Weixin Pan1,2*#, Wenfeng Zeng1#, Yingxiu Chen1, Zuxuan Gu1, Yang Yu1
1Department of Urology, Hainan Western Central Hospital, Danzhou, China
2Department of Urology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
#Weixin Pan and Wenfeng Zeng authors contributed equally to this work.
*Corresponding Author: Weixin Pan, Department of Urology, Hainan Western Central Hospital, Danzhou, China, Department of Urology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China.
Abstract
Background
Postoperative delirium is a typical impairment in cognition, especially for those older patients who suffered from surgery, characterized by an acute change in confusion and inattention. Due to the lack of reliable predictive markers of postoperative delirium, The onset time of postoperative delirium is unpredictable, and the treatment of postoperative delirium is brutal.
Case presentation
The case is of a 65-years-older man with kidney rupture, multiple fractures of the ninth rib, and diabetes suffered from nephrectomy and gastrointestinal decompression. Then he developed delirium 59 hours after surgery. By treating them with benzodiazepines (midazolam + diazepam) actively and so on, he recovered well and was discharged from the hospital.
Conclusion
A combination medication strategy of midazolam and diazepam effectively treated postoperative delirium after nephrectomy due to traumatic renal rupture. Besides medication, our case highlights the importance of care and psychological guidance in postoperative delirium.
Keywords: Postoperative Delirium, Nephrectomy, Traumatic Renal Rupture, Midazolam, Diazepam
Introduction
Postoperative delirium (POD) is the most common surgical complication in older adults, occurring in 15 % to 25 % of patients following elective major surgery [1]. Besides, POD is a dramatic change in mental status that affects more than 7 million hospitalized patients in the U.S each year and also increases the probability that a patient will be hospitalized for 30 days after discharge [2]. There are few reports about postoperative delirium after nephrectomy for traumatic renal rupture. This case study discusses the case of traumatic renal rupture and reviews the literature. Therefore, after obtaining the patient's authorization and consent, we publish his clinical data to provide a reference for medical workers.
Case presentation
Patient Chief Complaint and Past History
A 66-year-old male who fell from a boat 3 hours ago ruptured his kidney, with a history of diabetes, no history of hypertension, coronary heart disease, chronic obstructive pulmonary disease, asthma, and no history of drug and food allergies.
Physical Examination
The patient was conscious when he was admitted to the hospital. The skin on the left waist is local redness and swelling with tenderness. Catheterization showed that red urine flowed from the urinary catheter, about 200 ml.
Accessory Examination
An abdominal CT scan showed the left kidney rupture and the left ninth rib fracture.
Healing Process
The patient was admitted to the hospital for a left-sided nephrectomy and was given blood transfusions during the operation. The patient developed delirium 59 hours after the procedure and regained consciousness 127 hours after the operation. During the POD process, the patient returned to a conscious state after changing quiet wards, proper restraint, adjusting sleep time, and drug sedation.
Diagnostic Assessment
The laboratory test results when the patient was in the initial and final stage of POD are shown in Table 1.
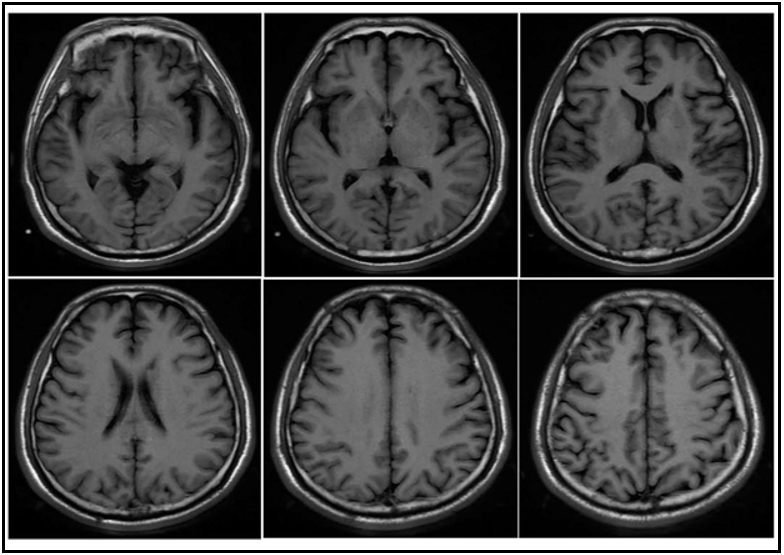
The result of the MRI of the brain when the patient is in the state of POD is shown in Figure 1.
Table 1 . The laboratory test results when the patient was in the initial and final stage of POD
|
|
Before the POD |
After the POD |
|
Hemoglobin |
78 g/L |
72 g/L |
|
RBC count |
2.50×10^12/L |
2.39×10^12/L |
|
Platelets |
123×10^9/L |
226×10^9/L |
|
Plasma prothrombin time |
11.8 s |
12.40 s |
|
International Normalized Ratio |
1.02 |
1.03 |
|
D-dimer assay |
3860 ng/ml |
7250 ng/ml |
|
Serum sodium |
139 mmol/L |
139 mmol/L |
|
Serum potassium |
3.89 mmol/L |
3.68 mmol/L |
|
Serum calcium |
2.03 mmol/L |
1.95 mmol/L |
|
serum creatinine |
80 umol/L |
67 umol/L |
Figure 1: The result of MRI in brain when the patient in the state of POD
Local brain tissue in the left basal ganglia was softened with gliosis, and there were a few lacunar ischemic foci in the right frontal lobe and bilateral occipital lobe.
The Detection Method of POD
The confusion assessment method (CAM) was used to detect patients with POD [3].
Interventions and Follow-Up
The doctor told the patient that if he felt unwell after being discharged from the hospital, he should return to the hospital immediately for further treatment. At the 6-month follow-up, the patient recovered well.
Discussion
POD is a common medical problem treated as a complication due to unrecognized, misdiagnosed, and undertreated by doctors or nurses[4]. Therefore, it was essential to identify and assess risk factors early in the treatment of POD.
There were risk factors associated with POD, such as levels of perceived stress [5], Postoperative inflammatory reaction [6], levels of postoperative pain[7], a history of cerebrovascular disease, low Hasegawa Dementia Scale-Revised score < 20 points, low serum albumin level < 3.5 g/dL and long surgery duration >4 h [8]. Besides, there are biomarkers associated with POD, for example, amino acids, melatonin, Interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-1 (IL- 1),interleukin-2 (IL-2), C-reactive protein (CRP), insulin-like growth factor 1, S–100B, apolipoprotein- E (APO-E), cortisol, estradiol, TNF- alpha [9]. However, current articles are enough to predict the risk of POD, but there was not enough evidence to support using any single biomarker as the sole risk of the disease marker for POD [10]. Therefore, care should be the main agenda for POD in further research. Most nurses and doctors in China considered delirium a severe problem, but their cognition of rage was lacking [11]. In Germany, although nurses believed POD and related problems were highly correlated, doctors seem to have limited knowledge of these conditions [12]. Taken together, compared to doctors, nurses are highly concerned about delirium. Therefore, nurses should play a central role in POD coordination and care. If this standard is going to be established, then clinical nurses must be educated and authorized to implement nonpharmacological interventions for patients with POD.
The voice of a loved one was an adequate measure of nonpharmacological treatment. A study shows that recording the mother's voice may effectively reduce emergence agitation in children undergoing bilateral eye surgery [13]. Although the result was not statistically significant in our observation that patients were less agitation in the company of their family members.
Besides, some nonpharmacological interventions, such as lower voice thresholds in the morning and higher voice thresholds during the day, are associated with an increased incidence of delirium in the intensive care unit [14]. The duration and frequency of restraint were positively correlated with fever [15]. Patients in a single bedroom take a lower risk of delirium than those in a multi-bedroom [16].
Finally, it has been controversial whether antipsychotic treatment is effective for delirium. There was rare evidence to support the use of antipsychotics for agitation, and anesthesia guidelines recommend avoiding benzodiazepines in older patients[17,18]. However, in our report, a patient with POD was successfully cured with midazolam, and there was no postoperative cognitive decline in the patient at the 6- month follow-up. In the case of excluding individual differences, it is necessary to research the safety and reliability of midazolam in elderly patients with POD.
Conclusion
Our case reports are unique and informative. We need more evidence to support using any single biomarker as POD's sole risk or disease marker.
Besides, we need more evidence to support the evidence that POD is more likely to occur in patients with only one kidney due to the poor metabolism of anesthetics. Therefore, we should pay attention to the role of care in POD patients. The effectiveness of drug therapy for POD is a difficult question, and more studies are needed to confirm the reliability of the results.
Acknowledgement: We thank the patients for their support and consent for the publication of the data.
Statement of Ethics: Approval was received from the Ethics Board of the Hainan Western Central Hospital. The patient has signed written informed consent for the publication of this case report and any associated images.
Conflict of Interest Statement: The authors declare that there is no conflict of interest regarding the publication of this manuscript.
Funding Sources: None
Author Contribution
Yang Yu, Yingxiu Chen and Zuxuan Gu made contributions to the full management of patients in clinical practice, Wenfeng Zeng contributed in the writing of the manuscript, Weixing Pan contributed to the concept and design. All authors read and approved the final manuscript
Data Availability Statement: The data supporting the results of this article included within the article and its additional files.
References
- Marcantonio ER (2017) Delirium in Hospitalized Older Adults. N Engl J Med. 377(15): 1456-1466.
- LaHue SC, Douglas VC, Kuo T, Conell CA, Liu VX, et al. (2019) Association between Inpatient Delirium and Hospital Readmission in Patients 65 Years of Age: A Retrospective Cohort Study. J Hosp Med. 14(4): 201-206.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, et al. (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 113(12): 941-948.
- Florou C, Theofilopoulos D, Tziaferi S, Chania M (2017) Post- Operative Delirium in Elderly People Diagnostic and Management Issues of Post-Operative Delirium in Elderly People. Adv Exp Med Biol. 987: 301-312.
- Banjongrewadee M, Wongpakaran N, Wongpakaran T, Pipanmekaporn T, Punjasawadwong Y, et al. (2020) Role of perceived stress in postoperative delirium: an investigation among elderly patients. Aging Ment Health. 24(1): 148-154.
- Plaschke K, Weigand MA, Fricke F, Kopitz J (2016) Neuroinflammation: effect of surgical stress compared to anaesthesia and effect of physostigmine. Neurol Res. 38(5): 397- 405.
- Wang Y, Sands LP, Vaurio L, Mullen EA, Leung JM (2007) The effects of postoperative pain and its management on postoperative cognitive dysfunction. Am J Geriatr Psychiatry. 15(1): 50-59.
- Matsuki M, Tanaka T, Takahashi A, Inoue R, Hotta H, et al. (2020) Incidence and risk factors of postoperative delirium in elderly patients undergoing urological surgery: A multi-institutional prospective study. Int J Urol. 27(3): 219-225.
- Dunne SS, Coffey JC, Konje S, Gasior S, Clancy CC, et al. (2021) Biomarkers in delirium: A systematic review. J Psychosom Res. 147: 110530.
- Marcantonio ER (2020) Still Predicting Delirium After All These Years. Anesth Analg. 130(1): 76-78.
- Xing J, Sun Y, Jie Y, Yuan Z, Liu W (2017) Perceptions, attitudes, and current practices regards delirium in China: A survey of 917 critical care nurses and physicians in China. Medicine (Baltimore). 96(39): e8028.
- Sturm H, Wildermuth R, Stolz R, Bertram L, Eschweiler GW, et al. (2019) Diverging Awareness of Postoperative Delirium and Cognitive Dysfunction in German Health Care Providers. Clin Interv Aging. 14: 2125-2135.
- Byun S, Song S, Kim JH, Ryu T, Jeong MY, et al. (2018) Mother's recorded voice on emergence can decrease postoperative emergence delirium from general anaesthesia in paediatric patients: a prospective randomised controlled trial. Br J Anaesth. 121(2): 483-489.
- Sangari A, Emhardt EA, Salas B, Avery A, Freundlich RE, et al. (2021) Delirium Variability is Influenced by the Sound Environment (DEVISE Study): How Changes in the Intensive Care Unit soundscape affect delirium incidence. J Med Syst. 45(8): 76.
- Pan Y, Jiang Z, Yuan C, Wang L, Zhang J, et al. (2018) Influence of physical restraint on delirium of adult patients in ICU: A nested case-control study. J Clin Nurs. 27(9-10): 1950-1957.
- Blandfort S, Gregersen M, Rahbek K, Juul S, Damsgaard EM (2020) Single-bed rooms in a geriatric ward prevent delirium in older patients. Aging Clin Exp Res. 32(1): 141-147.
- Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM (2016) Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta- Analysis. J AM GERIATR SOC. 64(4): 705-714.
- Lee D, Petersen F, Wu M, Chapman G, Hayman M, et al. (2021) A prospective observational cohort pilot study of the association between midazolam use and delirium in elderly endoscopy patients. Bmc Anesthesiol. 21(1): 53.