Sanjana Santhosh Kumar, B.D.S.1, Hima Bindu Reddy.C, B.D.S.2*, Elavenil Panneerselvam, MDS, MBA, FAM, FDS RCPSG3, Bharathwaj.V.V, MDS4, Krishna Kumar Raja.V. B, MDS5
1Private practice, Residency at Eastman Institute of Oral Health University of Rochester, New York, USA. Orcid number: 0000-0001-5902-3934
2private practitioner, Chennai, India. Orcid number: 0000-0002-2664-7828
3Department of Oral & Maxillofacial Surgery, SRM Dental College & Hospital, Ramapuram Campus, Ramapuram, Chennai, India. Orcid number: 0000-0002-9930-3292
4Department of Public Health Dentistry, SRM Dental College & Hospital, Ramapuram Campus, Ramapuram, Chennai, India. Orcid number: 0000- 0002-9915-9323
5professor & HOD Department of Oral & Maxillofacial Surgery, SRM Dental College & Hospital, Ramapuram Campus, Ramapuram, Chennai, India. Orcid number: 0000-0002-1220-4081
*Corresponding Author: Hima Bindu Reddy.C, B.D.S., private practitioner, Chennai, India. Orcid number: 0000-0002-2664-7828.
Abstract
Objectives: To develop a hand sign manual for effective patient-dentist communication during dental procedures.
Materials and Methods: This prospective cross-sectional study recruited 260 patients who reported for dental treatment in October 2019. The 6 hand signs developed by the authors were taught to patients for use during dental treatment. A questionnaire consisting of 5 questions aimed at understanding the importance and efficacy of the hand sign manual was designed. The questionnaire obtained patient feedback regarding hand signs before and after treatment. Statistical analysis was performed with Chi-Square and Fisher’s exact tests.
Results: 254 patients (95 males and 159 females) who appropriately completed the questionnaire were considered for statistical evaluation. Of the total sample size, 61.1% were literate, and 38.9% were illiterate. Statistically, it was found that 97.2% of patients (literate 95% and illiterate 100%) appreciated the need to learn hand signs (p-value 0.04). The importance of hand signs for communication with dentists and the ease of usage was appreciated by patients irrespective of literacy and gender.
Conclusion: The use of hand signs is a necessary practice for effective communication during dental treatment.
Keywords: questionnaire study, hand signals, dental clinic, patient-dentist communication, dental procedures, anxiety
Introduction
Among the various treatment modalities, dental procedures have been cited by many as a significant cause for provoking fear and anxiety. [1,2,3] This is greatly attributed to the potentially pain-inducing procedures and complex armamentarium used for treatment. The inability of patients to speak or express themselves for any clarification during treatment also instills fear of great magnitude.[4] A dentist may significantly reduce this anxiety by establishing good communication with the patient and exercising empathy towards patients’ varied expressions.[5] Good communication between the patient and dentist benefits the patient, dentist, and the entire dental team by achieving many objectives: (1) a proper understanding of the clinical problem through the description of symptoms by patients,[6] (2) clear expression of doctor’s concern towards patients which alleviates their anxiety,[7,8] (3) eliminating the fear of dental procedures by a proper explanation of the same, [9,10] and (4) improvement in dentists’ decision-making ability and sensitivity toward patients’ emotion.[11,12] Further, effective communication between a patient and the dentist increases the accuracy of diagnosis with less likelihood of litigations. [13] Proper communications also ensure better patient cooperation towards treatment and increases patient satisfaction. [14,15] In contrast, a loss of 25% of patients has been reported in the literature over 5 years due to poor dentist-patient communication.[6] Better communication is, therefore, necessary at every stage of patient management, before, during, and after treatment.[16]
Various modes of patient-dentist communication mentioned in the literature include verbal, auditory, visual, and written methods. [6] The patient-dentist communication “before” a dental procedure is predominantly “verbal,” and its implementation is straightforward. [14,17] However, verbal communication “during” the procedure is complex, especially in a dental clinic, where the area of instrumentation is the oral cavity, which precludes verbal expression of patients’ feelings or thoughts. It is often challenging to elicit responses to even the simplest of questions, like “Are you all, right?”. It is difficult for patients to move their heads in response or speak with an instrument inside their mouth. This may lead to misinterpretation of a patient’s response or increase the duration of the treatment because of frequent interruptions to communicate verbally. To overcome the problems mentioned above, literature shows that hand signs may be used as an effective mode of communication.[16] Hand signs constitute a particular form of language in conveying socially pertinent information to the other person. [18,19] They are simple gestures commonly used by people with impaired hearing or speaking abilities. [20,21] Goldin-Meadow et al. [20] stated that these sign gestures are as effective as verbal expressions. In specific clinical scenarios, hand gestures have also been very helpful for healthcare workers to improve sterile working environments.[22] However, the use of hand signs during dental treatment is less recognized and practiced. [16] Therefore, the primary aim of this study was to develop a clinically effective and user-friendly manual of hand signs to be utilized “during” dental treatments. This study also assessed the effectiveness of the authors’ manual of hand signs and patient’s perception of its usage based on literacy and gender.
Materials and Methods
Study Design
To fulfil the stated objectives of the study, a prospective cross- sectional study was conducted, which involved 254 outpatients of the Department of Oral and Maxillofacial Surgery, SRM Dental College, Chennai, India, in October 2019. Ethical clearance to conduct the study was obtained from the Institutional Review Board (SRMU/M&HS/SRMDC/2020/S/016). Patients between the ages of 18 and 50 years with a good orientation of mind and with previous history of dental procedures were included in the study. Exclusion criteria consisted of patients with disabilities related to hearing and vision. Patients who were mentally challenged and without previous exposure to dental treatments were also excluded. The sample size was determined using G power software for Chi Square contingency tables, estimated to be 246. The power was set to 95%, and the effect size was set to 0.2, with a p-value of 0.05 showing significance. The recruited patients were informed about the study, and consent was obtained.
Development of "SRM hand signs manual."
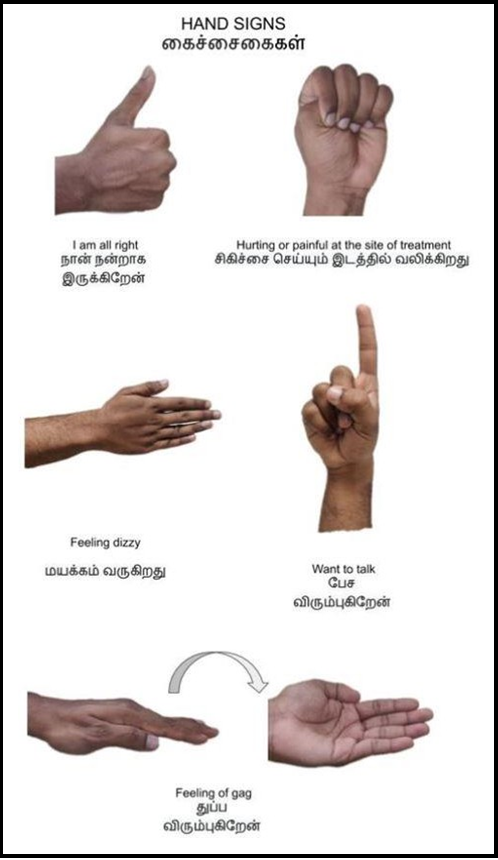
A manual of hand signs was developed based on existing literature and validated by a pilot study. The manual included 6 signs, each indicating a specific patient response (Figure 1). Descriptions of each hand sign were bilingual (English and Tamil).
Figure 1 SRM Hand signs
Development of questionnaire
The questionnaire consisted of 5 questions about the need to communicate with the dentist and use hand signs during dental treatment. The questions were bilingual (English and Tamil) and designed to elicit binary responses (Yes or No). Questions 1 and 2 focused on patients' perceptions regarding the necessity of communicating with the dentist during treatment and the need to learn hand signs. Question 3 was regarding the patient's previous experience, while questions 4 and 5 were related to patients' opinions regarding our hand sign manual. Experts verified the validity of the questionnaire, and it met all the face and content validity criteria.
Implementation
Hand signs were taught before treatment, and the patients were encouraged to use the same signs during their dental procedures. The patients were instructed to give their responses by filling out the questionnaire. The responses to questions 1, 1,2, and 3 were filled before the commencement of treatment and use of hand signs, while the responses to questions 4 and 5 were recorded after using hand signs. The responses were filled by the authors for illiterate patients. Only those responses where all questions were answered were considered valid and included in the subsequent statistical analysis.
Statistical analysis
A Chi-Square test was applied to compare proportions between groups. Fisher's exact test was used if any expected cell frequency was less than five. To analyze the data, SPSS (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY: IBM Corp. Released 2019). The significance level was fixed as 5% (α = 0.05).
Results
260 patients were reported to the Department of Oral and Maxillofacial Surgery. Responses from 6 were excluded because of incomplete or multiple responses, culminating in a study sample of 254 participants.
Descriptive statistics
The mean age of the patients was 27.5 years. The gender-wise distribution of the sample consisted of 95 males (37.4%) and 159 females (62.6%). The distribution of literate and illiterate patients was 61.1% and 38.9%, respectively.
Response of patients based on literacy:
Regarding the need for intra-operative communication, 83.8% of the illiterate and 80% of the literate patients felt it was necessary, while when assessing the importance of hand signs, all the illiterate patients were affirmative, and only 95% of the literate felt so which was statistically significant (p=0.045). It was found that a higher percentage of literate patients had prior experience in using hand signals during dental treatment when compared to illiterate patients (Table 1). The illiterate patient population felt that the hand signals were easy to memorize and found it helpful during the treatment duration against a marginally lower literate population.
Table 1: Comparing proportions between illiterates and literates using Chi-Square test.
|
Sl No |
Questions |
Illiterate (N=99) |
Literate (N=155) |
Total (N=254) |
Statistical Analysis |
|||
|
Yes |
No |
Yes |
No |
Yes |
No |
|||
|
Q1 |
Need for intra-operative communication. |
83 83.8% |
16 16.2% |
124 80.0% |
31 20.0% |
207 81.5% |
47 18.5% |
0.442 |
|
Q2 |
Importance of hand signs |
99 100% |
0 0.0% |
148 95.5% |
7 4.5% |
247 97.2% |
7 2.8% |
0.045* |
|
Q3 |
Use of hand signals in previous dental treatments |
37 37.4% |
62 62.6% |
70 45.2% |
85 54.8% |
107 42.1% |
147 57.9% |
0.220 |
|
Q4 |
Ease of memorising hand signs |
99 100.0% |
0 0.0% |
150 96.8% |
5 3.2% |
249 98.0% |
5 2.0% |
0.160* |
|
Q5 |
Usefulness of hand signs |
99 100.0% |
0 0.0% |
153 98.7% |
2 1.3% |
252 99.2% |
2 0.8% |
0.522 |
*Fisher’s exact test
Response of patients based on gender:
Of the 254 patients, 160 were females (63%), and 84 were male (37%). A higher percentage of male patients elicited a need for intra- operative communication, which was statistically significant (p=0.032) and supported its importance, while a higher number of female patients provided a history of using hand signals in earlier instances (Table 2). Both genders demonstrated comparable results for the post-exposure evaluation of assessing the ease of memorizing and the usefulness of hand signals.
Table 2: Comparing proportions between males and females using Chi-Square test.
|
Sl No |
Questions |
Male (N=84) |
Female (N=160) |
Total (N=254) |
Statistical Analysis |
|||
|
Yes |
No |
Yes |
No |
Yes |
No |
|||
|
Q1 |
Need for intra-operative communication |
83 88.3% |
11 11.7% |
124 77.5% |
36 22.5% |
207 81.5% |
47 18.5% |
0.032 |
|
Q2 |
Importance of hand signs |
92 97.9% |
2 2.1% |
155 96.9% |
5 3.1% |
247 97.2% |
7 2.8% |
0.999* |
|
Q3 |
Use of hand signals in previous dental treatments |
35 37.2% |
59 62.8% |
72 45.0% |
88 55.0% |
107 42.1% |
147 57.9% |
0.226 |
|
Q4 |
Ease of memorising hand signs |
92 97.9% |
2 2.1% |
157 98.1% |
3 1.9% |
249 98.0% |
5 2.0% |
0.999* |
|
Q5 |
Usefulness of hand signs |
93 98.9% |
1 1.1% |
159 99.4% |
1 0.6% |
252 99.2% |
2 0.8% |
0.999* |
*Fisher’s exact test
Discussion
Dental appointments are considered the most dreadful experience by many. Many studies have focused on the impact of pre and postoperative communication between a patient and dentist in reducing patient apprehension. [23,24,25] However, the role of intra- operative communication, which is clinically significant, needs to be discussed more in the literature. The intra-operative interaction between a dentist and a patient is more crucial because, during this phase, a patient’s fear, anxiety, or confusion increases manifold due to the sight or noise of instruments. The ability of the patient to communicate with the dentist during this stage instills a sense of security that their fears or queries may be addressed with adequate concern and immediate care. [26] This study has analyzed the efficacy of hand signs in achieving such effective intra-operative communication.
It has been well established that good intra-operative communication that helps patients ventilate their thoughts and worries will enormously reduce their aversion or fear towards the procedure. [27] The lack of a reliable or standard intra-operative communication system can result in misinterpretation, patient discontent, or unpleasant dental experience and vice versa. [16] Intra-operative communication in dental practices is thus a crucial aspect of patient management. The results of this study also indicate that most patients (97.2%) appreciated the importance of hand signs for effective communication with dentists during treatment. Valid questionnaire responses from the participants provided an accurate and representative overview of the significance of the application of hand signs. Vignesh P et al. [16] conducted a questionnaire-based study that recorded the opinion of patients as well as dentists regarding the use of hand signs for intra-operative communication and observed that 86.7% of their respondents agreed on implementing hand signs as a universal protocol to be followed by all the dental practitioners. However, the authors did not design a manual or test its clinical application. Paul Dwyer et al. [28] designed a system of hand signs that included static and dynamic hand signs and proposed guidelines for their usage. However, the efficacy of the hand signs was not analyzed clinically. In contrast to the abovementioned studies, our study involved multiple vital phases, such as designing a new system of hand-sign manuals, training patients for their clinical implementation, and obtaining subsequent feedback. Additionally, this study compared factors such as literacy and gender with the understanding ability of participants, their desire to learn our hand sign manual, and the implementation of hand signs during intra- operative dental procedures. It was observed that literacy did not play a crucial role in realizing the need to communicate with their dentists during intra-operative procedures. The literate and the illiterate considered hand signs critical and displayed equal levels of inclination toward learning the hand signs. Identifying patients with inadequate literacy is crucial. A patient’s ability to read any information brochure provided at health care centers does not always guarantee their comprehension to an acceptable level. [29,30] It has also been observed that evaluating a patient’s understanding of instructions by an attending physician is less than 2% of instances.
[31] However, our study ensured that a proper explanation of the hand sign manual was given to literate and illiterate participants without bias. Interestingly, the results of our study showed that 100% of the illiterate patients felt it was easy to memorize the signs compared to 96.8% of literates who felt the same.
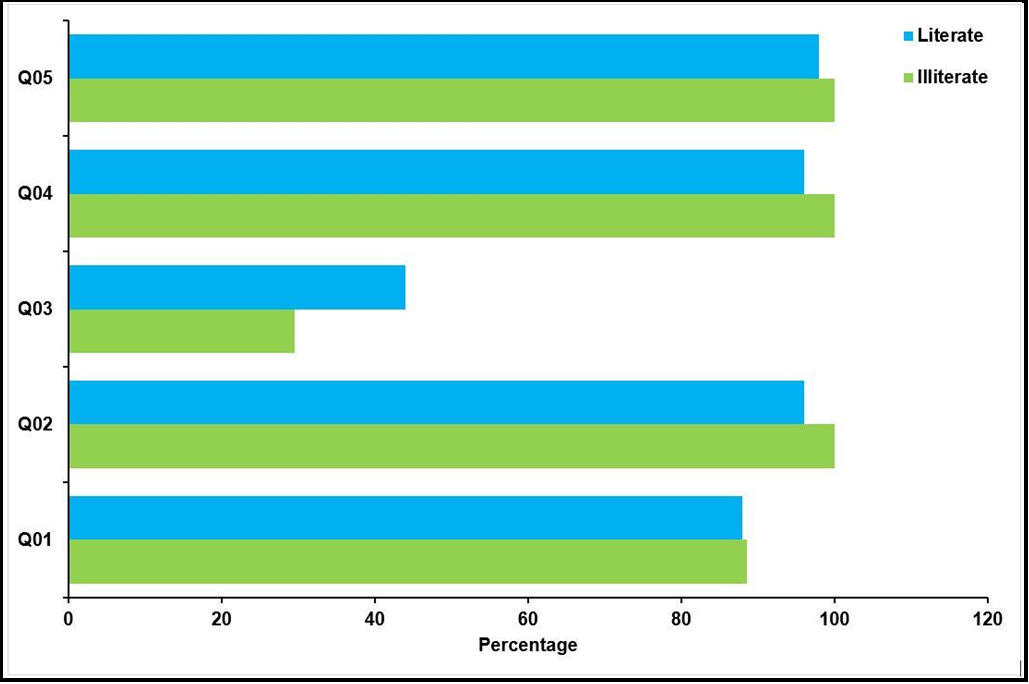
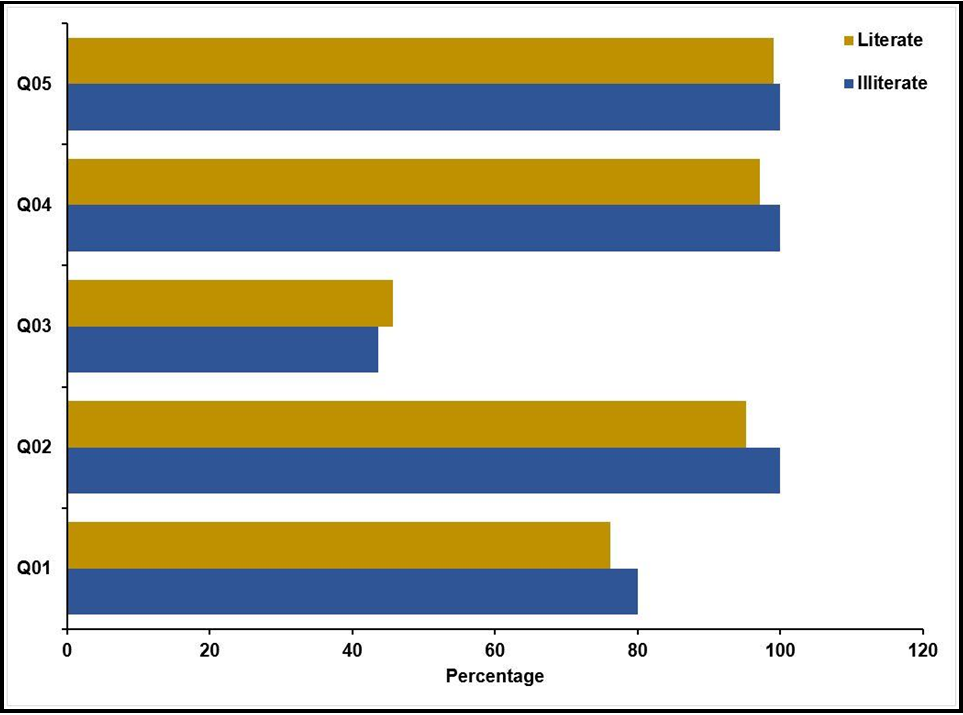
Furthermore, the results of this study are consonant with Goldsmith C et al. [32] regarding the fact that non-verbal communication would help improve multi-lingual patient-dentist communication. No data could be identified in earlier literature comparing gender-based comprehension and opinion on health literacy. However, as evidenced by (Figures 2 and 3), our study found that irrespective of literacy status, both male and female participants acknowledged the efficacy of hand signs equally and the ease of memorization of the same in a positive manner.
Figure 2 Comparing proportions of positive response between illiterate and literate men
Q01: Do you have any experience during which you felt the necessity to communicate to the dentist during the treatment?
Q02: Do you feel it is important to learn hand signals?
Q03: Have you used hand signals during your previous dental treatments?
Q04: Was it easy to memorize these hand signs?
Q05: Do you find these hand signs to be helpful?
Figure 3 Comparing proportions of positive response between illiterate and literate women
Q01: Do you have any experience during which you felt the necessity to communicate to the dentist during the treatment?
Q02: Do you feel it is important to learn hand signals?
A solid and trustworthy dentist-patient relationship established with the help of effective communication plays a crucial role in managing patients’ dental anxiety. [25,33,34] A gap in communication between dentists and patients causes frustration and negative perceptions and reduces patients’ trust in the dentist. [25,33,34] In contrast, a dentist’s empathy towards a patient through good communication has been found to impact patient anxiety and increase patient satisfaction positively. [5] When communication is good, patients comply better with instructions, and the information a relaxed, interested patient provides promotes a greater understanding of any problem. [6] The results of this study also imply that intra-operative communication through this hand sign manual will possibly improve patient satisfaction and reduce anxiety during dental procedures, comparable to the successful outcomes obtained through verbal pre-and postoperative communication mentioned in the literature.[14,25,34,35,36] The authors also propose that emphasis on intra-operative patient-dentist communication needs to be offered as a part of the regular curriculum during dental schooling. [37]
There are many advantages of good communication during dental procedures: (1) effectively reduces the frequency of interruptions during the procedure to convey any information, (2) instills a sense of security in patients and evokes better patient response and cooperation. (3) reduce the duration of treatment by minimizing the frequency of interruptions. We believe that “SRM hand signs” would be helpful in specific clinical scenarios in dentistry where verbalization becomes impossible, such as (1) root canal treatment, fillings/ bridges/crown fixing procedures during which rubber dams are clamped and fixed. (2) After administering local anesthetic injections, which usually affect articulation, (3) in patients before experiencing pre-syncopal episodes or similar conditions.
This study had certain limitations. This study involved feedback from the patients only. Similar feedback from the dentists to analyze their perspective regarding the efficacy of intra-operative communication based on hand signs would help refine the manual. The other limitation is a sample that has yet to be categorized according to various age groups.
Future perspectives
Hand signs for the visually impaired may be devised using Braille and customized for the pediatric population.
Conclusion
Hand signs in dental practice are considered a precious method by patients to establish effective communication between a patient and a dentist. Its practice during dental procedures will benefit both the dentist and the patient, avoiding interrupted talking to reduce fear and anxiety. SRM manual of hand signs is more accessible to learn and adaptable in practice. Besides aiding as a good communication tool, our hand sign manual will always help build a good rapport between the patient and the dentist and increase trust and confidence in the dentist.
Conflict of Interest: None
References
- Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, et al. (2017) Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 18(2): 121-130.
- Lin CS, Wu SY, Yi CA (2017) Association between Anxiety and Pain in Dental Treatment: A Systematic Review and Meta- analysis. J Dent Res. 96(2): 153-162.
- Klingberg G, Broberg AG (2007) Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 17(6): 391-406.
- Armfield JM, Heaton LJ (2013) Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 58(4): 390-407.
- Jones LM, Huggins TJ (2014) Empathy in the dentist-patient relationship: review and application. NZ Dent J. 110(3): 98-104.
- Shigli K, Awinashe V (2010) Patient-dentist communication: an adjunct to successful complete denture treatment. J Prosthodont. 19(6): 491-3.
- Carey JA, Madill A, Manogue M (2010) Communications skills in dental education: a systematic research review. Eur J Dent Educ. 14(2): 69-78.
- Hagihara A, Tarumi K (2006) Doctor and patient perceptions of the level of doctor explanation and quality of patient-doctor communication. Scand J Caring Sci. 20(2): 143-50.
- Mataki S (2000) Patient-dentist relationship. J Med Dent Sci. 47(4): 209-14.
- Hakeberg M, Heidari E, Norinder M, Berggren U (2000) A Swedish version of the Dental Visit Satisfaction Scale. Acta Odontol Scand. 58(1): 19-24.
- Khalifah AM, Celenza A (2019) Teaching and Assessment of Dentist-Patient Communication Skills: A Systematic Review to Identify Best-Evidence Methods. J Dent Educ. 83(1): 16-31.
- Wener ME, Schönwetter DJ, Mazurat N (2011) Developing new dental communication skills assessment tools by including patients and other stakeholders. J Dent Educ. 75(12): 1527-41.
- Becker C, Hunziker S (2019) Die Wichtigkeit der Kommunikation in der Arzt-Patienten-Beziehung [The importance of communication between physicians and patients]. Ther Umsch. 76(5): 231-238.
- Sangappa SB (2012) Patient satisfaction in prosthodontic treatment: multidimensional paradigm. J Indian Prosthodont Soc. 12(1): 21-6.
- Takayama T, Yamazaki Y, Katsumata N (2001) Relationship between outpatients' perceptions of physicians' communication styles and patients' anxiety levels in a Japanese oncology setting. Soc Sci Med. 53(10): 1335-50.
- Vignesh R, Sukanya T, Priyadharshni I (2016) Use of hand signals for communication during dental procedure. Journal of Indian Association of Public Health Dentistry. 14(3): 308-312.
- Sondell K, Palmqvist S, Söderfeldt B (2004) The dentist's communicative role in prosthodontic treatment. Int J Prosthodont. 17(6): 666-71.
- Montgomery KJ, Isenberg N, Haxby JV (2007) Communicative hand gestures and object-directed hand movements activated the mirror neuron system. Soc Cogn Affect Neurosci. 2(2): 114-22.
- Parr LA, Waller BM, Fugate J (2005) Emotional communication in primates: implications for neurobiology. Curr Opin Neurobiol. 15(6): 716-20.
- Goldin-Meadow S, Brentari D (2017) Gesture, sign, and language: The coming of age of sign language and gesture studies. Behav Brain Sci. 40: e46.
- Emmorey K, McCullough S, Mehta S, Ponto LL, Grabowski TJ (2013) The biology of linguistic expression impacts neural correlates for spatial language. J Cogn Neurosci. 25(4): 517-33.
- Jacob MG, Wachs JP, Packer RA (2013) Hand-gesture-based sterile interface for the operating room using contextual cues for the navigation of radiological images. J Am Med Inform Assoc. 20(e1): e183-6
- Gazal G, Tola AW, Fareed WM, Alnazzawi AA, Zafar MS (2016) A randomized control trial comparing the visual and verbal communication methods for reducing fear and anxiety during tooth extraction. Saudi Dent J. 28(2): 80-5.
- Appukuttan DP (2016) Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Investig Dent. 8: 35-50.
- Al-Mobeeriek A (2012) Dentist-patient communication as perceived by patients in Riyadh, Saudi Arabia. Int J Occup Med Environ Health. 25(1): 89-96.
- Vika M, Skaret E, Raadal M, Ost LG, Kvale G (2008) Fear of blood, injury, and injections, and its relationship to dental anxiety and probability of avoiding dental treatment among 18-year-olds in Norway. Int J Paediatr Dent. 18(3): 163-9.
- Freeman R (1999) The psychology of dental patient care. 9. Communicating effectively: some practical suggestions. Br Dent J. 187(5): 240-4.
- Paul R (2008) Interventions to improve communication in autism. Child Adolesc Psychiatr Clin N Am. 17(4): 835-56, ix-x.
- Bass PF 3rd, Wilson JF, Griffith CH, Barnett DR (2002) Residents' ability to identify patients with poor literacy skills. Acad Med. 77(10): 1039-41.
- Davis TC, Fredrickson DD, Arnold C, Murphy PW, Herbst M, et al. (1998) A polio immunization pamphlet with increased appeal and simplified language does not improve comprehension to an acceptable level. Patient Educ Couns. 33(1): 25-37.
- Braddock CH 3rd, Fihn SD, Levinson W, Jonsen AR, Pearlman RA (1997) How doctors and patients discuss routine clinical decisions. Informed decision making in the outpatient setting. J Gen Intern Med. 12(6): 339-45.
- Goldsmith C, Slack-Smith L, Davies G (2005) Dentist-patient communication in the multilingual dental setting. Aust Dent J. 50(4): 235-41.
- Yuan S, Freeman R, Hill K, Newton T, Humphris G (2020) Communication, Trust and Dental Anxiety: A Person-Centred Approach for Dental Attendance Behaviours. Dent J (Basel). 8(4): 118.
- Jaakkola S, Lahti S, Räihä H, Saarinen M, Tolvanen M, et al. (2014) Dental fear affects adolescent perception of interaction with dental staff. Eur J Oral Sci. 122(5): 339-45.
- Wong HM, Bridges SM, McGrath CP, Yiu CK, Zayts OA, et al. (2017) Impact of Prominent Themes in Clinician-Patient Conversations on Caregiver's Perceived Quality of Communication with Paediatric Dental Visits. PLoS One. 12(1): e0169059.
- Berman MH. More on the year one dental visit. Pediatr Dent. 2001;23(4): 342.
- Alvarez S, Schultz JH (2018) A communication-focused curriculum for dental students - an experiential training approach. BMC Med Educ. 18(1): 55.