Mohammad Al-Akchar1 *, Abdisamad M. Ibrahim2, Mohsin Salih1, Mukul Bhattarai1, Cameron Koester2, Mohamed Labedi1, Tareq Zaza, Robert Robinson2
1Division of Cardiology. Department of Internal Medicine. SIU School of Medicine
2Department of Internal Medicine. SIU School of Medicine
*Corresponding Author: Mohammad Al-Akchar, MD SIU-School of Medicine, 701 N. First St., Rm. D442, Springfield, Il 62781.
Abstract
Background
Interpretation of electrocardiograms (EKG) is an essential tool for every physician. Despite this, the diagnosis of life-threatening pathology on EKG remains suboptimal in trainees. The purpose of this study is to study resident attitudes and behaviors towards EKGs and describe an innovative way to teach EKGs.
Methods:
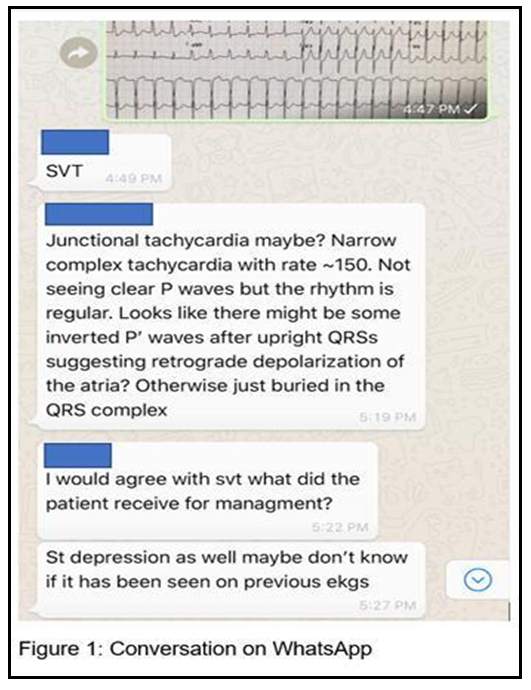
An observational cross-sectional study through an anonymous online survey of internal medicine residents’ attitudes and comfort with EKG interpretation in Southern Illinois University in 2018. This was followed by the creation of a WhatsApp group for discussion and interpretation of EKGs with peers. At the end of the day, the official EKG interpretation was posted.
Results:
Forty-one out of 63 residents (65 %) completed the survey. 85 % of respondents thought that an interactive way to teach EKGs is the best method of teaching, and 73 % did not feel confident interpreting EKGs. 30 % often rely on automated EKG interpretation. Further analysis indicated that PGY-1 residents reported ordering fewer EKGs (correlation coefficient -0.399, p = 0.012) and were uncomfortable diagnosing QT prolongation on an EKG (correlation coefficient -0.310, p = 0.049). Residents in the third or greater year of the training ordered more EKGs (correlation coefficient 0.379, p = 0.015), less frequently relied on the computer for EKG diagnosis (correlation coefficient 0.399, p = 0.010), and were comfortable diagnosing an acute myocardial infarction and atrial arrhythmias.
Conclusion: In conclusion, most IM trainees do not feel comfortable interpreting EKG, however, this does improve with PGY year. New social media platforms (such as WhatsApp) may be an innovative way of teaching EKGs.
Keywords: Electrocardiogram, Medical Education, WhatsApp
Abbreviations: EKG – Electrocardiogram, STEMI - ST-elevation myocardial infarction SIU - Southern Illinois University, PGY - Post Graduate Year
Introduction
Introduced more than 100 years ago by William Einthoven, Electrocardiograms (EKG) remain an essential tool for doctors in diagnosing a variety of conditions. An abnormal EKG remains part of the criteria for diagnosing and activating the response for ST-elevation myocardial infarction (STEMI), one of the most important causes of mortality nationwide [1,2] and it is a major diagnostic tool for many cardiovascular diseases like myocarditis and cardiogenic shock [3,4,5]. Interpretation of EKGs is an essential tool for any physician, especially in the field of internal medicine, often one of the first lines of defense for diagnosing EKG abnormalities. It is a skill that is learned during medical school and residency training [6]. Despite this, the diagnosis of life-threatening pathology on EKG remains suboptimal in trainees [7]. This poor performance may be attributed to a lack of a standard methodology of teaching EKGs across the United States [7]. Also, the introduction of computerized interpretation may have led to over-reliance on automated readings and less effort to interpret and teach EKGs [8].
Historically, EKG interpretation had been taught bedside, during rounds, and through didactic lectures [9]. The competing responsibilities, pressure for early discharge, and the increase in volume and acuity of patients have led to shorter rounding duration as well as less didactic time. In fact, a study has shown that bedside teaching compromises less than 20 % of the length of rounds [10]. As a result, residents tend to self-study EKGs and read books on their own time without direct feedback on their interpretation skills. A study evaluating the retention of ECG interpretation skills found that workshop-based or lecture-based teaching was superior to self-directed learning with over a 10 percent difference in scores between these groups [11].
The new challenges of learning created new solutions and methods for teaching. With multiple communication apps being introduced in the 21st century, including Facebook, Telegram, Twitter, WhatsApp, and others have found their way in aiding medical education, especially given the common use amongst millennials. One study report that 99 % of medical students use WhatsApp (9). Another study estimated WhatsApp usage to be around 20 % of all smartphone behavior [12]. All of this led to increasing use of social media as a tool of education. In this study, we evaluate behaviors and attitudes of medical residents toward EKGs, and we describe an innovative way to teach EKGs through a group chat using the WhatsApp platform.
Methods
In 2018, the Southern Illinois University (SIU) School of Medicine Internal Medicine residency program conducted a cross-sectional observational study of internal medicine residents. We investigated attitudes and behaviors towards EKGs through multi-item surveys (see table one for questions). This was followed by the creation of a WhatsApp group to aid in teaching EKGs. Membership in the WhatsApp group was voluntary and was open to all internal medicine residents, cardiology fellows, and faculty. A de-identified EKG interpreted by an electrophysiology specialist was chosen by cardiology fellows and posted to the WhatsApp group every Wednesday. Residents were encouraged to interpret and discuss the EKG with peers. At the end of the day, the official EKG interpretation was posted. This would be followed by questions from faculty members and residents and a final wrap-up (Figure one). The SIU School of Medicine Internal Medicine residency program is an ACGME accredited residency located in Springfield, Illinois, USA. The residency has 42 categorical internal medicine residents, 11 preliminary residents, and 10 medicine/psychiatry residents. For purposes of data analysis, 4th and 5th-year medicine psychiatry residents were classified as Post Graduate Year (PGY)-3 residents. An anonymous online survey of resident attitudes and comfort with EKG interpretation was sent out to the “EKG of the Week group” after one month.
Measurement Test:
Forty-two internal medicine residents at SIU School of Medicine were administered questionnaires through an anonymous survey. The questions included in the survey included the following (Table 1)
Table 1: Survey questions
|
Questions |
Answers |
|||||
|
How important are EKGs in addressing cardiac issues? |
Low importance |
Slightly important |
Neutral |
Moderately important |
Very important |
Extremely important |
|
How often do you order EKGs per week on average? |
Less than 1 |
1 to 5 |
5 to 10 |
10 to 15 |
More than 15 |
|
|
How often do you rely on computer- generated diagnosis for the interpretation of EKG? |
Never |
Occasionally |
Sometimes |
Often |
Always |
|
|
I am confident in my EKG interpretation skills |
Strongly disagree |
Disagree |
Neither agree or disagree |
Agree |
Strongly agree |
|
|
Did you receive any form of training in reading and interpreting EKG in your residency? |
Yes |
No |
|
|
|
|
|
If yes, what form of training did you receive? |
Didactics |
Modules |
Focus groups |
Bedside teaching |
|
|
|
Do you think an EKG course will help enhance your EKG interpretation skills? |
Yes |
No |
Maybe |
|
|
|
|
What resources do you use for learning EKGs? |
Books |
Internet |
Senior residents |
Attending |
Cardiology Rotation/Atten ding |
Didactics |
|
How comfortable are you at interpreting the following on EKG? |
|
|
|
|
|
|
|
Myocardial infarction? |
Not at all comfortable |
Slightly comfortable |
Somewhat comfortable |
Moderately comfortable |
Extremely comfortable |
|
|
QT prolongation? |
Not at all comfortable |
Slightly comfortable |
Somewhat comfortable |
Moderately comfortable |
Extremely comfortable |
|
|
Atrial fibrillation? |
Not at all comfortable |
Slightly comfortable |
Somewhat comfortable |
Moderately comfortable |
Extremely comfortable |
|
|
Other atrial arrhythmias? |
Not at all comfortable |
Slightly comfortable |
Somewhat comfortable |
Moderately comfortable |
Extremely comfortable |
|
|
Ventricular arrhythmias? |
Not at all comfortable |
Slightly comfortable |
Somewhat comfortable |
Moderately comfortable |
Extremely comfortable |
|
|
What would be the best way to improve your EKG interpretation? |
EKG didactics |
EKG modules |
Reading EKG books |
Watching online lectures |
Other |
|
|
What year are you currently in? |
PGY-1 (categorical) |
PGY-1 (Prelim) |
PGY-2 |
PGY-3 |
PGY-4 |
PGY-5 |
|
Are you interested in pursuing a fellowship? |
Yes |
No |
Maybe |
|
|
|
|
If yes - what fellowship |
List your answer here |
|
|
|
|
|
Statistical analysis
Spearman correlations were used to assess the strength and direction of the association PGY year with comfort in interpreting EKGs. Two-sided P-values < 0.05 were considered significant. Statistical analysis was performed using SPSS version 25 (SPSS Inc., Chicago, IL, USA).
Results
Participation in the survey was good with 41 out of 63 residents (65 %) completing the survey. Forty-one percent of the respondents were PGY-1, 29 % were PGY-2, and 29 % were PGY-3 and above. The results of this anonymous survey indicated that PGY-1 residents reported ordering fewer EKGs (correlation coefficient -0.399, p = 0.012) and were uncomfortable diagnosing QT prolongation on an EKG (correlation coefficient -0.310, p = 0.049). Residents in the third or greater year of the training ordered more EKGs (correlation coefficient 0.379, p = 0.015), less frequently relied on the computer for EKG diagnosis (correlation coefficient 0.399, p = 0.010), and were comfortable diagnosing an acute myocardial infarction and atrial arrhythmias. Table 2 summarizes the analysis of questions in relation to PGY year.
Table 2: EKG survey by PGY Year
|
Questions |
PGY-1 |
PGY-2 |
PGY-3+ |
|
N=17 |
N=12 |
N=12 |
|
|
How often do you order EKGs? |
Correlation -0.339 |
Correlation 0.043 |
Correlation 0.379 |
|
P = 0.012 |
P = 0.790 |
P = 0.015 |
|
|
How important are EKGs in addressing cardiac issues? |
Correlation 0.045 |
Correlation -0.097 |
Correlation 0.049 |
|
P = 0.781 |
P = 0.546 |
P = 0.763 |
|
|
How often do you rely on the computer diagnosis for interpreting EKGs? |
Correlation 0.058 |
Correlation 0.269 |
Correlation -0.331 |
|
P = 0.718 |
P = 0.093 |
P = 0.036 |
|
|
How confident are you in your EKG interpretation skills? |
Correlation -0.198 |
Correlation -0.184 |
Correlation 0.399 |
|
P = 0.214 |
P = 0.249 |
P = 0.010 |
|
|
How comfortable are you in diagnosing a specific problem on an EKG? |
|
|
|
|
Acute Myocardial Infarction |
Correlation -0.134 |
Correlation -0.176 |
Correlation 0.321 |
|
P = 0.402 |
P = 0.272 |
P = 0.041 |
|
|
QT Prolongation |
Correlation -0.310 |
Correlation 0.081 |
Correlation 0.254 |
|
P = 0.049 |
P = 0.615 |
P = 0.108 |
|
|
Atrial fibrillation |
Correlation -0.188 |
Correlation -0.073 |
Correlation 0.276 |
|
P = 0.240 |
P = 0.651 |
P = 0.081 |
|
|
Other atrial arrhythmias |
Correlation -0.069 |
Correlation -0.224 |
Correlation 0.319 |
|
P = 0.667 |
P = 0.125 |
P = 0.042 |
|
|
Ventricular arrhythmias |
Correlation 0.007 |
Correlation -0.186 |
Correlation 0.179 |
|
P = 0.967 |
P = 0.245 |
P = 0.264 |
Ninety-three percent of the residents selected very important or extremely important in EKGs addressing cardiac issues. Eighty percent of the residents were interested in pursuing fellowships; with 25 % showing interest in cardiology, 10 % in hematology/oncology, and 7 % critical care.
Only 49 % of residents reported receiving training in reading and interpreting EKGs in the following forms: 70 % indicated receiving bedside teaching, 40 % didactics, 20 % focus groups, 5 % modules, and/or senior resident-led teaching. Ninety percent indicated that an
EKG course will help enhance their interpretation skills. Sixty-six percent of the residents selected EKG didactics as the best way of learning and improving EKG interpretation. Most residents reported learning EKG from multiple sources with the selection of internet (80 %) and books (61 %) being the most popular.
As for the WhatsApp group, over a period of 8 months, more than 30 common and challenging EKGs were posted and discussed. The group grew to include all cardiology fellows, 9 faculty members, and 50 internal medicine preliminary and categorical residents. The number of responses to an EKG of the week post ranged from 3 to 50, with an average of 16 responses per post. After four months, a brief two-question survey was conducted to obtain feedback from the participants. The questions were whether the EKG group helped you in interpreting EKGs and whether any suggestions were available to help enhance the group. 84% of respondents felt that this method helped them in EKG interpretation. Respondents suggested adding the clinical context and outcome of the patient at the end of the discussion. It also suggested posting the EKG later in the day as opposed to morning and posting the interpretation later on to allow more time for residents to participate in the discussion.
Discussion
Interpretation of EKGs is a critical skill needed for all physicians, especially internal medicine physicians. Since 1895 when Dr. William Osler coined the term “internal medicine training” and till this day [11], there continues to be a dynamic change in resident responsibilities, skills, learning, educational curriculum, and time dedicated to teach and learn. The key findings of our study are that over 50 % of residents did not feel comfortable interpreting EKGs. In addition, two-thirds of residents selected an interactive way to teach EKGs as the best method to learning EKGs. Finally, our study showed teaching EKGs through WhatsApp may be a new innovative way to supplement learning EKGs.
The ability of trainees to interpret electrocardiograms is highly variable and depends on the level of training. Several studies evaluating senior medical students have shown them to miss 26% to 62% of acute myocardial infarctions [13]. Another study involving internal medicine residents demonstrated that only half of the common ECGs findings were interpreted correctly [14]. Acute MI and life-threatening ventricular tachycardia were missed by 26% and 56% of trainees, respectively [13,14]. In our study, only 26.8 % of IM trainees felt comfortable interpreting EKGs, however, the level of confidence did improve with advancing PGY year. PGY-1 residents reported ordering fewer EKGs (correlation coefficient -0.399, p = 0.012) and were uncomfortable diagnosing QT prolongation on an EKG (correlation coefficient -0.310, p = 0.049). But many experienced residents who are in the third or greater year of the training ordered more EKGs (correlation coefficient 0.379, p = 0.015) and less frequently relied on the computer for EKG diagnosis (correlation coefficient 0.399, p = 0.010), and were comfortable diagnosing an acute myocardial infarction and atrial arrhythmias. ECG interpretation is often poor at undergraduate and postgraduate levels [9]. Similar to the study by Eslava et al, our study also showed that Internal medicine residents at the beginning of their residency training demonstrated low overall proficiency in interpreting ECGs and self-perceived confidence.
Our study also evaluated an important aspect of trainee practices in relation to reliance on EKG interpretation. Automated interpretation may influence physicians’ ECG reading. A retrospective study by Garvey et al has shown that the machine set algorithms may demonstrate wide variations and discrepancies in false positive (overdiagnosis in 0 % to 42 %) and false-negative results (underdiagnosis in 22 % to 42 %) [14]. In our study, 30 % of residents often rely on automated ECG interpretation. This was higher than another study (2) that looked at family medicine residents and reliance on EKG interpretation and found it to be 21 %. While automated interpretation improves the diagnostic abilities when the interpretation is correct, it does increase the probability of errors when the proposed diagnosis is incorrect, and negatively influences the decision-making of the physician in charge of the patient [16,17]. It has been roughly estimated that such misdiagnoses may account for up to a large number of avoidable adverse effects or deaths worldwide annually [18]. Nevertheless, diagnostic errors and wrong interpretation also depend on the level of expertise, training of the physician, time constraints, or fatigue [19,20].
In order to provide a solution to low comfort in interpreting EKGs, it was important to investigate which methods are preferred for learning EKG interpretation. A survey in 2005 involving Internal Medicine clerkship directors showed that the most common teaching method of EKGs was lecturing (75 %) followed by teaching rounds (44 %) [10]. In our study, the most common way of receiving education on EKG interpretation was rounded (70 %). Most residents reported learning EKG interpretation from multiple sources with the selection of internet (80 %) and books (61 %) being the most popular. While self-directed learning has been encouraged to improve the skills of ECG learning it is associated with poorer competence in ECG interpretation [9]. Learners often follow the internet sharing site ECG interpretation videos which may contain misleading information. When residents in our study were questioned about their preferred method of learning EKGs, 66 % percent selected EKG didactics as the best way of learning and improving EKG interpretation. What we found common across the answers of the preferred method, and what another study suggested, was that an interactive approach is the best method of teaching EKGs While the survey gave us input about the attitudes towards EKGs and behavior of learning, it also opened a door for innovation and the use of new tools in medical education. Social media, in general, continues to gain more popularity in the youth group. Having more than 1 billion active users across the world, WhatsApp® is a free communication tool that is utilized by many residents [12]. Its advantage of having secure encrypted communication makes it highly valuable in medical education compared to other platforms. It also keeps the critical component of interaction in learning. Furthermore, with several faculty, different levels of knowledge, and trainee level, this opens the door for peer-to-peer teaching, faculty input, and easy access to learning from each other. With several other studies reporting the utility and benefit of this model to supplement teaching [21,22], we opted to utilize WhatsApp in teaching EKGs. The concept of one EKG a week compared to daily was chosen to lower the burden of participation, and to allow residents to read up on discussed concepts every week. Similar to other studies, the participation grew over time [22]. The number of responses to an EKG of the week post ranged from 3 to 50, with an average of 16 responses per post. We believe that participation grew as residents became more comfortable sharing their answers, knowledge, and questions. In addition, the WhatsApp group allowing peer-to-peer teaching made residents more comfortable with making mistakes and learning from them. With this easily accessible app, teaching through WhatsApp may be a great way to supplement teaching internally and across different residency programs.
Through our WhatsApp experience, and through feedback from residents we learnt a lot, and suggest several points in order to maintain a successful social media platform for education. First, there must be a champion from both the learners and teachers that continues to facilitate the group discussions. Second, it is crucial to take into account the timing, complexity, and amount of material delivered in one as not to overwhelm trainees. Third, one must not be discouraged by the number of responses as this tends to improve over time and should always seek feedback from trainees and faculty on how to improve response rate. Trainees have a variable schedule in terms of how busy they are with an hour to an hour and day-to-day differences. It is important to take that into account when posting learning material and choose “off-peak” hours such as rounding, and conference times. Fourth, like any other method of teaching, this should be a step-up approach and starting with common than more challenging EKGs. Finally, and most importantly, the institution must always seek feedback from participants on how to improve the method of delivery of education, and what can be done to further enhance the experience.
Limitations
The main limitation of the study is the small sample size. Also, the study was conducted in a single academic medical institute and didn’t involve all medical subspecialties who usually are involved in the ECG interpretation like critical care fellows and emergency medicine residents. In addition, the utility and effectiveness of teaching through WhatsApp was not evaluated in this study, however, this is currently being evaluated in a more longitudinal way in the internal medicine program at SIU.
Declarations
Ethics approval and consent to participate
This survey and the research protocol were reviewed by the Springfield Committee on Research Involving Human Subjects (CHRIS) and was determined that it does not fall under the purview of the IRB as research involving human subjects according to 45 CFR 46.101 and 45 CFR 46.102. (Ref: 018276).
Individual consent to participate in the survey was obtained as part of the survey in written format.
Consent for publication: Not applicable
Availability of data and material
All results of questionnaires and data acquisition may be provided upon request. All data has been gathered through an anonymous day, with no link to individual participants.
Competing interests: All authors declare no competing interests
Funding: This project lacked funding
Authors' contributions: All authors made substantial contributions to this work. The design was done by M.A, M.L., A.A. Data acquisition was obtained and facilitated through, C.K., Data analysis was done by R.R., and M.S. Manuscript writing and review was done by M.A., M.B, M.S, A.A, and R.R.
Conclusion: Training in EKG interpretation remains lacking and unstructured. The ideal way to teach and learn EKG interpretation remains unknown. EKG interactive teaching via WhatsApp may be used as a possible format for teaching ECG.
Acknowledgments: We thank SIU residents and faculty for their participation in the group and surveys and thank Professor Chami (Program director of cardiology fellowship) for his support of the project.
References
- Doost Hosseiny A, Moloi S, Chandrasekhar J, Farshid A (2016) Mortality pattern and cause of death in a long-term follow-up of patients with STEMI treated with primary PCI. Open Heart. 3(1): e000405.
- Al-Akchar M, Sawalha K, Al-Khadra Y, Kittleson M, Missula V, et al. (2021) Outcomes of cardiogenic shock with autoimmune rheumatological disorders. Cardiovascular Revascularization Medicine.
- Sawalha K, Abozenah M, Kadado AJ, Battisha A, Al-Akchar M, et al. (2020) Systematic review of COVID-19 related myocarditis: insights on management and outcome. Cardiovascular Revascularization Medicine. 23: 107-113.
- Battisha A, Sawalha K, Altibi AM, Madoukh B, Al-Akchar M, et al. (2020) Cardiogenic shock in autoimmune rheumatologic diseases: an insight on etiologies, management, and treatment outcomes. Heart failure reviews. 20: 1-9.
- Battisha A, Sawalha K, Madoukh B, Sheikh O, Doughem K, et al. (2020) Acute Myocardial Infarction in Systemic Mastocytosis: Case Report with Literature Review on the Role of Inflammatory Process in Acute Coronary Syndrome. Current cardiology reviews. 16(4): 333-337.
- Isiguzo GC, Iroezindu MO, Muoneme AS, Okeahialam BN (2017) Knowledge and utilization of electrocardiogram among resident doctors in family medicine in Nigeria. Nigerian journal of clinical practice. 20(9): 1133-1138.
- Hartman ND, Wheaton NB, Williamson K, Quattromani EN, Branzetti JB, et al. (2016) A Novel Tool for Assessment of Emergency Medicine Resident Skill in Determining Diagnosis and Management for Emergent Electrocardiograms: A Multicenter Study. J Emerg Med. 51(6): 697–704.
- Hillson SD, Connelly DP, Liu Y (1995) The effects of computer- assisted electrocardiographic interpretation on physicians’ diagnostic decisions. Med Decis Making. 15(2): 107–12.
- Fent G, Gosai J, Purva M (2015) Teaching the interpretation of electrocardiograms: which method is best? J Electrocardiol. 48(2): 190-3.
- Crumlish CM, Yialamas MA, McMahon GT (2009) Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 4(5): 304-7.
- Sawalha K, Al-Ali M, Sawalha A, Ko H, Abdelli I, et al. (2017) Factors influencing academic motivation among UOS medical students. Journal of Health Science. 5: 177-180.
- Fordtran JS, Armstrong WM, Emmett M, Kitchens LW, Merrick BA (2004) The history of internal medicine at Baylor University Medical Center, part 1. Proc (Bayl Univ Med Cent). 17(1): 9– 22.
- Coleman E, O'Connor E (2019) The role of WhatsApp® in medical education; a scoping review and instructional design model. BMC Med Educ. 19(1): 279.
- Antiperovitch P, Zareba W, Steinberg JS, Bacharova L, Tereshchenko LG, et al. (2018) Proposed in-trainingelectrocardiogram interpretation competencies for undergraduate and postgraduate trainees. J Hosp Med. 13(3): 185–193.
- Eslava D, Dhillon S, Berger J, Homel P, Bergmann S (2009) Interpretation of electrocardiograms by first-year residents: the need for change. J Electrocardiol. 42(6): 693–7.
- Garvey JL, Zegre-Hemsey J, Gregg R, Studnek JR (2016) Electrocardiographic diagnosis of ST segment elevation myocardial infarction: An evaluation of three automated interpretation algorithms. J Electrocardiol. 49(5): 728–732.
- Martínez-Losas P, Higueras J, Gómez-Polo JC, Brabyn P, et al. (2016) The influence of computerized interpretation of an electrocardiogram reading. Am J Emerg Med. 34(10): 2031– 2032.
- Mele PF (2008) The ECG dilemma: guidelines on improving interpretation. J Healthc Risk Manag. 28(2): 27–31.
- Anh D, Krishnan S, Bogun F (2006) Accuracy of electrocardiogram interpretation by cardiologists in the setting of incorrect computer analysis. J Electrocardiol. 39(3): 343– 345.
- Bogun F, Anh D, Kalahasty G, Wissner E, Serhal CB, et al. (2004) Misdiagnosis of atrial fibrillation and its clinical consequences. Am J Med. 117(9): 636–42.
- Raiman L, Antbring R, Mahmood A (2017) WhatsApp messenger as a tool to supplement medical education for medical students on clinical attachment. BMC Med Educ. 17(1): 7.
- Kochar A, Rymer J, Samad Z, Duke Cardiovascular Education Group (2018) Disrupting fellow education through group texting: WhatsApp in fellow education? J Am Coll Cardiol. 72(25): 3366–3369.