Tsujimura S, Kwong Hing A*, Hamblin MR
PBM Healing International Ltd Unit 23/D, Sun Ying Industrial Center, 9 Tin Wan Close Aberdeen, Hong Kong, HKSAR
*Corresponding Author: Alan Kwong Hing, PBM Healing International Ltd Unit 23/D, Sun Ying Industrial Center, 9 Tin Wan Close Aberdeen, Hong Kong, HKSAR
Abstract
Orthognathic surgery can correct irregularities of the jaw bones; improve the way the jaws and teeth function and facial and tooth esthetics can be enhanced to be more esthetically pleasing for the patient.
Prior to and after corrective jaw surgery, orthodontic treatment will be completed to enhance the function and esthetics of the teeth. The successful use of Photobiomodulation to overcome post-operative pain and accelerate healing with orthognathic surgery is presented in this case report.
Introduction
Many human body parts undergo development with bilateral symmetry. However, due to biological factors inherent to processes of development as well as environmental disturbances, perfect bilateral symmetry is rarely found [1].
The face often presents with a mild degree of asymmetry. Nevertheless, slight asymmetry, also known as relative symmetry, subclinical asymmetry or normal asymmetry, ends up being unperceived by its carriers and everyone around them. It derives from the fact that the lower and midface develop from the medial and lateral nasal processes as well as maxillary and mandibular processes, and despite being intrinsically coordinated, these structures might imply failure of development or maturation of such embryonic processes [2].
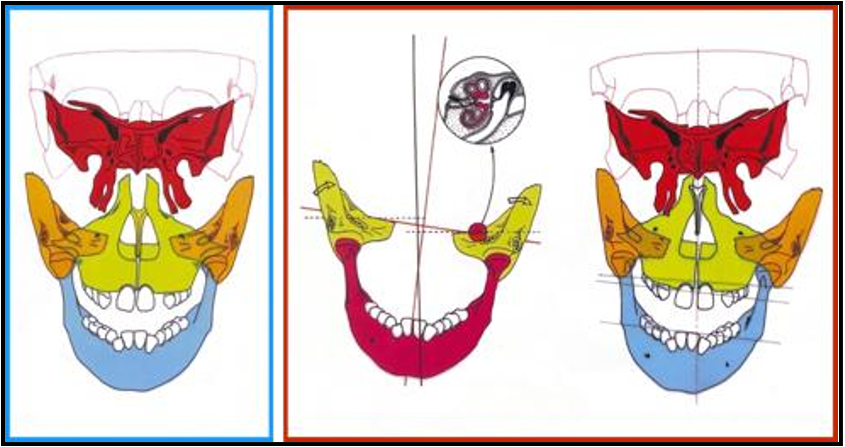
The etiology of facial asymmetry can be divided into three components: congenital, developmental and acquired [3, 4]. Facial asymmetry may be present along with Class I or Class II malocclusions, but it most commonly occurs in cases with Class III malocclusions [5, 6].
Depending on the craniofacial structures involved, facial asymmetry can be classified into - skeletal, dental and functional. Dental factors mainly include early loss of deciduous tooth, congenital missing tooth or teeth, and certain habits. Skeletal asymmetry may involve either one or more bones. Functional asymmetry may result because of deviation of the mandible due to tooth interferences. Most often there is more than one contributing factor. [7]
In a recent study, an Oral and Maxillofacial Surgery (OMFS) research team at the Faculty of Dentistry of the University of Hong Kong (HKU) revealed that jaw asymmetry is likely to be a causative factor of jaw joint pain, and that surgical correction of facial asymmetry is effective in improving or even curing patients suffering from jaw joint pain. Patients with facial asymmetry will see a difference in the length of the left and right side of the jaws, which results in a deviated face as well as a shifted bite. The asymmetric face not only affects the facial appearance of the individual but also hinders the eating or speech function and lowers the patient's self-esteem [8].
Photobiomodulation
One of the mechanisms thought to be responsible for the physiological effects of Photobiomodulation (PBM), is the absorption of light photons by cytochrome c oxidase in the mitochondrial respiratory chain, leading to changes in cellular metabolism. As a result of this stimulation, production of the intracellular energy source, adenosine triphosphate (ATP) is increased. It is postulated that more ATP allows for increased function and metabolism of cells in tissues that are ischemic, damaged, affected by toxins, or at risk of death. [9]
LEDs have many advantages over lasers for use in PBM, including a much larger irradiation area due to the use of LED arrays, more accessible hardware package, and a lower power density with no safety concerns. [10]. Recent experiments utilizing LED PBM have shown a similar therapeutic effect as low-level laser PBM [11]. Animal studies have shown the ability of PBM to accelerate the healing of autologous [12] and xenograft [13] bone grafts in rat skull surgical defects.
PBM Implant device The intraoral photobiomodulation LED device used in this case was PBM Implant manufactured by PBM Healing International (PBM Group of Companies, Hong Kong). (Figure 1)
Figure 1: PBM Implant device untilized in the treatment of the case report patient
PBM Implant LED mouthpiece description and parameters Power Input: 2.1 V
LED Cores: 46
Wavelength: 625 nm
Current for each LED Core: 30 mAmp
Energy Absorbed over 6 minutes per arch: 130 Joules per segment The PBM Implant device has an alignment system that allows the patient to position and fix the array as needed over the relevant surgical site in the mouth. An external battery powers the device. The PBM Implant is programmed to deliver the prescribed PBM regimen every time it is used for 6 minutes. The surgical site is treated three times per day for the first two weeks post op and then 1x per day until healing has occurred, the device has been designed for one user only and to allow the patient to easily treat themselves at home.
Advantages of using PBM therapy include: Decreased pain associated with surgery Improved bone grafting consolidation Enhanced implant stability.
Maximize the individual biology to enhance healing
Maintain long-term soft and hard tissue health
Works with any implant system or bone grafting material
The overall orthognathic surgery process is complicated and is a team effort by the general dentist, oral and maxillofacial surgeon in collaboration with an orthodontist. The surgery has considerable risks including blood loss, infection, nerve injury, jaw fracture, relapses of the jaw to the original position, problems with bite fit and jaw joint pain, need for further surgery, root canal therapy on selected teeth and loss of a portion of the jaw.
After surgery there is significant pain and swelling, problems with eating, adjustment to a new facial appearance and a lengthy period for healing and recovery for up to 3 - 4 months [14]
Case Presentation
A 17 -year-old female patient reported for orthodontic treatment as a prelude to jaw surgery to correct a lower jaw asymmetry. There was a chief complaint of asymmetric jaw relationship and in addition irregular teeth position, jaw clicking and an unesthetic smile due to the crooked jaw. (Figure 2 and 3)
Figure 2: Extraoral preop photos demonstrating asymmetric jaw and tooth positioning
Figure 3: Intraoral symmetric smile preop photos
Patients had a leptoproscopic facial type with mandibular asymmetry. Facial profile was convex with retrusive chin position and high clinical FMA. Intraoral findings showed Class II subdivision right malocclusion with good alignment of upper and lower anteriors, and a lower midline deviation of 3 mm to right.
There was a bilateral open bite. The patient was first treated with aligners to correct the tooth and jaw discrepancy, but this was not successful, therefore she elected to have jaw surgery as well as pre surgical fixed orthodontics to finalize the detailing of the teeth positioning for surgical repositioning. (Figure4)
Figure 4: Initial treatment with aligners
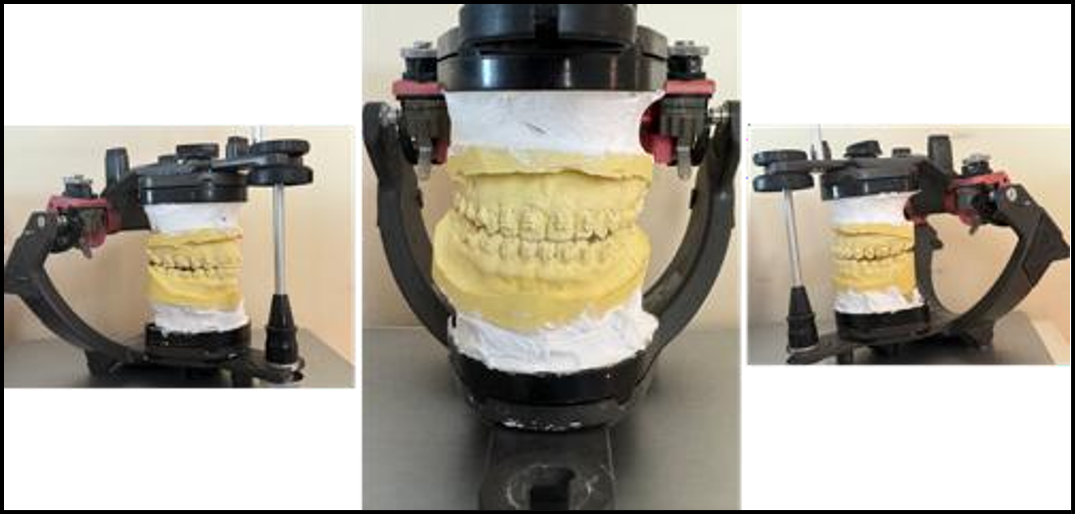
Full medical and dental records were taken and no contraindications to the planned orthognathic surgery and use of the PBM Implant photobiomodulation device were noted. Contraindications to the use of the PBM Implant device include pregnancy and light sensitivity. Diagnostic records, including extraoral radiographs, lateral cephalogram, Panoramic, CT scan, photographs and study models were taken. In addition, two cephalographs with postero-anterior (PA) view in centric occlusion and open mouth position were taken to differentiate between skeletal and dental asymmetry.face bow transfer was recorded on the patient and transferred onto the articulator to evaluate the midline shift. (Figure 5)
Figure 5: Mid treatment mounted models using facebow transfer and records with fixed orthodontics in plave
Findings
Photographic analysis revealed non-coinciding midlines with deviation of the chin towards the right. An open bite was noted bilaterally and a Class II molar relationship.
Panoramic radiograph showed that the condyle of the left side was slightly larger than the right side, suggesting mild hyperplasia of the left condyle.
The lateral cephalometric tracing showed a good anteroposterior skeletal relationship with a vertical growth pattern.
Face bow transfer indicated the presence of skeletal midline shift, which was confirmed with the radiographic analysis of PA view cephalograms in occlusion and in open mouth position.
The analysis of the patient’s facial asymmetry and her desire for a better esthetic and functional result confirmed a surgical correction of the facial asymmetry to be completed. (Figure 6) She had a small click of the joint on opening on the right side TMJ joint which was not painful. In addition, enhanced surgical healing of the bone, decreased overall post operative pain and inflammation were to be achieved with the use of Intraoral photobiomodulation as delivered by the PBM Implant device.
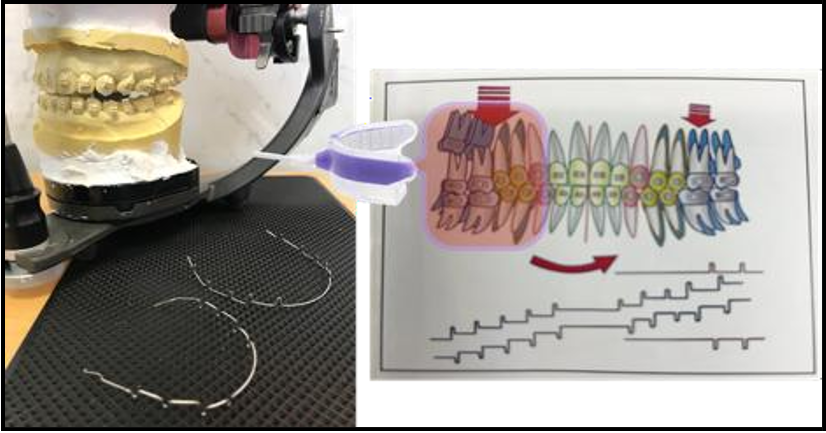
Pretreatment orthodontics completed with fixed orthodontics. Significant improvement was observed in the patient's dental esthetics including alignment of upper and lower anteriors, however she still had an open bite and Class II molar relationship. (Figure 7)
Figure 7: Pretreatment photographs
Fixed orthodontics to finalize aligment of the teeth. (Figure 8 and 9) When the teeth were in the correct orientation for the orthognathic surgery her screening was completed and her surgery scheduled. The fixed braces were left intact for use in securing the jaws after the surgery.
Figure 8 & 9: Preoperative surgical fixed orthodontic treatment
Surgical correction of the mandibular aysemmetry was completed uneventfully and the patient was provided immediately after surgery with a PBM Implant device (Figure 10) to use for controlling post operative pain and swelling and to enhance bone healing. Post- operative surgical healing instructions were given to the patient along with instructions for the use of the PBM Implant device.
Figure 10: Intraoral use of the PBM Implant with illumination of the soft tissues by red light.
General Recommendations for use of the PBM Implant device include:
Deliver the PBM Implant device to the patient prior to completing any procedure and instruct them on how to use it for their specific treatment area.
The patient should bring their PBM Implant device with them to all appointments.
Prior to starting any procedure, which may cause pain, the patient should use their PBM Implant device for a 6-minute treatment session using full arch treatment mode. For example, prior to giving local anesthetic for any procedure, the patient should use their device.
After any procedure is completed, the patient should immediately use their device for a 6-minute treatment period, either in the office or on their way home.
The best time to use the device is at the same time each day when the patient can sit still for the 6-minute treatment period, for example while commuting to work.
The device should be used 3 x per day, but there should be 8 hours between treatments as overuse will impede the biological healing process. This increased frequency is only recommended for the first 2 weeks after treatment.
Post-operative medications including an antibiotic and anti- inflammatory were given to the patient. She was asked to report back after 1 week for a post-surgical check. Post operatively the patient was also asked to complete a VAS form to record the levels of pain and medication use.
She noted minimal pain with a rating of 2 after the surgery and almost zero after 2 days of PBM Implant usage. More importantly as she did not have significant pain, she did not use any analgesic medications despite undergoing extensive surgery. In addition, in this case, despite a significant change in jaw position, the treatment was completed without complaints of maladjustment or pain including temporomandibular joint pain, which was an effect of the PBM treatment. The patient continued to use the PBM Implant device for the healing period of 6 weeks and did not have any significant pain or discomfort. It was estimated the healing time for her was shortened by at least 1/3. However, as this was an initial case the timelines were not refined. In addition, her jaw click resolved after the surgery. Subsequent cases and monitoring of healing will allow for more accurate estimation of decreased healing time. However, the lack of pain and swelling was a sufficient reason for the patient to use the PBM Implant device. The result of meticulous diagnosis, treatment planning and surgery with the PBM Implant device adjunctively for pain relief resulted in a pleasing aesthetic result and non-traumatic surgical course of treatment. The patient was extremely happy with her results (Figure 11 and 12)
Figure 11: Post operative intraoral photo showing nice alignment of the teeth
Figure 12: Post operative photo showing correction of the jaw asymmetry and alignment of the teeth
Discussion
True dental asymmetry may be managed by orthodontic treatment alone. Severe skeletal asymmetries require a combination of orthodontic and surgical management. Deviation of the lower face is more frequent and greater in length than that of the upper and midface [15, 16] A possible explanation would be the longer mandibular growth periods, in addition to the maxilla being rigidly attached to the stable region of synchondroses at the cranial base [17].
Surgical treatment planning may include orthognathic facial bone contouring surgery, genioplasty and contouring of soft tissues such as the masseter muscle and buccal fat pads [18, 19] The extent of soft tissue changes as a result of related skeletal structure mobilization may be difficult to predict accurately [20] If later a second operation is required for adjustment of symmetry, alloplastic implants and fat injections for volume augmentation, as well as bone contouring and liposuction for volume reduction, can be carried out [21]
Conclusion
Correction of facial asymmetry is a complex treatment involving many different disciplines for an accurate diagnosis, treatment plan and execution of treatment to achieve an excellent esthetic and functional result for a patient.
Patient concerns associated with the consequences of surgery such as pain, swelling and lengthy healing period can be addressed with the use of Intraoral photobiomodulation delivered in this case report by using a PBM Implant device. Treatment was completed faster with minimal pain and no pain medication usage with Photobiomodulation. The use of PBM should be considered a valuable tool to enhance the entire surgical process and provide the patient with the best treatment experience.
Conflicts of Interest
Dr Alan Kwong Hing is the Founder and Chairman of PBM Healing International
Dr Michael Hamblin is a consultant to PBM Healing International
Acknowledgments
As part of the manuscript preparation, language editing and formatting were supported by AI-based tools (ChatGPT, OpenAI) to enhance clarity and consistency.
Data Availability Statement
Data can be made accessible upon publication following approval of a proposal and a signed data access agreement through the corresponding author.
Funding Statement
Funded by PBM Healing International Ltd. No influence on data analysis or publication decisions.
Ethics Approval Statement
This report was conducted in accordance with ethical standards and GCP guidelines as per ISO 14155. The single study did not need the Ethics Review Board of any institution.
Patient Consent Statement
The patient signed an informed consent form for participation in the case study and an authorization form permitting the use of their information and data for research purposes.
Consent for Publication
Consent was given by the patient for images included in the report. All authors confirm consent for publication.
References
- Lindauer SJ (1998) Asymmetries: diagnosis and treatment. Semin Orthod. 4(3): 133.
- Cheong YW, Lo LJ (2011) Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J.34(4): 341–51.
- Cohen MM Jr (1995) Perspectives on craniofacial asymmetry. III. Common and/or well-known causes of asymmetry. Int J Oral Maxillofac Surg. 24(2): 127–33.
- Reyneke JP, Tsakiris P, Kienle F (1997) A simple classification for surgical treatment planning of maxillomandibular asymmetry. Br J Oral Maxillofac Surg. 35(5): 349–51.
- Chew MT (2005) Soft and hard tissue changes after bimaxillary surgery in Chinese Class III patients. Angel Orthod. 75(6): 959– 63.
- Chew MT (2006) Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angel Orthod. 76(5): 806–9.
- Agrawal M, Agrawal JA, Nanjannawar L, Fulari S, Kagi V (2015) Dentofacial asymmetries: challenging diagnosis and treatment planning. J Int Oral Health.7(7): 128–31.
- Toh AQJ, Lee CK, Tay AG, Chan LL, Toh CG (2021) Mandibular asymmetry as a possible etiopathologic factor in temporomandibular disorder: a prospective cohort of 134 patients. Clin Oral Investig. 25(5): 2951–60.
- Karu TI, Pyatibrat LV, Folyakov SF, Afanasyeva NI (2005) Absorption measurements of a cell monolayer relevant to phototherapy: reduction of cytochrome c oxidase under near IR radiation. J Photochem Photobiol B. 81(2): 98–106.
- Reynolds PA (1996) An investigation into the safety of low level laser irradiation [PhD thesis]. London: University of London.
- Desmet KD, Paz DA, Corry JJ, Eells JT, Wong-Riley MT, et al. (2006) Clinical and experimental applications of NIR-LED photobiomodulation. Photomed Laser Surg. 24(2): 121–8.
- da Silva RV, Camilli JA (2006) Repair of bone defects treated with autogenous bone graft and low-power laser. J Craniofac Surg. 17(2): 297–301.
- Piheiro ALB, Limeira Junior F, Marquez Gerbi ME, Ramalho LM, Maronezi MC (2003) Effect of low-level laser therapy on the repair of bone defects grafted with inorganic bovine bone. Braz Dent J.14(3):177–81.
- Mayo Clinic Staff. Jaw surgery (2018).
- Haraguchi S, Takada K, Yasuda Y (2002) Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 72(1): 28–35.
- Choi JY, Choi JP, Lee YK, Baek SH (2010) Simultaneous correction of hard- and soft-tissue facial asymmetry: combination of orthognathic surgery and face lift using a resorbable fixation device. J Craniofac Surg.21(2): 363–70.
- Ferguson JW (2005) Definitive surgical correction of the deformity resulting from hemimandibular hyperplasia. J Craniomaxillofac Surg. 33(3): 150–7.
- Jung YJ, Kim MJ, Baek SH (2009) Hard and soft tissue changes after correction of mandibular prognathism and facial asymmetry by mandibular setback surgery: three-dimensional analysis using computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.107(6): 763–71.
- Mackool RJ, Hopper RA, Grayson BH, Holliday R, McCarthy JG (2003) Volumetric change of the medial pterygoid following distraction osteogenesis of the mandible: an example of the associated soft-tissue changes. Plast Reconstr Surg.111(6): 1804–7.
- Weinberg SM, Naidoo S, Govier DP, Martin RA, Kane AA, et al. (2010) Anthropometric precision and accuracy of digital three-dimensional photogrammetry: comparing the Genex and 3dMD imaging systems with one another and with direct anthropometry. J Craniofac Surg. 21(3): 763–7.
- Lübbers HT, Medinger L, Kruse A, Grätz KW, Matthews F (2010) Precision and accuracy of the 3dMD photogrammetric system in craniomaxillofacial application. J Craniofac Surg. 21(3): 763–7.