Kshma Rao1*, Gowri Bhandarkar2, Raghavendra Kini3, Roopashri Kashyap4, Ujwala Shetty5, Meghana HC6
1Post Graduate Student, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
2Reader, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
3Professor and Head, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
4Professor, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
5Reader, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
6Reader, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India
*Corresponding Author: Kshma Rao, Post Graduate Student, Oral Medicine & Radiology, A.J Institute of Dental Sciences, Kuntikana, Mangaluru 575004, Karnataka, India.
Abstract
Philipsen first described Odontogenic keratocyst (OKC). It is presently known as a Keratocystic odontogenic tumor (KCOT). They are the most common of developmental or inflammatory origin. Patients will often complain of swelling or discharge. OKC occurring in between the roots of the premolars is called lateral OKC. This may resemble a lateral periodontal cyst or lateral radicular cyst.
Keywords: Odontogenic keratocyst, swelling, OKC
Introduction
Philipsen first described Odontogenic keratocyst (OKC). It is presently known as a Keratocystic odontogenic tumor (KCOT). They are the most common of developmental or inflammatory origin. [1] Multiple OKCs may be associated with Nevoid basal cell carcinoma syndrome. Most keratocyst occurs in the mandible but may occur in any part of the jaw. It is seen happen in the 2nd and 3rd decade of life. [2] Radiographically, it may appear as unilocular or multilocular radiolucency with a corticated border. [3] At this moment, we report a case of lateral odontogenic cyst of the posterior mandibular region.
Case Report
A healthy 45-year-old male patient visited our department with a complaint of swelling in the lower left jaw region for 2 months and swelling gradually increased in size with a history of pus discharge and associated pain. Diffuse swelling was noted on the left lower third of the face extending from the upper lip to the inferior border of the mandible super inferiorly, mediolaterally from the angle of the mouth to 3 cm away from the tragus of the ear. Swelling measured 4x3cm and was firm in consistency. Intraoral examination revealed swelling in the left mandibular vestibular region extending from 34 to 37, measuring 3x3cm. The swelling was non-tender, lobulated, and firm in consistency.
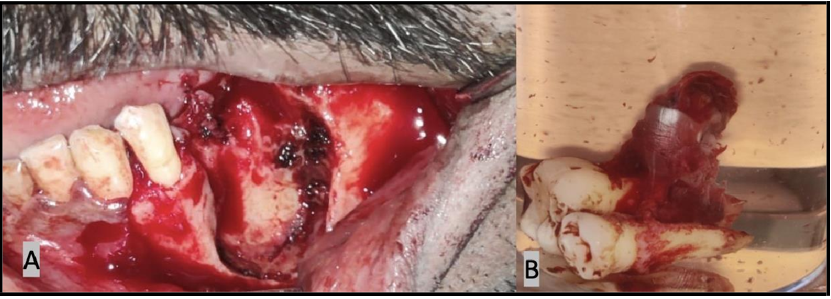
The overlying mucosa was normal. [Figure 1] The patient was advised for a mandibular lateral occlusal radiograph that revealed no buccolingual expansion of the cortical plate. [Figure 2] We advised an orthopantomogram to check for the extension of the swelling that indicated unilocular, teardrop-shaped radiolucency [Figure 3] extending from 35 to the middle third of 36 with no root resorption. Based on the clinical and radiologic examination, a provisional diagnosis of Odontogenic keratocyst was given. Differential diagnoses considered were lateral periodontal cyst and radicular cyst. The contents of the swelling were aspirated [Figure 4] and sent for investigation, the result of which was consistent with the diagnosis of the cystic lesion. Enucleation of the lesion, along with the removal of involved teeth, was carried out. [Figure 5] The specimen was then sent for histopathological examination. Histopathological examination revealed cystic lining of stratified squamous Para keratinized epithelium having 6-8 layers of thickness without rete pegs. Basal cells were tall columnar and had palisading arrangements showing a characteristic tombstone appearance. Focal areas of chronic inflammatory cell infiltration were also evident. The above features were suggestive of infected lateral odontogenic keratocyst.
Figure 1: Intraoral view depicting the buccal cortical plate expansion of left side
Figure 2: Mandibular lateral occlusal radiograph reveals no bucco-lingual expansion
Figure 3: Orthopantogram reveals unilocular, tear-shaped radiolucency
Figure 4: Fine needle aspiration reveals creamy white aspirate intermixed with blood
Figure 5: A) Enucleation along with the extraction of involved teeth B) Specimen
Discussion
OKC is an odontogenic cyst with an aggressive nature and high recurrence rate. [4] Keratocyst is a jaw cyst that contains keratin. It was previously known as a primordial cyst, which was believed to have primordial odontogenic epithelium. Pronounced peak frequency is seen in the 2nd and 3rd decades of life. They are generally found more in males than females. [5] In 70 % of the cases, the mandible is involved, particularly in the angle, ramus, third molar, and premolar region. In the maxilla, it may be observed in the third molar and the canine area. [6] In our reported case, the patient was a male of age 45 years, and the lesion was observed in the mandibular premolar region. Locally destructive lesions occur intrabony and tend to enlarge before it appears as a swelling buccolingually, thus preventing an early diagnosis of any underlying lesion. Multiple odontogenic keratocysts of the jaws, along with vertebral and rib anomalies and intracranial calcification, are observed in Nevoid basal cell carcinoma syndrome. [7] Our case did not have any manifestations of Nevoid basal cell carcinoma syndrome.
Patients will often complain of swelling or discharge. Some may experience paresthesia of the lower lip or teeth. Some may not be aware until they develop pathologic fractures. [2] Our patient experienced painful swelling with a history of discharge and no other symptoms.
OKC occurring in between the roots of the premolars is called lateral OKC. This may resemble a lateral periodontal cyst or lateral radicular cyst. [8]
According to Fantasia, eight of the 46 lateral periodontal cysts were OKC. Gold et al. discovered 6 OKCs out of the 32 cases. Brannon found that out of 82 cysts occurring in lateral periodontal locations, 20 were OKC. OKC is characterized by a 4-8 layer thick epithelium devoid of rete ridges. Columnar or cuboidal basal cells with a palisading arrangement may be observed. The cystic lumen is often filled with desquamated keratin. Keratin is usually parakeratin, but occasionally orthokeratinization may be evident. Within the cystic wall, small daughter cells are frequently found. A lateral periodontal cyst is characterized by a 1-3 layer thick nonkeratinized epithelium with glycogen-rich clear cells. [9] In the present case, OKC was observed between the mandibular premolar roots. Histologically, it was characterized by a 6-8 layer thick parakeratinized epithelium, devoid of rete pegs, and basal cells were tall columnar having palisading arrangement.
Recurrence of keratocyst may be due to the residue of the original cystic lining post-surgery, from one or more satellite cysts escaping enucleation, or from remnants of dental lamina outside the original capsule of the cyst. [10]
Conclusion
Lateral OKC can appear as a diagnostic ultimatum as it is often misinterpreted as a lateral periodontal cyst. Hence, careful examination and a good number of differential diagnoses must be included to rule out the occult odontogenic keratocyst.
References
- Soni PK, Choudhary B, Vashistha V, Sinha P (2021) Odontogenic Keratocyst in Posterior Mandible: A Case Report. Int J Sci Stud. 9(1): 4-7.
- Kanth K, Uppala D, Majumdar S (2016) Lateral Odontogenic Keratocyst mimicking Periodontal Cyst: A Case Report and Review. Oral Maxillofac Pathol J. 7(2): 758-760.
- Elnouaem MI, El Sayed Darwish Z, Aly Sharaf R (2016) An unusual presentation of odontogenic keratocyst with malignant changes in a 13-year-old girl. Int J Case Rep Images. 7(10): 657– 661.
- Neville BW, Damm DD, Allen CM, Bouquot JE (2009) Oral and Maxillofacial Pathology. 3 ed. St. Louis: Mosby, Elsevier.
- Shear M, Speight P (2007) Cysts of the Oral and Maxillofacial Regions. 4th Edn.; Blackwell Publishing Ltd. 59 78.
- Khalam AS, Zacariah RK (2012) Underdiagnosis of an odontogenic keratocyst-a controversial lesion. IOSR J Dent Med Sci. 2(5): 37-40.
- Dowling PA, Fleming P, Saunders ID, Gorlin RJ, Napier SS (2000) Odontogenic keratocysts in a 5-year-old: initial manifestations of nevoid basal cell carcinoma syndrome. Pediatr Dent. 22(1): 53–5.
- Pindborg JJ, Hansen J (1963) Studies on odontogenic cyst epithelium. Clinical and roentgenology aspects of odontogenic keratocysts. Acta Pathol Microbiol Scand. 58: 283-294.
- Neville BW, Mishkin DJ, Traynham RT (1984) The Laterally Positioned Odontogenic Keratocyst: A Case Report. Journal of Periodontology, 55(2): 98–102.
- Toller PA (1972) Newer concepts of odontogenic cysts. International Journal of Oral Surgery. 1(1): 3–16.