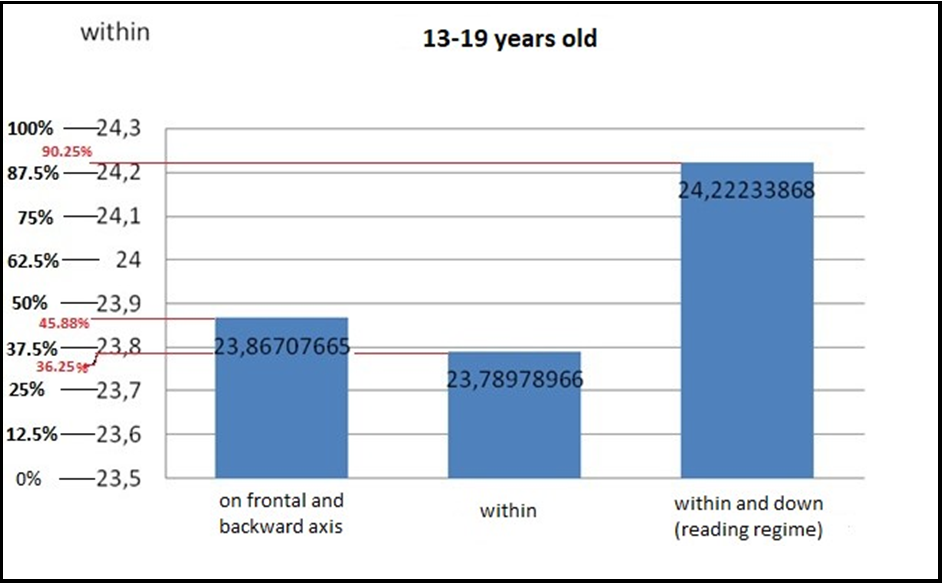
Diagram 2: Ultrasound Biometry Data for Patients Aged 13 to 19 Years (Average Values) Diagram 2 presents data from 80 patients (160 eyes) aged 13 to 19 years.
The results show that in this age group, 90.25% of the subjects exhibited elongation of the scleral capsule in reading mode.
Diagram 3: Ultrasound Biometry Data for Patients Aged 19 Years and Older (Average Values)
The data presented in Diagram 3 indicates that among those aged 19 years and older, 91.5% of the subjects exhibited elongation of the scleral capsule in reading mode.
Over the past decade, myopia has become more common in adolescence and preschool age. Among children, myopic refraction accounts for nearly 80% [24,25]. The decrease in vision accompanying progressive myopia complicates the perception of visual information and reduces work potential. According to the modern understanding of the genesis of myopia, the leading risk factors for its development are: a) a sedentary lifestyle; b) improper diet; c) an increase in viral and infectious diseases; d) an increase in time spent at the computer [17].
This acceleration of the problem's trend necessitates a thorough study of the pathogenesis of this pathology. The results of the study revealed that in children, near-vision strain causes scleral tension, deformation of the scleral capsule, elongation of the eye’s APO, and, consequently, the development of myopic disease.
Given the aforementioned genesis factors, improved scleral trophism will likely enhance the plasticity of the sclera, which in turn reduces the likelihood of accumulating residual deformations of the scleral capsule and significantly lowers the risk of developing myopia.
Based on the data obtained during the study, we recommend using the study results as a basis for preventive measures, medication, or other forms of therapy. Ongoing research already provided some insights into molecular pathways underlying myopia and could be expected that it will soon produce new drug targets and drugs for treatment of myopia.
References
- Avetisov, E.S. Myopia (1999) Medicine.
- Aminova, Z.M. Information Support for the Problems of Childhood Disability. Public Health and Healthcare.
- Kim MH, Zhao D, Kim W, Lim DH, Song YM, et al. (2013) Heritability of myopia and ocular biometrics in Koreans: the Healthy Twin Study. Investigative Ophthalmology & Visual Science. 54(5): 3644-9.
- Kim MH, Zhao D, Kim W, Lim DH, Song YM, et al. (2013) Heritability of myopia and ocular biometrics in Koreans: the Healthy Twin Study. Investigative Ophthalmology & Visual Science. 54(5): 3644-9.
- Konovalova A.B (2007) Hygienic Assessment of Environmental Factors’ Influence on the Prevalence of Eye Diseases and its Adnexa among the Pediatric Population. Healthcare of the Russian Federation.
- Nefedovskaya L.V (2008) Myopia in Children as a Medical and Social Problem. Russian Pediatric Journal.
- Nefedovskaya, L.V (2008) Prevention of Vision Impairment in School-Aged Children. Pediatric Reference. - № 7
- Jiang BC, Schatz S, Seger K (2005) Myopic Progression and Dark Focus Variation in Optometry Students during the First Academic Year. Clinical and Experimental Optometry. 88(3): 153-9.
- Saw SM, Tong L, Chua WH, Chia KS, Koh D, et al. (2005) Incidence and Progression of Myopia in Singaporean School Children. Investigative Ophthalmology & Visual Science. 46(1): 51-7.
- Morgan I, Rose K (2005) How Genetic is School Myopia?. Progress in Retinal and Eye Research. 24(1): 1-38.
- Siatkowski RM, Cotter S, Miller JM, Scher CA, Crockett RS, et al. (2004) Safety and Efficacy of 2% Pirenzepine Ophthalmic Gel in Children with Myopia: A 1-Year, Multicenter, Double- Masked, Placebo-Controlled Parallel Study. Archives of Ophthalmology. 122(11): 1667-74.
- Schultz N (2009) Generation Specs: Stopping the Short-Sight Epidemic. New Scientist.
- Guggenheim JA, Hill C, Yam TF (2003) Myopia, Genetics, and Ambient Lighting at Night in a UK Sample. British Journal of Ophthalmology. 87(5): 580-582.
- Kemper AR, Wallace DK, Zhang X, Patel N, Crews JE, et al. (2012) Uncorrected Distance Visual Impairment among Adolescents in the United States. Journal of Adolescent Health. 50(6): 645–647.
- McBrien N.A, Arumugam B, Gentle A, Chow A, Sahebjada S (2011) The M4 Muscarinic Antagonist MT-3 Inhibits Myopia in Chick: Evidence for Site of Action. Ophthalmic and Physiological Optics. 31(5): 529-39.
- Morgan IG, Ohno-Matsui K, Saw SM (2012) Myopia. Lancet. 379(9827): 1739-48.
- Foster P.J, Jiang Y (2014) Epidemiology of Myopia. Eye (London). 28(2): 202–208.
- Mirshahi A, Ponto KA, Höhn R, Wild PS, Pfeiffer N (2013) Ophthalmological Aspects of the Gutenberg Health Study (GHS): An Interdisciplinary Prospective Population-Based Cohort Study. Ophthalmologe. 110(3): 210–217.
- Pan CW, Ramamurthy D, Saw SM (2012) Worldwide Prevalence and Risk Factors for Myopia. Ophthalmic and Physiological Optics. 32: 3–16.
- Smith EL 3rd, Hung LF, Huang J (2012) Protective Effects of High Ambient Lighting on the Development of Form-Deprivation Myopia in Rhesus Monkeys. Investigative Ophthalmology & Visual Science. 53(1): 421–428.
- Mutti D.O, Marks A.R (2011) Blood Levels of Vitamin D in Teens and Young Adults with Myopia. Optometry and Vision Science. 88(3): 377-82.
- Mutti DO, Cooper ME, Dragan E, Jones-Jordan LA, Bailey MD, et al. (2011) Vitamin D Receptor (VDR) and Group-Specific Component (GC, Vitamin D-Binding Protein) Polymorphisms in Myopia. Invest Ophthalmol Vis Sci. 52(6): 3818-24.
- Li, Y.J., Goh, L., Khor, C.C. et al. Genome-Wide Association Studies.