A Picton1, C Venter2*
1Reproductive Medicine Assistant, Vitalab Centre for Assisted Conception, Sandton and Umhlanga, South Africa.
2Reproductive Medicine Specialist, Affiliated lecturer to University of the Free State, South Africa
*Corresponding Author: C Venter, Reproductive Medicine Specialist, Affiliated lecturer to University of the Free State, South Africa
Abstract
Background: A growing number of patients who desire future fertility, are presenting to IVF Units post-UAE (Uterine Artery Embolization) for fibroids. In most cases, the uterus remains unsuitable for gestation because of persistent fibroids, while others display endometrial or ovarian dysfunction. In all cases, these patients were advised by their gynaecologist to pursue UAE over myomectomy and referred for treatment.
Objective: To review the evidence regarding UAE versus myomectomy in women with fibroids who expressly seek future fertility.
Conclusions: UAE versus myomectomy for fibroids is associated with lower rates of pregnancy and livebirth with higher rates of miscarriage. UAE impairs ovarian reserve and is associated with significant post-intervention endometrial abnormalities. UAE offers no significant procedural risk reduction over myomectomy. In women with fibroids, expressly seeking future pregnancy, UAE should be reserved for women refusing or unsuitable for surgery.
Keywords: Uterine Artery Embolization (UAE), Myomectomy, Fibroids, Fertility.
Introduction
Uterine fibroids are the most common benign tumour affecting women. Lifetime prevalence is 50-60 %, rising to 70 % by age 50.[1] Management of symptomatic fibroids has traditionally fallen to surgical treatment, with medical management limited to 6-months due to the risks of osteoporosis.[2]
In symptomatic patients, UAE vs hysterectomy offers comparable rates of satisfaction (78 % vs 87 %) for symptom relief.[3] It is controversial whether UAE should be offered to women still desiring future fertility. [4,5,6,7] It is about this group of women that this article is written.
Fibroids and Fertility
Fibroids, except for sub-serosal location, are associated with lower pregnancy rates (RR = 0.697, P < 0.001) and higher miscarriage rates (RR= 1.678, P < 0.001). This includes intra-mural fibroids with no effect on the cavity. Sub-mucosal fibroids are associated with the lowest ongoing pregnancy rate (RR = 0.318, P < 0.001).[8] The pathophysiology of sub- fertility is related to endometrial receptivity and HOX gene expression [9], altered myometrial contractility and increased endometrial venous pressure.[10]
Complication Rate associated with UAE and Surgery
UAE is seen as a means of reducing the surgical risk to patients. What is the evidence from RCT’s?
Myomectomy vs UAE is associated with less early (15.9 % vs. 20.7 %), and late (8.1 % vs. 13.8 %) postprocedural complications.[5] Hysterectomy versus UAE is showed fewer major complications: 2.7 % vs. 4.9 % (P-value = 0.68) and significantly fewer minor complications: 40 % vs. 58.0 %, RR= 1.45, (95 % CI: 1.04 – 2.02, P = 0.24).[11]
Uterine integrity following myomectomy remains a concern to gynaecologists for future pregnancy, especially in patients expressing the desire to deliver naturally.
In an unselected population, the prevalence of uterine rupture is 0.05 %, and 1.0 % following the previous caesarean section.[12] Meta-analysis shows uterine rupture in pregnancy following open vs. laparoscopic myomectomy remains low (0.4 % vs. 1.2 %, p = 0.119) while successful vaginal delivery in these groups is high 88 % vs. 93 %.[12]
UAE the Procedure
Uterine artery embolization was first described in the mid-’90s. The femoral artery is used as an entry site, to allow for catheterization of the uterine arteries and the injection of embolic particles: poly-vinyl alcohol (PVA), PVA microspheres or gelatin-coated tris-acryl microspheres, which disrupt the blood supply of the fibroid (See figure 1 attached).
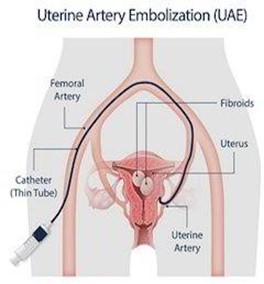
Figure 1
UAE and Ovarian Reserve
Fibroids derive their blood supply from both sides in almost all cases. Bilateral uterine artery embolization, where occlusion or marked reduction in blood flow in both uterine arteries is achieved, is considered a technical success. The recommended threshold for bilateral uterine artery embolization is 96 %.[4]
Angiography in patients undergoing UAE showed ovarian-uterine artery anastomosis in 21.7 %. The uterine artery was the major blood supply to the ovary in 6.6 % of patients.[13]
In patients undergoing hysterectomy following UAE, histology confirmed the presence of embolic particles in the fallopian tube or ovary in all patients with evidence of utero-ovarian anastomosis at the time of the procedure.[14] (See Figure 2 attached).
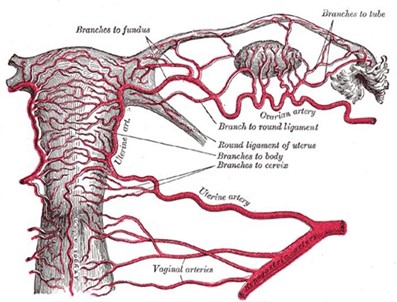
Figure 2
Analysis of AMH (Anti-Mullerian Hormone) and AFC (Antral follicle count) shows a reduction in ovarian reserve post-UAE. Women aged < 40 years show the greatest ability to recover, however, baseline levels of ovarian function are not recovered, with permanent deficit.[15] Up to 7 % of women develop permanent amenorrhoea following UAE. [16]
Post-procedural ovarian reserve testing following UAE vs. supra-cervical hysterectomy in premenopausal women, showed the averaged percentage changes in AFC and AMH, to be -63.4 % vs -8.4 % and -61.9 % vs -3.5 %, respectively. UAE is associated with significant (p < 0.001) deleterious changes in all measures of ovarian reserve.17 The reduction in ovarian reserve following UAE is more than that seen at hysterectomy.[18]
UAE and the Myometrium
UAE is associated with a 50 % volume reduction in most patients.19 Volume reduction is progressive, 46 %, 61 % and 66 % at 3, 6 and 12 months, respectively.[20] The relationship of volume to diameter is not linear, rather it is governed by the formula: Volume = 4/3π r3. This implies a 50 % volume reduction of a fibroid does not translate into a 50 % Reduction in diameter. If you have 3 fibroids of diameter 10, 8 and 5cm before UAE, and all undergo a 50 % volume reduction, you are left with fibroids of diameter 8, 6.4 and 4cm respectively.
Randomized comparison of UAE vs. myomectomy showed a reintervention rate of 32.8 % vs 3.2 %, P < 0.0001. The main indication for surgical reintervention was the persistence of a large fibroid (> 5cm) at 6 months post-UAE. [5]
UAE and the Endometrium
Hysteroscopy reveals endometrial abnormalities in 59.1% of women following UAE. This included tissue necrosis (40.9 %), intra-cavity myoma protrusion (35.4 %), intra-cavity adhesions (10.2 %), and fistulae between intra-mural myomas and the cavity (6.3 %). [21]
UAE and Pregnancy
When pregnancy outcomes are compared, UAE vs Myomectomy is associated with lower pregnancy rates (50% vs. 78%, P < 0.05), lower livebirth rates (19 % vs. 48 %, P < 0.05) and higher miscarriage rates (64 % vs. 23 %, P < 0.05).[5]
Women following UAE vs. Myomectomy have a RR = 2.22 (95 % CI: 1.11 – 4.44) not to get pregnant and a RR = 2.79 (95% CI:1.25 – 6.22) to abort.
Systematic review of UAE vs. Myomectomy showed higher miscarriage (27.4 % vs. 19.0 %, P < 0.001) and lower livebirth rates (60.6 % vs. 75.6 %, P < 0.001). [7]
Following UAE in women of average age 35.9, rates of miscarriage were 28 %, equivalent to women with untreated fibroids.[22]
Follow-up of 31 women of average age 37.3, post-UAE, all actively seeking pregnancy with normal ovarian reserve tests, showed a single pregnancy which ended in miscarriage after a total of 33.4 months. (This included the transfer of 22 embryos in own-egg IVF cycles and 8 embryos from donor-egg transfers). This equates to a monthly fecundability rate of 0.1 %, (95 % CI 0 – 0.3 %).[23]
The American College of Obstetrics and Gynaecology (ACOG) lists the express desire for future fertility as a relative contra-indication to UAE. There is a recommendation that patients be adequately counselled regards the reproductive implications before UAE.[24]
Fertility Assessment before UAE
Fibroids often co-exist with other pathology, such that while 5-10 % of women present with infertility and fibroids, in only 1 - 2.4 % of cases, are the fibroids the sole cause of infertility.[25] Pre-intervention AFC or AMH levels provide only a prognostic measure of expected ovarian response to stimulation (egg number).
The age-associated embryo aneuploidy rates [26], and averaged percentage chance of LBR (live birth rate) per mature oocyte retrieved (MOR) need to be communicated to patients to place the egg number into context. In the general IVF population (ages 23 – 43 years), LBR / MOR= 3.8 %.[27]
If considering fertility preservation prior to UAE, oocyte freezing places further demand on egg number. In comparison, to fresh oocytes, vitrified oocytes are associated with lower fertilization (77.9 % vs. 90.5 %, 95 % CI: 0.80 – 0.93), cleavage (90.0 vs. 99.2 %, 95 % CI: 0.87 – 0.96) and blastulation rates (34.8 % vs. 50.8 %, 95 % CI: 0.54 – 0.86), meaning less embryos from a given number of frozen eggs. [28]
Fertility assessment and discussion of its preservation fall outside the scope of the interventional radiologist and the generalist gynaecologist. Not involving a fertility specialist in the decision-making process around UAE in women desiring future pregnancy will ensure uninformed consent.
Conclusions
Untreated fibroids reduce pregnancy rates and increase miscarriage rates. UAE for fibroids is associated with significantly lower pregnancy rates, higher miscarriage rates and lower live birth than if managed by myomectomy. Myomectomy offers acceptable uterine integrity in subsequent pregnancy and the ability for a natural delivery, with no significantly increased procedural complication rate over UAE. Fertility evaluation of a couple is complex and best performed at a fertility unit, without which the patient makes an uninformed decision. The desire for a future pregnancy is a relative contraindication to UAE for fibroids. Patients need to be well informed of the potential adverse effects of UAE and fertility outcomes.
References
- Lisiecki M, Paszkowski M, Wozniak S (2017) Fertility impairment associated with uterine fibroids- a review of literature. Prz Menopauzalny. 16(4): 137 – 140.
- Parker WH (2007) Uterine myomas: management. Fertil Steril. 88(2): 255 – 271.
- De Bruijn AM, Ankum WM, Reekers JA, Birnie E, Van der Kooij SM, et al. (2016) Uterine artery embolization vs hysterectomy in the treatment of symptomatic fibroids: 10-year outcomes from the Emmy trial. Am J Obstet Gynecol. 215(6): 745.e1–745.e12.
- Hovsepian, D.M., Siskin, G.P., Bonn, J. Cardella, J.F., Clark, T.W.I., Lampmann, L.E. Miller, D.L., Omary, R.M., Pelage, J.P., Rajan, D., Schwartzberg, M.S., Towbin, R.B., Walker, W.J. and Sacks D. CIRSE (Cardiovascular and Interventional Radiology Society of Europe. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Cardiovasc Intervent Radiol 2004; 15: 535 – 542.
- Mara M, Maskova J, Fucikova Z, Kuzel D Belsan T, Sosna O (2008) Midterm Clinical and First Reproductive Results of a Randomized Controlled Trial comparing Uterine Fibroid Embolization and Myomectomy. Cardiovasc Intervent Radiol. 31(1): 73-85.
- Van Overhagen H, Reekers JA (2015) Uterine Artery Embolization for Symptomatic Leiomyomata. Cardiovasc Intervent Radiol. 38(3): 536 – 542.
- Khaw SC, Anderson RA, Lui M (2020) Systematic review of pregnancy outcomes after fertility-preserving treatment of uterine fibroids. Reprod Biomed Online. 40(3): 429 – 444.
- Pritts EA, Parker WH, Olive DL (2009) Fibroids and Infertility: an updated systematic review of the evidence. Fertil Steril. 91(4): 1215– 1223.
- Rackow BW, Taylor HS (2010) Submucosal uterine leiomyomas have a global effect on molecular determinants of endometrial receptivity. Fertil Steril. 93(6): 2027 – 2034.
- Buttram VC, Reiter RC (1981) Uterine Leiomyomata: Etiology, Symptomatology and Management. Fertil Steril. 36(4): 433 – 445.
- Hehenkamp WJK, Volkers NA, Donderwinkel PFJ, De Blok S, Birnie E, et al. (2005) Uterine artery embolization versus hysterectomy in the treatment of symptomatic fibroids (EMMY trial): peri-and postprocedural results from a randomized controlled trial. Am J Obstet Gynecol MFM. 193(5): 1618 – 1629.
- Claeys J, Hellendoorn I, Hammerlynck T, Bosteels J, Weyers S (2014) The risk of uterine rupture after myomectomy: a systematic review of the literature and meta-analysis. Gynecol Surg. 11(3): 197– 206.
- Razavi MK, Wolanske KA, Hwang GL, Sze DY, Kee ST, et al. (2002) Angiographic classification of ovarian artery-to-uterine artery anastomoses: initial observations in uterine artery embolization. Radiology. 224(3): 707 – 712.
- Kim HS., Thronse VR, Judson K, Vang R (2007) Utero-Ovarian Anastomosis: Histopathologic Correlation after Uterine Artery Embolization with or without Ovarian Artery Embolization. J Vasc Interv Radiol. 18(1 pt 1): 31 – 39.
- Kim CW, Shim HS, Jang H, Song YG (2016) The effects of uterine artery embolization on ovarian reserve. Eur J Obstet Gynecol Reprod Biol. 206: 172-176.
- Walker WJ, Pelage JP (2002) Uterine artery embolization for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 109(11): 1262 – 1272.
- Czuczwar P, Stepniak A, Milart P, Paszkowski T, Wozniak S (2018) Comparison of the influence of three fibroid treatment options: supracervical hysterectomy, ulipristal acetate and uterine artery embolization on ovarian reserve – an observational study. J Ovarian Res. 1(1): 45.
- Hehenkamp WJK, Volkers NA, Broekmans FJM, de Jong FH, Themmen APN, et al. (2007) Loss of ovarian reserve after uterine artery embolization: a randomized comparison with hysterectomy. Hum Reprod. 22(7): 1996 – 2005.
- Ukybassova T, Terzic M, Dotlic J, Imankulova B, Terzic S, et al. (2019) Evaluation of Uterine Artery Embolization on Myoma Shrinkage: Results from a Large Cohort Analysis. Gynecol Minim Invasive Ther. 8(4): 165 – 171.
- Tomislav S, Josip M, liana CS, Marko V, Ante R, et al. (2011) Uterine Artery embolization as Nonsurgical Treatment of Uterine Myomas. ISRN Obstet and Gynecol. 2011: 489281.
- Mara M, Horak P, Kubinova K, Dundr P, Belsan T, et al. (2012) Hysteroscopy after uterine fibroid embolization: evaluation of intrauterine findings in 127 patients. J Obstet Gynaecol Res. 2012; 38(5): 823 – 31.
- Mohan PP, Hamblin MH, Vogelzang RL (2013) Uterine artery Embolization and its Effects on Fertility. J Vasc Interv Radiol. 24(7): 925 – 30.
- Torre A, Paillusson B, Fain V, Labauge P, Pelage JP, et al. (2014) Uterine artery embolization for severe symptomatic fibroids: effects on fertility and symptoms. Hum Reprod. 29(3): 490 – 501.
- ACOG Committee Opinion. Uterine Artery Embolization. Obstet Gynecol. 2004; 103(2):403-4.
- Guo XC, Segars, JH (2012) The Impact and Management of Fibroids for Fertility: an evidence-based approach. Obstet Gynecol Clin North Am. 39(4): 521 – 533.
- Franasiak J, Forman E, Hong K, Werner M, Upham K, et al. (2014) The nature of aneuploidy with increasing age of the female partner: a review of 15, 169 consecutive trophectoderm biopsies evaluated with comprehensive chromosome screening. Fertil Steril. 101(3): 656 – 663.
- Stoop D, Ermini B, Polyzos N, Haentjens P, De Vos M, et al. (2012) Reproductive potential of a metaphase II oocyte retrieved after ovarian stimulation: an analysis of 23, 354 ICSI cycles. Hum Reprod. 27(7): 2030-2035.
- Forman E, Li X, Ferry K, Scott K, Treff N, et al. (2012) Oocyte vitrification does not increase the risk of embryonic aneuploidy or diminish the implantation potential of blastocysts created after intracytoplasmic sperm injection: a novel paired randomized controlled trial using DNA fingerprinting. Fertil Steril. 98(3): 644- 649.



