Ali Sreij MD*, Nabil Ammouri MD, Raja Sawaya MD
Department of Neurology, American University of Beirut Medical Center, Beirut, Lebanon.
*Corresponding Author: Ali Sreij MD, Fellow, Department of Neurology, American University of Beirut Medical Center, Beirut, Lebanon.
Abstract
Isolated sciatic mononeuropathy is a rare disorder and is usually secondary to a pathology. The diagnosis is done by the patient’s history, physical examination, MRI imaging and electrophysiological studies. Etiologies for a sciatic mononeuropathy are usually traumatic, tumoral, or iatrogenic. Idiopathic isolated sciatic mononeuropathies are rarely reported and are usually in the pediatric population or young adults. We describe the case of an idiopathic isolated sciatic mononeuritis in an elderly man misdiagnosed for 8 years as monomeric amyotrophic lateral sclerosis. The diagnosis was then made by electrophysiological studies confirming a sciatic nerve lesion rather than a motor neuron pathology.
Keywords: sciatic nerve, mononeuropathy, ALS, EMG, neuritis.
Introduction
Isolated sciatic nerve lesion is a rare phenomenon. It is usually caused by a pathology in the pelvis, hip, or lumbosacral plexus with only few anecdotal cases reports of idiopathic etiology. For this reason, patients who present with symptoms and signs related to the sciatic nerve are usually easily diagnosed by clinical, radiologic, and electrophysiological studies and receive treatment accordingly. We describe a patient who suffered from weakness and muscle atrophy in one leg for more than 8 years and was diagnosed as suffering from monomeric amyotrophic lateral sclerosis (ALS). When the patient’s condition failed to progress an extensive EMG study was done and diagnosed an isolated sciatic nerve lesion. Repeat MRI imaging suggested a neuritis of the sciatic nerve. The condition was labeled idiopathic as all related studies were normal.
Case Report
We report the case of an elderly man who had been suffering from progressive weakness of the muscles of the left lower extremity for more than 8 years. The weakness involves the proximal as well as the distal muscles. The patient denies any pain, numbness, paresthesia, or anesthesia in the left lower extremity. He denied back pain or any symptoms in the right lower extremity or the upper extremities. He had no sphincter or erectile dysfunction. The symptoms have been progressing slowly resulting in an unsteady gait requiring assistance. At the time of diagnosis the patient had undergone MRI of the lumbosacral spine and lumbosacral plexus which were reported to be within normal limits for age. EMG done at that time was also reported normal.
The patient presented for a second opinion 8 years later. On neurologic examination, he had intact mental status and cognitive functions. He had normal cranial nerves and speech. He had no dysphagia, dysarthria, or diplopia. The neurological examination of the upper extremities and right lower extremity were normal. The quadriceps, hamstrings, tibialis anterior, and gastrocnemius muscles in the left lower extremity were weak against resistance and atrophic. The patient had a normal sensory exam for light touch, pain, vibration, and proprioception in all four extremities. He had normal and symmetrical deep tendon reflexes in the lower extremities with absent Babinski signs.
Nerve conduction studies and electromyography were then performed on the upper and lower extremities. The results showed slightly decreased motor amplitudes in the left posterior tibial nerve compared to the right with a slight delay in the proximal and distal latencies. The posterior tibial F-responses were asymmetrical with dispersed responses on the left side with the presence of A-waves (Figure 1). Normal motor neurographies of the peroneal nerves bilaterally and the right posterior tibial nerve. The sensory sural amplitude was significantly and consistently lower in the left leg compared to the right. The superficial peroneal sensory responses were present and symmetrical in both lower extremities. Normal motor and sensory neurographies of the median and ulnar nerves bilaterally.
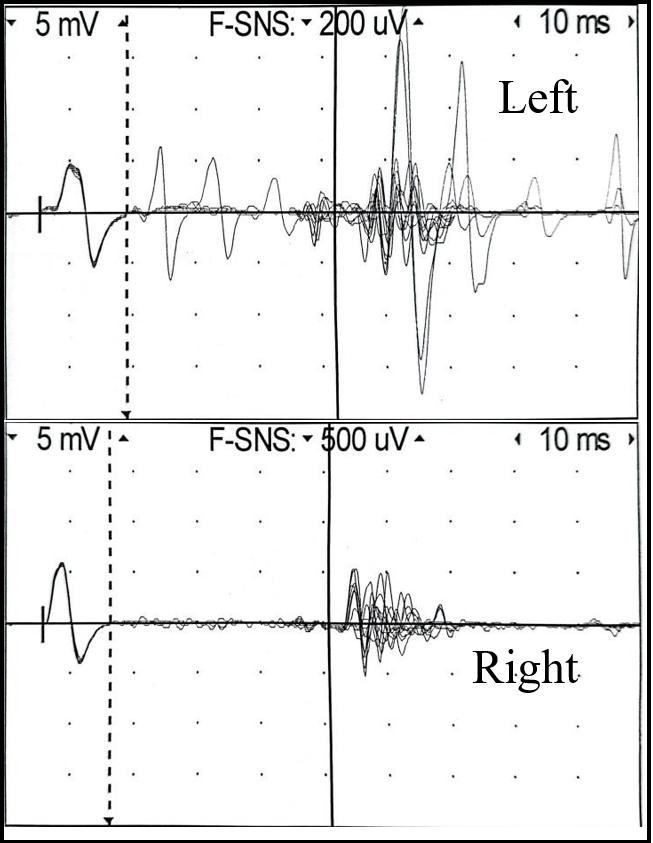
Figure 1: A scheme showing the posterior tibial F-waves asymmetry.
The concentric needle EMG examination revealed chronic neurogenic changes in the left tibialis anterior muscle with the absence of spontaneous activity and decreased recruitment pattern. Normal motor units seen in the left peroneus longus, medial gastrocnemius, vastus medialis and rectus femoris. The recruitment of motor units in these muscles was also significantly reduced with the absence of spontaneous activity. The conclusion of the electrophysiological study was compatible with a moderate chronic left sided sciatic nerve lesion with affection of the motor fibers as well as the sensory fiber of the sural nerve. The definite involvement of the sural nerve places the lesion in the lumbosacral plexus rather than the lumbosacral root region and negates the electrophysiological diagnosis of a motor neuron disease. (Table 1)
Table 1: Nerve conduction studies.
|
|
DL (ms) |
Amplitude (mV) |
CV (m/s) |
|
Tibial MNC |
|||
|
Ankle (L) |
4.9 |
7.4 |
|
|
Knee (L) |
14 |
6.7 |
46 |
|
Ankle (R) |
4.2 |
10.2 |
|
|
Knee (R) |
12.7 |
8.5 |
46 |
|
Peroneal MNC |
|||
|
Ankle (L) |
3.7 |
5.5 |
|
|
Fibular Head (L) |
13.7 |
5.0 |
40 |
|
Ankle (R) |
3.2 |
4.3 |
|
|
Fibular Head (R) |
13.1 |
4.3 |
40 |
|
Sural SNC |
|||
|
Ankle (L) |
4.0 |
2 |
35 |
|
Ankle (R) |
2.8 |
15 |
39 |
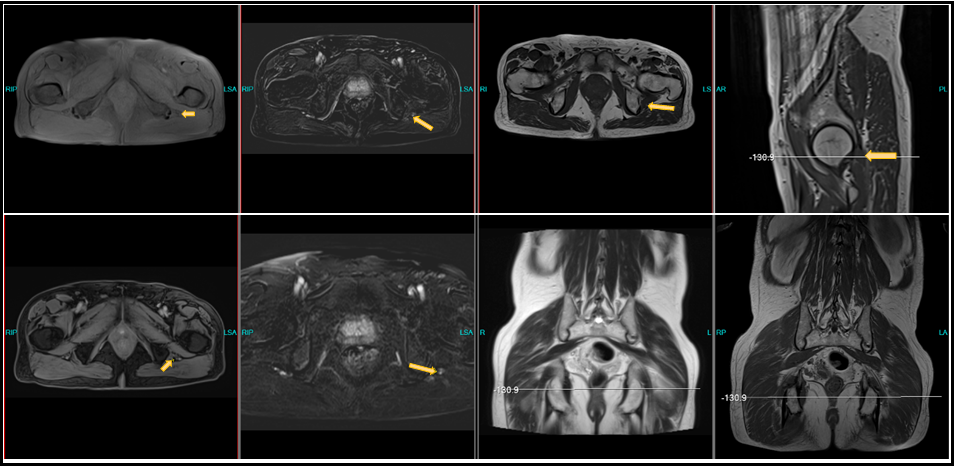
With the above electrophysiological findings, the patient underwent a repeat MRI of the lumbosacral plexus with thin cuts and intravenous gadolinium. The result revealed a normal left genitofemoral and obturator nerves. Both piriformis muscles were symmetric and normal and the superior and inferior gluteal nerves were symmetrical. There was squeezing of the left sciatic nerve in between the left obturator internus and left gluteus maximus muscles in between normal space of the left ischial tuberosity and lesser trochanter area.
Post intravenous injection of contrast material showed a mild enhancement of the sciatic nerve at the site of stenotic area compatible with neuritis. The sciatic nerve distally in the upper thigh was normal. The right and left femoral nerves were symmetrical (Figure 2).
A complete battery of blood studies including serum vasculitis studies and anti-ganglioside antibody titers were normal. CSF studies were normal.
Figure 2: Lumbosacral plexus MRI showing the involvement of the left sciatic nerve.
Discussion
Mononeuropathies of the sciatic nerve has been defined in the literature. Schwannomas of the sciatic nerve are rare but reported. They present with pain and weakness in the area innervated by the sciatic nerve and its branches. MRI imaging can differentiate benign from malignant nerve sheath tumors of the sciatic nerve. Treatment is usually surgical excision and in rare cases radiotherapy [1].
Lipomatosis of the sciatic nerve, also known as lipofibromatous hamartoma, is an even rarer pathology. These pathologies present with abnormal motor nerve conduction studies with definite sensory sural nerve involvement guiding the clinician to search for a pathology in the lumbosacral plexus. Treatment is surgical excision. [2]
Entrapment of the sciatic nerve in the muscles of the pelvis is often reported as the deep gluteal syndrome. This includes the priformis syndrome, the gemelli-obturator internus syndrome, the ischiofemoral impingement syndrome, and the proximal hamstring syndrome [3]. These entities are usually diagnosed by a careful history taking and physical examination. The diagnosis is usually delayed as clinicians tend to think the reason for the patients’ symptoms and signs is a lumbosacral disc disease. Time is lost with repeated imaging and physical therapy. These entities may not be evident by radiographic studies of the pelvis, but rather show up on abnormal nerve conduction studies with specific pathology involving the post-ganglionic sensory fibers [3,4,5].
Traumatic lesions of the sciatic nerve can be seen after intramuscular injections in the gluteus maximus muscle. These occur usually in unexperienced hands or in the population with poorly constructed buttocks such as small children or elderly patients. Education of healthcare providers is essential in avoiding these iatrogenic injuries of the sciatic nerve [6].
The sciatic nerve can also be injured after hip surgery or hip arthroplasty. These can occur either acutely intraoperatively from retraction trauma to the sciatic nerve or can occur chronically after fibrosis and scar tissue formation [7].
Idiopathic sciatic mononeuropathies are labelled so after extensive investigation for etiologies is exhausted. To our knowledge, there are only few reports of idiopathic sciatic mononeuropathies [8,9]. These cases are more frequent in the pediatric population or the young adults. They are diagnosed by the clinical picture and abnormal nerve conduction studies and normal MRI imaging of the spine and pelvis. [10].
It is important to diagnose sciatic mononeuropathies precisely as the clinical condition of the patient is functionally disturbed and usually these neuropathies have a treatable etiology. These rare cases of idiopathic sciatic mononeuropathies amount to 6-10% of all cases of sciatic nerve lesions described in the literature [9]. The diagnosis of this entity is important to avoid unnecessary medical treatment and surgical interventions.
Declarations
Ethics approval and consent to participate: Consent approved by the patient.
Consent for publication: All patients consented to the study protocol and collection of data.
Disclosure:
Ali Sreij M.D. and Raja Sawaya M.D. have no conflicts of interest, and they did not receive any funding for this work.
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
References
- Telera S, Raus L, Vietti V, Pace A, Villani V, et al. (2020) Schwannomas of the sciatic nerve: A rare and neglected diagnosis. A review of the literature with two illustrative cases. Clin Neurol Neurosurg. 195: 105889.
- Fandridis EM, Kiriako AS, Spyridonos SG, Delibasis GE, Bourlos DN, et al. (2009) Lipomatosis of the sciatic nerve: report of a case and review of the literature. Microsurgery. 29(1): 66-71.
- Park JW, Lee YK, Lee YJ, Shin S, Kang Y, et al. (2020) Deep gluteal syndrome as a cause of posterior hip pain and sciatica-like pain. Bone Joint J. 102-B(5): 556-567.
- Cass SP (2015). Piriformis syndrome: a cause of nondiscogenic sciatica. Curr Sports Med Rep. 14(1): 41-4.
- Marco C, Miguel-Pérez M, Pérez-Bellmunt A, Ortiz-Sagristà JC, Martinoli C, et al. (2019) Anatomical causes of compression of the sciatic nerve in the pelvis. Piriform syndrome. Rev Esp Cir Ortop Traumatol (Engl Ed). 63(6): 424-430.
- Kadioglu HH (2018) Sciatic Nerve Injuries from Gluteal Intramuscular Injection According to Records of the High Health Council. Turk Neurosurg. 28(3): 474-478.
- Regev GJ, Drexler M, Sever R, Dwyer T, Khashan M, et al. (2015) Neurolysis for the treatment of sciatic nerve palsy associated with total hip arthroplasty. Bone Joint J. 97-B(10): 1345-9.
- Engstrom JW, Layzer RB, Olney RK, Edwards MB (1993) Idiopathic, progressive mononeuropathy in young people. Arch Neurol. 50(1): 20-3.
- Sawaya RA (1999) Idiopathic sciatic mononeuropathy Clinical Neurology and Neurosurgery. 101(4): 256–259.
- Srinivasan J, Ryan MM, Escolar DM, Darras B, Jones HR (2011) Pediatric sciatic neuropathies: a 30-year prospective study. Neurology. 76(11): 976-80.