Motwakil Imam Awadelkareim Imam1*, Mohammed Mahgoup Altayeb Addabalfailla2, Ahmed Awadelkareem Omer Mahmoud2, Ahmed Hassan Abushama Altom2
1Associate Professor of Internal Medicine, Faculty of Medicine, Shendi University, Consultant physician, Elmek Nimer University Hospital. Orcid: 0000-0002-4679-9255
2Medical students, Faculty of Medicine, Shendi University, Sudan
*Corresponding Author: Motwakil Imam Awad Elkareim Imam, Associate Professor of Internal Medicine, Faculty of Medicine, Shendi University, Consultant physician, Elmek Nimer University Hospital. Orcid: 0000-0002-4679-9255
Abstract
Background: COVID-19 viral infection is one of the respiratory infections that make the lives of patients miserable, decreasing the quality of their life and causing a fatal disease, especially in elderly age groups, chronic diseases, co-morbidity patients, and those with immunodeficiency health states. The disease can be diagnosed clinically since symptoms, signs, and examinations are insufficient. A chest X-ray, CT, and imaging techniques must be done for all suspicious cases in all age groups in addition, it is a very infectious disease and spreads fast.
Objectives: To evaluate the effectiveness of radiological procedures in diagnosing COVID-19. Identify various radiological patterns of COVID- 19 and determine the incidence rate of these radiological patterns of COVID-19. Compare the radiological findings between CT and CXR. And to identify which lung involved more and which part involved less.
Methods: This study was conducted from April 2021 to January 2023, taking 21 months to be accomplished. 160 patients participated in this study from centers in the el-Khartoum capital of Sudan and the Nile state.
Results: Both CT and chest X-ray are significant for diagnosing COVID-19. Males are more commonly presented than females. The commonest presenting age in both sexes is between 65 and 85 years. A chest x-ray presents with bilateral lower zonal consolidation in both sexes commonly. The right side lung in chest X-ray is mostly involved in both sexes. CT's chest presented with ground glass opacities in both sexes. There is associated lymph adenopathy and pleural effusion in males, commonly in CT chest. Bilateral lower lung lobes in CT chest are mostly involved in both sexes.
Conclusion: radiological imaging, particularly CT scans, proved to be a critical tool in diagnosing and assessing the severity of COVID19 in Sudanese population. The study also highlighted a strong correlation between extensive radiological finding and severe clinical presentations, emphasizing the prognostic value of imaging in resources-limiting like Sudan.
Keywords: Radiological Patterns, COVID-19, Shendi –Sudan
Introduction:
1.1 Background
Coronaviruses are a family of RNA viruses with spike-like projections. Its surface gives it a crown-like appearance under a microscope [1], found in humans and other mammals such as dogs and cats [2], and can cause illnesses such as the common cold, severe acute respiratory syndrome (SARS), and Middle East respiratory syndrome (MERS). [3]
On January 30, 2020, the coronavirus disease 2019 (COVID-19), formerly known as the 2019 novel coronavirus (2019-nCoV) was declared to be a global health emergency by the World Health Organization. Dramatic measures have been put in place to halt the progression of the virus, and as of February 6, 2020, COVID-19 has infected over 28,000 patients with 564 confirmed deaths. Knowledge of COVID-19 is still evolving, but anecdotal evidence is suggesting that patients can be asymptomatic and infected for up to 14 days. [4] It is clear that our understanding of the radiologic features of COVID- 19 is incomplete, and as it continues to rapidly spread, there is an urgent need to consolidate the emerging knowledge on its radiologic profile. [5]
The signs and symptoms of COVID-19 present at illness onset vary. Still, throughout the disease, many people with COVID-19 will experience fever, cough, shortness of breath, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea, vomiting, or diarrhea [6]. The reported neurological manifestations of COVID-19 include headache, dizziness, confusion, an altered sense of smell (hyposmia/anosmia), and loss of taste (agues) [7]. Fainting and skin manifestations have been less frequently reported [8]. At the end of 2019, the severe acute respiratory syndrome. Coronavirus-2 (SARS-CoV-2) spread from China to different parts of the world, and the ensuing pandemic was officially named coronavirus disease 19 (COVID-19). The disease can be asymptomatic or present with respiratory and/or systemic symptoms. The gold standard diagnostic test for COVID-19 is the real-time reverse transcription polymerase Chain reaction- (RT-PCR) based detection of the viral nucleic acids; however, RT-PCR has low sensitivity [8].
In cases where RT-PCR is not accessible or yields negative results in symptomatic COVID-19 patients, chest imaging is regarded as a component of the screening process for possible COVID-19 cases. For managing COVID-19 patients, laboratory parameters and clinical evaluation are enhanced by radiological imaging. When the first wave of the pandemic peaked in China, computed tomography (CT) was utilized for diagnosis since it is more sensitive (95%) and specific than chest X-rays (CXR) for identifying this illness. According to the Fleischer Society, because a CT scan necessitates laborious decontamination steps to reduce the possibility of cross-infection, it is not appropriate for COVID-19 screening or initial diagnosis. [9] Therefore, CXR cane is used instead of CT because of its extensive availability and easy and quick decontamination procedures. Few studies Have compared the sensitivity of CXR and RT-PCR for Detecting COVID-19; however, the association Between CXR findings and clinical and laboratory findings has not been assessed adequately. [9]
1.2 Problem statement
Carriers of the infection can be asymptomatic, pre-symptomatic, or characteristic. [2] The contagion can enter the body through the air, deposit itself on exposed mucous membranes, and come into contact with infected hands that have defiled hands.[5] 97.5 % of individualities who witness symptoms do so within 11.5 days, with an average exposure to symptom onset of 5 days. [2] In one of the first studies carried out in Wuhan, China, pleural effusion was set up in about 9 of the 62 cases. simply 7 of 919 cases in a sizable systemic review displayed atypical findings similar as parenchymal lung nodes encircled by GGO, lymphadenopathy, pleural effusions, and thickening of the bronchial wall. Since multiple tiny nodules and cavitations are uncommon, bacterial super infection or another opinion should be considered. [10, 11, 12, 13, 14]
1.3 Justification:
Sudan has not seen enough exploration on the content, and in our clinical practice, we've observed that cases with COVID-19 who tested positive for the contagion had a range of radiological instantiations. We thus decided to carry out this exploration to gain a better understanding of the issue and enhance our practice going forward.
1.4 Objectives:
1.4.1 General objectives: To identifying various radiological patterns of covid-19 among adult Sudanese patients
1.4.2 Specific objective: To evaluate the effectiveness of radiological procedures’ in the diagnosis of COVID-19, to identify various radiological patterns of COVID-19, to determine the incidence rate of this radiological patterns of COVID-19, to compare the radiological finding between CT and CXR, and to identify which lung involved more and which part involved less.
1.5 Previous study:
According to Thomas C. Kwee and Robert M. Kwee there were Several chest CT findings have been reported in more than 70% of RT-PCR test–proven COVID-19 cases, include ground-glass opacities, vascular enlargement, bilateral abnormalities and lower lobe involvement. Other findings have been reported in10%–70% of RT-PCR test–proven COVID-19cases include consolidation (51.5%), air bronchogram (40.2%), pleural thickening (34.7%), nodules (19.8%) and bronchial wall thickening (14.3%). The following lesion distributions have been reported unilateral (15.0%), multifocal (63.2%), diffuse (26.4%), single and/or focal (10.5%), middle or upper lobe involvement (49.3%–55.4%), peripheral location (59.0%), and central and peripheral location (36.2%). Finally, the uncommon findings in RT-PCR test–proven COVID-19 cases include pleural effusion (5.2%), lymphadenopathy (5.1%) and cavitation lung lesions (0.7%). [15]
A study conducted in Hong Kong involved 21 COVID-19 cases found predominant imaging pattern was of ground-glass opacification with occasional consolidation in the peripheries. Pleural effusions and lymphadenopathy were absent in all those cases. [16]
A study conducted in Turkey about chest X-ray and chest CT findings of pediatric patients with COVID-19 stated the findings are most commonly observed unilaterally and in lower zones of lungs in chest X-ray examinations. Bilateral and multifocal involvement (55%) was the most observed involvement in the CT examinations, as well as single lesion and single lobe (27%) involvement were also detected. In 41% of cases ground-glass appearance was observed, ground-glass appearance and consolidation together were in 36%. While peripheral and central co-distribution of the lesions (55%) was frequently observed, the involvement of the lower lobes (69%) was significant [17].
A study conducted in Italy found that the CXR showed most prevalent manifestations in CXR in COVID-19 patients are consolidations (46.9%) and hazy increased opacities (37.5%). Typical CT features included bilateral and multilobar ground-glass opacities with (59.5%) and without (35.7%) consolidations having a predominantly peripheral distribution (64.3%). Also, lymphadenopathy (14.3 %) and pleural effusion (7.1%) were observed [18].
2. Methodology:
2.1 Study design: a sanitarium- grounded, descriptive, retrospective study. Between April and October of 2022, 110 CT and 50 CXR samples were attained from multi-institutional Sudanese isolation centers. A fresh educated radiologist reviewed the radiological instantiations.
2.2 Study area: This study was conducted in multi-institutional isolation centers in Sudan, which treat cases with COVID- 19 and accept cases from different municipalities in Sudan. The Jabra isolation center is located in Khartoum, the capital of Sudan; the Shendi and Atbara isolation centers are located in the state of the River Nile.
2.3 Study population COVID-19 PCR-positive cases that were brought to multi-institutional Sudanese isolation centers passed radiological images.
2.4 Study Sample. 4.1 Sample type convenience slice system.
2.5 Sample size: 160 radiological images, including 110 CT and 50 CXR.
2.5.1 Data collection:
2.5.2 Data collection tools: Data collected via standardized pre- designed questionnaires.
2.5.3 Data collection ways: data attained from multi-institutional Sudanese isolation centers.
2.5.4 Variables Socio- demographic variables
2.5.5 Data analysis: A software program was used to enter the data from an Excel distance recording into the computer. The statistical package for social wisdom (SPSS) was also used to dissect the data and produce results that were displayed as numbers, tables, and graphs.
3. Ethical concurrence: The operation of the study area and the original ethical commission granted formal blessing. All collected data will be kept private and non-public.
4. Results:
4.1 Regarding to the finding CT:
Twenty-eight patients had multifocal in peripheral and basal area 25.4% ,thirteen patients had diffuse 11.8%, thirty-six patients had bilateral peripheral 32.7%, nine patients had sub pleural 8.2%, three patients had right upper lobar 2.7%, three patients had left upper lobar 2.7%, three patients had bilateral lower 2.7%, only one patient had posterior upper lobar bilateral 0.9% ,one patient had right middle lobar 0.9%, thirty eight patients had consolidation 34.5%, thirteen patients had pleural effusion 11.8%, one patient had pericardial effusion 0.9%, three patients had pulmonary hyperinflation 2.7%, one patient had pneumothorax 0.9%, one patient had pulmonary edema 0.9%, one patient had pulmonary nodule 0.9%, three patients had abdominal ascites 2.7%, nine patients had honey combs appearance 8.2, two patients had bilateral mosaic attenuation 1.8%, thirty three patients had mediastinal lymphadenopathy 30%, seventeen patients had Para tracheal lymphadenopathy 15.7%, one patient had mediastinal and lower cervical lymphadenopathy 0.9%, six patients had upper labara spider web septal thickening 5.4%, two patients had bilateral sub pleural spider web septal thickening 1.8%, two patients right apical 1.8%, two patients right lower 1.8%, only one patient had lingular 0.9%
Only one patient had bilateral middle and lower consolidation 0.8%, one patient had right upper consolidation 0.8%, one patient had left upper and lower consolidation 0.8%, one patient had left lower consolidation 0.8%, one patient had right middle and lower consolidation 0.8%, and sixteen patients had bilateral lower consolidation 16.9%, six patients had bilateral diffuse consolidation 4.8%, and two patients had bilateral upper consolidation 1.6%. [Table 1]
Table 1: Distribution of the study group according to Finding CT:
|
Item |
Frequency |
Percentage |
|
multifocal in peripheral &Basal area GGO |
28 |
25.4% |
|
Diffuse GGO |
13 |
11.8% |
|
Bilateral peripheral GGO |
36 |
32.7% |
|
Sub pleural GGO |
9 |
8.2% |
|
Right Upper lobar GGO |
3 |
2.7% |
|
Left Upper lobar GGO |
3 |
2.7% |
|
Bilateral lower GGO |
3 |
2.7% |
|
posterior upper lobar Bilaterally GGO |
1 |
0.9% |
|
Right Middle lobar GGO |
1 |
0.9% |
|
Consolidation |
38 |
34.5% |
|
Pleural Effusion |
13 |
11.8% |
|
Pericardial Effusion |
1 |
0.9% |
|
Pulmonary Hyper inflation |
3 |
2.7% |
|
Pneumothorax |
1 |
0.9% |
|
Pulmonary Edema |
1 |
0.9% |
|
Pulmonary Nodule |
1 |
0.9% |
|
Abdominal Ascites |
3 |
2.7% |
|
Honey combos’ appearance |
9 |
8.2% |
|
Bilateral Mosaic attenuation |
2 |
1.8% |
|
Mediastinal lymph adenopathy |
33 |
30% |
|
Para tracheal lymph adenopathy |
17 |
15.4% |
|
Mediastina & lower Cervical lymph |
1 |
0.9% |
|
Upper labara spider web septal thickening |
6 |
5.4% |
|
Bilateral sub pleural spider web septal thickening |
2 |
1.8% |
|
Right apical |
2 |
1.8% |
|
Right lower |
2 |
1.8% |
|
Lingular |
1 |
0.9% |
|
Total |
110 |
100.0% |
4.2 Regarding to the finding of the X-ray:
Forty four patients had bilateral lower consolidation 28%, three patients had bilateral middle and lower consolidation 6%, three patients had bilateral middle consolidation 6%, four patients had bilateral upper and lower consolidation 8%, two patients had bilateral diffuse consolidation 4%, two patients had bilateral middle and lower consolidation and cavitations 4%, five patients had right lower consolidation 10%, four patients had right middle and lower consolidation 8%, only one patient had right upper consolidation 2%, two patients had right diffuse consolidation 4%, one patient had right upper and lower consolidation 2%, one patient had right lower consolidation and cavitations 2%, one patient had right diffuse consolidation and cavitations and loss of lung volume 2%, two patients had left middle and lower consolidation 4%, one patient had right upper and middle and left lower cavitations 2%, one patient had right diffuse and left upper consolidation 2%, one patient had right diffuse and left middle consolidation 2%, one patient had right diffuse and left lower consolidation 2%. [Table 2]
Table No 2: Distribution of the study group according to the Finding X-ray
|
Item |
Frequency |
percentage |
|
Bilateral lower consolidation |
14 |
28.0% |
|
Bilateral Middle & lower consolidation |
3 |
6.0% |
|
Bilateral Middle consolidation |
3 |
6.0% |
|
Bilateral Upper& lower consolidation |
4 |
8.0% |
|
Bilateral Diffuse consolidation |
2 |
4.0% |
|
Bilateral Middle & lower consolidation & cavitations |
2 |
4.0% |
|
Right lower consolidation |
5 |
10.0% |
|
Right middle& lower consolidation |
4 |
8.0% |
|
Right Upper consolidation |
1 |
2.0% |
|
Right Diffuse consolidation |
2 |
4.0% |
|
Right Upper& lower consolidation |
1 |
2.0% |
|
Right lower consolidation & cavitations |
1 |
2.0% |
|
Right Diffuse consolidation & cavitations &loss of lung Volume |
1 |
2.0% |
|
left middle &lower consolidation |
2 |
4.0% |
|
Right Upper & middle + left lower cavitations |
1 |
2.0% |
|
Right Diffuse &left Upper consolidation |
1 |
2.0% |
|
Right Diffuse &left middle consolidation |
1 |
2.0% |
|
Right Diffuse &left lower consolidation |
2 |
4.0% |
|
Total |
50 |
100.0% |
4.3 Regarding the relation between finding CT and age patient CT:
Less than 25 years of total of five patients 5.6%; three patients had multifocal in peripheral basal area 3.4%, only one patient had to diffuse 1.1%, two patients had bilateral peripheral 2.2%, one patient had right upper lobar 1.1%, one patient had bilateral lower 1.1%, one patient had bilateral diffuse consolidation 1.1%, No patient had sub pleural, left upper lobar, posterior upper lobar bilateral, bilateral lower consolidation, bilateral upper consolidation, bilateral middle, and lower consolidation, right upper consolidation, left upper consolidation, left upper and lower consolidation, left lower consolidation, right middle, and lower consolidation, right lower consolidation 0.0%.
25 – 45 years total of eighteen patients 20.2%; two patients had multifocal in peripheral basal area 2.2%, six patients had to diffuse 6.7%, seven patients had bilateral peripheral 7.9%, one patient had left upper lobar 1.1%, two patients had bilateral diffuse consolidation 2.2%, one patient had posterior upper lobar bilateral1.1%, five patients had bilateral lower consolidation 5.6%, No patient had subpleural, right upper lobar, bilateral lower, bilateral upper consolidation, bilateral middle and lower consolidation, right upper consolidation, left upper consolidation, left upper and lower consolidation, left lower consolidation, right middle, and lower consolidation, right lower consolidation 0.0%.
46-65 years total thirty-one patients 34.8%; ten patients had multifocal in a peripheral basal area 11.2%, one patient had to diffuse 1.1%, fifteen patient had bilateral peripheral 16.9%, one patient had subpleural 1.1%, one patient had right upper lobar 1.1%, one patient had left upper lobar 1.1%, five patients had bilateral lower consolidation 5.6%, 2 patients had bilateral diffuse consolidation 2.2%, two patients had bilateral upper consolidation 2.2%, one patient had right upper consolidation 1.1%, one patient had left lower consolidation 1.1%, one patient had right lower consolidation 1.1%, No patient had bilateral lower consolidation, posterior upper lobar bilateral, bilateral middle and lower consolidation, left upper and lower consolidation, right middle and lower consolidation 0.0%. 66-85 years total twenty-nine patients 32.6%; fifteen patients had multifocal in a peripheral basal area 11.2%, three patients diffuse 3.4%, eleven patients had bilateral peripheral 12.4%, one patient had subpleural 1.1%, one patient had right upper lobar 1.1%, one patient had left upper lobar 1.1%, eleven patients had bilateral lower consolidation 12.4%, one patient had bilateral middle and lower consolidation 1.1%, one patient had left upper and lower consolidation 1.1%, one patient had right middle and lower consolidation 1.1%, No patient had bilateral lower, posterior upper lobar bilateral, bilateral diffuse consolidation, bilateral upper consolidation, right upper consolidation, left lower consolidation, right lower consolidation 0.0%.
More than 85 years total of six patients 6.7%; three patients had multifocal in peripheral basal area 3.4%, two patients had to diffuse 2.2%, one patient had bilateral peripheral 1.1%, one patient had subpleural 1.1%, one patient had bilateral diffuse consolidation 1.1%, No patient had right upper lobar, left upper lobar, bilateral lower, posterior upper lobar bilateral, bilateral lower consolidation, bilateral upper consolidation, bilateral middle, and lower consolidation, right upper consolidation, left upper and lower consolidation, left lower consolidation, right middle, and lower consolidation, right lower 0.0%. [Table 3]
Table 3: Relation between the study groups age and CT findings (P.V=.044)
|
Finding CT |
Age |
Total |
||||
|
less than 25 years |
25 – 45 years |
46 – 65 years |
66 – 85 years |
> 85 years |
||
|
multifocal in peripheral Basal area |
3 |
2 |
10 |
15 |
3 |
33 |
|
3.4% |
2.2% |
11.2% |
11.2% |
3.4% |
32.5% |
|
|
Diffuse |
1 |
6 |
1 |
3 |
2 |
13 |
|
1.1% |
6.7% |
1.1% |
3.4% |
2.2% |
14.6% |
|
|
Bilateral peripheral |
2 |
7 |
15 |
11 |
1 |
40 |
|
2.2% |
7.9% |
16.9% |
12.4% |
1.1% |
41.4% |
|
|
Sub pleural |
0 |
0 |
1 |
1 |
1 |
3 |
|
0.0% |
0.0% |
1.1% |
1.1% |
1.1% |
3.4% |
|
|
Right Upper lobar |
1 |
0 |
1 |
1 |
0 |
3 |
|
1.1% |
0.0% |
1.1% |
1.1% |
0.0% |
3.4% |
|
|
Left Upper lobar |
0 |
1 |
1 |
1 |
0 |
3 |
|
0.0% |
1.1% |
1.1% |
1.1% |
0.0% |
3.4% |
|
|
Bilateral lower |
1 |
0 |
0 |
0 |
0 |
1 |
|
1.1% |
0.0% |
0.0% |
0.0% |
0.0% |
1.1% |
|
|
posterior upper lobar Bilateral |
0 |
1 |
0 |
0 |
0 |
1 |
|
0.0% |
1.1% |
0.0% |
0.0% |
0.0% |
1.1% |
|
|
Bilateral lower Consolidation |
0 |
5 |
5 |
11 |
0 |
21 |
|
0.0% |
5.6% |
5.6% |
12.4% |
0.0% |
23.6% |
|
|
Bilateral diffuse Consolidation |
1 |
2 |
2 |
0 |
1 |
6 |
|
1.1% |
2.2% |
2.2% |
0.0% |
1.1% |
6.7% |
|
|
Bilateral Upper Consolidation |
0 |
0 |
2 |
0 |
0 |
2 |
|
0.0% |
0.0% |
2.2% |
0.0% |
0.0% |
2.2% |
|
|
Bilateral middle and lower Consolidation |
0 |
0 |
0 |
1 |
0 |
1 |
|
0.0% |
0.0% |
0.0% |
1.1% |
0.0% |
1.1% |
|
|
Right Upper Consolidation |
0 |
0 |
1 |
0 |
0 |
1 |
|
0.0% |
0.0% |
1.1% |
0.0% |
0.0% |
1.1% |
|
|
lift Upper and lower Consolidation |
0 |
0 |
0 |
1 |
0 |
1 |
|
0.0% |
0.0% |
0.0% |
1.1% |
0.0% |
1.1% |
|
|
lift lower Consolidation |
0 |
0 |
1 |
0 |
0 |
1 |
|
0.0% |
0.0% |
1.1% |
0.0% |
0.0% |
1.1% |
|
|
Right middle and lower Consolidation |
0 |
0 |
0 |
1 |
0 |
1 |
|
0.0% |
0.0% |
0.0% |
1.1% |
0.0% |
1.1% |
|
|
Right lower |
0 |
0 |
1 |
0 |
0 |
1 |
|
0.0% |
0.0% |
1.1% |
0.0% |
0.0% |
1.1% |
|
|
Total |
5 |
18 |
31 |
29 |
6 |
110 |
|
5.6% |
20.2% |
34.8% |
32.6% |
6.7% |
100.0% |
|
4.4 Regarding the relation between finding X-ray and the age of the patient X-ray:
25–45 years total nine patients 18%; two patients had bilateral lower zonal consolidation 4%, only one patient had bilateral middle and lower consolidation 2%, one patient had bilateral middle consolidation 2%, one patient had bilateral diffuse consolidation 2%, one patient had middle and lower consolidation and cavitations 2%, one patient had right lower consolidation 2%, one patient had right upper consolidation 2%, and one patient had right diffuse and left middle consolidation 2%. No patient had bilateral upper and lower consolidation, right middle lower consolidation, right diffuse consolidation, right upper lower consolidation, right lower consolidation and cavitations, left middle and lower consolidation, right upper and middle and left lower cavitations, right diffuse and left upper consolidation, or right diffuse and left lower consolidation 0.0%.
46 – 65 years total fifteen patient 30%; three patients had bilateral lower zonal consolidation 6%, two patients had bilateral middle consolidation 4%, one patient had middle and lower consolidation and cavitations 2%, one patient had right lower consolidation 2%, three patients had right middle lower consolidation 6%, one patient had right diffuse consolidation 2%, one patient had right lower consolidation and cavitations 2%, one patient had left middle and lower consolidation 2%, one patient had right diffuse and left upper consolidation 2%, No patient had bilateral middle and lower consolidation, bilateral upper and lower consolidation, bilateral diffuse consolidation, right upper consolidation, right upper lower consolidation, right upper and middle and left lower cavitations, right diffuse and left middle consolidation, right diffuse and left lower consolidation 0.0%.
66 – 85 years total of twenty patients 40%; eight patients had bilateral lower zonal consolidation 16%, four patients had bilateral upper and lower consolidation 8%, one patient had bilateral diffuse consolidation 2%, three patients had right lower consolidation 6%, one patient had right middle lower consolidation 2%, one patient had right diffuse consolidation 2%, one patient had upper and middle and left lower cavitations 2%, one patient had right diffuse and left lower consolidation 2%, No patient had bilateral middle consolidation, bilateral middle and lower consolidation and cavitations, right upper consolidation, right upper lower consolidation, right lower consolidation, and cavitations, left middle and lower consolidation, right diffuse and left upper consolidation, right diffuse and left middle consolidation 0.0%.
More than 85 years total of six patients 12%; only one patient had bilateral lower zonal consolidation 2%, two patients had bilateral middle and lower consolidation 4%, one patient had right upper lower consolidation 2%, one patient had left middle and lower consolidation 2%, one patient had right diffuse and left lower consolidation 2%, No patient had bilateral middle consolidation, bilateral upper and lower consolidation, bilateral diffuse consolidation, bilateral middle, and lower consolidation and cavitations, right lower consolidation, right middle lower consolidation, right upper consolidation, right diffuse consolidation, right lower consolidation, and cavitations, right upper and middle and left lower cavitations, right diffuse and left upper consolidation, right diffuse and left middle consolidation 0.0%. [Table 4]
Table 4: Relation between study group age and CXR Findings (P.V=.027)
|
Finding X- ray |
Age X-ray |
Total |
|||
|
25 – 45 years |
46 – 65 years |
66 - 85 years |
> 85 years |
||
|
Bilateral lower zonal consolidation |
2 |
3 |
8 |
1 |
14 |
|
4.0% |
6.0% |
16.0% |
2.0% |
28.0% |
|
|
Bilateral Middle & lower consolidation |
1 |
0 |
0 |
2 |
3 |
|
2.0% |
0.0% |
0.0% |
4.0% |
6.0% |
|
|
Bilateral Middle consolidation |
1 |
2 |
0 |
0 |
3 |
|
2.0% |
4.0% |
0.0% |
0.0% |
6.0% |
|
|
Bilateral Upper& lower consolidation |
0 |
0 |
4 |
0 |
4 |
|
0.0% |
0.0% |
8.0% |
0.0% |
8.0% |
|
|
Bilateral Diffuse consolidation |
1 |
0 |
1 |
0 |
2 |
|
2.0% |
0.0% |
2.0% |
0.0% |
4.0% |
|
|
Bilateral Middle & lower consolidation + cavitations |
1 |
1 |
0 |
0 |
2 |
|
2.0% |
2.0% |
0.0% |
0.0% |
4.0% |
|
|
Right lower consolidation |
1 |
1 |
3 |
0 |
5 |
|
2.0% |
2.0% |
6.0% |
0.0% |
10.0% |
|
|
Right middle lower consolidation |
0 |
3 |
1 |
0 |
4 |
|
0.0% |
6.0% |
2.0% |
0.0% |
8.0% |
|
|
Right Upper consolidation |
1 |
0 |
0 |
0 |
1 |
|
2.0% |
0.0% |
0.0% |
0.0% |
2.0% |
|
|
Right Diffuse consolidation |
0 |
1 |
1 |
0 |
2 |
|
0.0% |
2.0% |
2.0% |
0.0% |
4.0% |
|
|
Right Upper lower consolidation |
0 |
0 |
0 |
1 |
1 |
|
0.0% |
0.0% |
0.0% |
2.0% |
2.0% |
|
|
Right lower consolidation + cavitations |
0 |
1 |
0 |
0 |
1 |
|
0.0% |
2.0% |
0.0% |
0.0% |
2.0% |
|
|
left middle& lower consolidation |
0 |
1 |
0 |
1 |
2 |
|
0.0% |
2.0% |
0.0% |
2.0% |
4.0% |
|
|
Right Upper & middle + left lower cavitations |
0 |
0 |
1 |
0 |
1 |
|
0.0% |
0.0% |
2.0% |
0.0% |
2.0% |
|
|
Right Diffuse +left Upper consolidation |
0 |
1 |
0 |
0 |
1 |
|
0.0% |
2.0% |
0.0% |
0.0% |
2.0% |
|
|
Right Diffuse +left middle consolidation |
1 |
0 |
0 |
0 |
1 |
|
2.0% |
0.0% |
0.0% |
0.0% |
2.0% |
|
|
Right Diffuse +left lower consolidation |
0 |
0 |
1 |
1 |
2 |
|
0.0% |
0.0% |
2.0% |
2.0% |
4.0% |
|
|
Total |
9 |
15 |
20 |
6 |
50 |
|
18.0% |
30.0% |
40.0% |
12.0% |
100.0% |
|
4.5 Regarding the relationship between patient gender and finding CT:
Male total sixty-three patients ; nineteen patients had multifocal in peripheral basal area 30.1%, ten patients had diffuse 15.8%, nine patients had bilateral peripheral 14.2%, nine patients had sub pleural 14.2%, three patients had right upper lobar 4.7%, three patients had left upper lobar 4.7%, three patients had bilateral lower 4.7%, one patient had posterior upper lobar bilateral 1.5%, one patient had right middle 1.5%, sixteen patients had consolidation 25.3%, eight patients had pleural effusion 12.6%, no patient had pericardial effusion 0.0%, three patients had pulmonary hyperinflation 4.7%, one patient had pneumothorax 0.5%, one patient had pulmonary edema 0.5%, no patient had pulmonary nodule 0.0% , two patients had abdominal ascites 3.2%, nine patients had honey combs appearance 14.2%, one patient had bilateral mosaic attenuation 1.5%, twenty-two patients had meditational lymphadenopathy 34.9%, twelve patients had Para tracheal lymphadenopathy 19%, one patient had mediastina and lower cervical lymphadenopathy 0.5%, 5patients had upper labara spider web septal thickening 7.9%, one patient had bilateral sub pleural spider web septal thickening 1.5%, no patient right apical , right lower , lingular 0.0%.
Female total forty-seven; nine patients had multifocal in peripheral basal area GGO 19.1%, three patients had diffuse GGO 6.3%, twenty- seven patients had bilateral peripheral GGO 57.4%, no patient subpleural, right upper lobar, left upper lobar, bilateral lower, posterior upper lobar bilateral, bilateral lower, bilateral middle and lower, right upper, left upper and lower, left lower, right middle and lower, right lower. [Table 5]
Table 5: Relation between the study groups between Finding CT and Gender Patient CT
|
Finding CT |
Gender |
P.V |
||
|
Male |
Female |
|||
|
multifocal in peripheral &Basal area |
N |
19 |
9 |
.011 |
|
% |
30.1% |
19.1% |
||
|
Diffuse |
N |
10 |
3 |
|
|
% |
15.8% |
6.3% |
||
|
Bilateral peripheral |
N |
9 |
27 |
|
|
% |
14.2% |
57.4% |
||
|
Sub pleural |
N |
9 |
0 |
|
|
% |
14.2% |
0.0% |
||
|
Right Upper lobar |
N |
3 |
0 |
|
|
% |
4.7% |
0.0% |
||
|
Left Upper lobar |
N |
3 |
0 |
|
|
% |
4.7% |
0.0% |
||
|
Bilateral lower |
N |
3 |
0 |
|
|
% |
4.7% |
0.0% |
||
|
posterior upper lobar Bilaterally |
N |
1 |
0 |
|
|
% |
1.5% |
0.0% |
||
|
Right Middle lobar |
N |
1 |
0 |
|
|
% |
1.5% |
0.0% |
||
|
Consolidation |
N |
16 |
22 |
|
|
% |
25.3% |
46.8% |
||
|
Pleural Effusion |
N |
8 |
5 |
|
|
% |
12.6% |
10.6% |
||
|
Pericardial Effusion |
N |
0 |
1 |
|
|
% |
0.0% |
2.1% |
||
|
Pulmonary Hyper inflation |
N |
3 |
0 |
|
|
% |
4.7% |
0.0% |
||
|
Pneumothorax |
N |
1 |
0 |
|
|
% |
1.5% |
0.0% |
||
|
Pulmonary Edema |
N |
1 |
0 |
|
|
% |
1.5% |
0.0% |
||
|
Pulmonary Nodule |
N |
0 |
1 |
|
|
% |
0.0% |
2.1% |
||
|
Abdominal Ascites |
N |
2 |
1 |
|
|
% |
3.2% |
2.1% |
||
|
Honey combos’ appearance |
N |
9 |
0 |
|
|
% |
14.2% |
0.0% |
||
|
Bilateral Mosaic attenuation |
N |
1 |
1 |
|
|
% |
1.5% |
2.1% |
||
|
Mediastinal lymph adenopathy |
N |
22 |
11 |
|
|
% |
34.9% |
4.7% |
||
|
Para tracheal lymph adenopathy |
N |
12 |
5 |
|
|
% |
19% |
10.6% |
||
|
Mediastina & lower Cervical lymph |
N |
1 |
0 |
|
|
% |
1.5% |
0.0% |
||
|
Upper labara spider web septal thickening |
N |
5 |
1 |
|
|
% |
7.9% |
2.1% |
||
|
Bilateral sub pleural spider web septal thickening |
N |
1 |
1 |
|
|
% |
1.5% |
2.1% |
||
|
Right apical |
N |
0 |
2 |
|
|
% |
0.0% |
4.2% |
||
|
Right lower |
N |
0 |
2 |
|
|
% |
0.0% |
4.2% |
||
|
Lingular |
N |
0 |
1 |
|
|
% |
0.0% |
2.1% |
||
|
Total |
N |
63 |
47 |
|
|
% |
100% |
100% |
||
4.6 Regarding the relation between finding X-ray and gender patient X-ray:
Male total thirty nine patients 78%, eleven patients had bilateral lower zonal consolidation 22%, three patients had bilateral middle and lower consolidation 6%, two patients had bilateral middle consolidation 4%, only one patient had bilateral upper and lower consolidation 2%, one patient had bilateral diffuse consolidation 2%, one patient had bilateral middle and lower consolidation and cavitations 2%, five patients had right lower consolidation 10%, three patients had right middle lower consolidation 6%, one patient had upper consolidation 2%, one patient had right diffuse consolidation 2% ,one patient had right upper lower consolidation 2%, one patient had right lower consolidation and cavitations 2%, one patient had left middle and lower consolidation %, two patients had right upper and middle and left lower cavitations 4%, one patient had right diffuse and left upper consolidation 2%, one patient had right and left middle consolidation 2%, one patient had right diffuse and left lower consolidation 2%.
One patient had bilateral diffuse consolidation 6%, one patient had bilateral middle and lower consolidation and cavitations 2%, one patient had right lower consolidation, one patient had right middle lower consolidation 2%, and three patients had bilateral lower zonal consolidation 6%, 2%, and 6%, respectively. Of the eleven patients, twenty-two percent were female. There was not a single patient with the following conditions: one left middle and lower consolidation, one right diffuse and left upper consolidation, one right and left middle consolidation, one right diffuse and left lower consolidation and cavitations, and one right diffuse and lower consolidation and cavitations. [Table 6]
Table 6: Relation between the study groups between Finding X- ray and Gender Patient X- ray (P.V=.081)
|
Finding X-ray |
Gender |
Total |
|
|
Male |
Female |
||
|
Bilateral lower zonal consolidation |
11 |
3 |
14 |
|
22.0% |
6.0% |
28.0% |
|
|
Bilateral Middle & lower consolidation |
3 |
0 |
3 |
|
6.0% |
0.0% |
6.0% |
|
|
Bilateral Middle consolidation |
2 |
1 |
3 |
|
4.0% |
2.0% |
6.0% |
|
|
Bilateral Upper& lower consolidation |
1 |
3 |
4 |
|
2.0% |
6.0% |
8.0% |
|
|
Bilateral Diffuse consolidation |
1 |
1 |
2 |
|
2.0% |
2.0% |
4.0% |
|
|
Bilateral Middle & lower consolidation + cavitations |
1 |
1 |
2 |
|
2.0% |
2.0% |
4.0% |
|
|
Right lower consolidation |
5 |
0 |
5 |
|
10.0% |
0.0% |
10.0% |
|
|
Right middle lower consolidation |
3 |
1 |
4 |
|
6.0% |
2.0% |
8.0% |
|
|
Right Upper consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Right Diffuse consolidation |
1 |
1 |
2 |
|
2.0% |
2.0% |
4.0% |
|
|
Right Upper lower consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Right lower consolidation + cavitations |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
left middle & lower consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Right Upper & middle + left lower cavitations |
2 |
0 |
2 |
|
4.0% |
0.0% |
4.0% |
|
|
Right Diffuse +left Upper consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Right Diffuse +left middle consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Right Diffuse +left lower consolidation |
1 |
0 |
1 |
|
2.0% |
0.0% |
2.0% |
|
|
Total |
39 |
11 |
50 |
|
78.0% |
22.0% |
100.0% |
|
4.7 Regarding the relation between the X-ray findings according to lung and lope involved:
Our result was that all of them have consolidation 55% with bilateral lung involved, 35.4% with right lung involved, and 9.6% with left lung involved as follows:
Consolidation on both sides of the lower lobe affected 17.7% of males and 4.8% of females, only on the right side in 11.2% of males and 0% of females, and in 4.8% of males and 0% of females. They were also involved with cavitations at the right lung in 1.6% of males. The middle lobe involved consolidation bilaterally in 3.2% of males & 1.6% of females, the right side only in 0% of males and 0% of females, and the left side in 1.6% of males and 0% of females. The upper lobe involved consolidation bilaterally in 0% of males & 0% of females, the right side only in 1.6% of males and 0% of females, and the left side in 1.6% of males and 0% of females.
6.4% of males and 4.8% of females had bilateral involvement of the middle and lower lobes in consolidation, whereas 1.6% of males and 0% of females had bilateral involvement on the left side and 4.8% of males on the right side. 6.4% of males and 4.8% of females had bilateral involvement of the middle and lower lobes in consolidation, whereas 1.6% of males and 0% of females had bilateral involvement on the left side and 4.8% of males on the right side. 6.4% of males and 4.8% of females had bilateral involvement of the middle and lower lobes in consolidation, whereas 1.6% of males and 0% of females had bilateral involvement on the left side and 4.8% of males on the right side. 6.4% of males and 4.8% of females had bilateral involvement of the middle and lower lobes in consolidation, whereas 1.6% of males and 0% of females had bilateral involvement on the left side and 4.8% of males on the right side. 6.4% of men and 4.8% of women had bilateral involvement of the middle and lower lobes in consolidation; only 4.8% of men and 1.6% of women had bilateral involvement of the right side, and 1.6% of men and 0% of women had bilateral involvement of the left side. Only 4.8% of men and 1.6% of women had bilateral involvement of the right side, and 1.6% of men and 0% of women had bilateral involvement of the left side. In consolidation, 6.4% of men and 4.8% of women had bilateral involvement of the middle and lower lobes. 6.4% of men and 4.8% of women had bilateral involvement of the middle and lower lobes in consolidation; only 4.8% of men and 1.6% of women had bilateral involvement of the right side, and 1.6% of men and 0% of women had bilateral involvement of the left side. They were also involved with cavitations bilaterally in 1.6% of males & 1.6% of females. Both upper & lower lobes were involved with consolidation bilaterally in 3.2% of males & 0% of females, the right side only in 0% of males and 0% of females, left side in 0% of males and 0% of females. Both upper & middle lobes involved consolidation bilaterally in 1.6% of males & 0% of females, the right side only in 0% of males and 0% of females, left side in 0% of males and 0% of females. Diffuse lung involved consolidation bilaterally in 3.2% of males & 1.6% of females, right side only in 9.6% of males and 1.6% of females, left side 0% of males and 0% of females. And with cavitations bilaterally in 1.6% of males & 1.6% of females, right lung in 1.6% of males & 1.6% of females. [Table 7]
Table 7: Relation between the study groups between X-ray finding according to lung & lobe involved (P.V=.181)
|
Finding |
Gender |
Bilateral |
Right |
Left |
Total |
|
lower lobe consolidation |
Male |
11(17.7%) |
7(11.2%) |
3(4.8%) |
21(33.8%) |
|
Female |
3(4.8%) |
0(0.0%) |
0(0.0%) |
3(4.8%) |
|
|
middle& lower consolidation |
Male |
4(6.4%) |
3(4.8%) |
1(1.6%) |
8(12.6%) |
|
Female |
3(4.8%) |
1(1.6%) |
0(0.0%) |
4(6.4%) |
|
|
middle lobe consolidation |
Male |
2(3.2%) |
0(0.0%) |
1(1.6%) |
3(4.8%) |
|
Female |
1(1.6%) |
0(0.0%) |
0(0.0%) |
1(1.6%) |
|
|
upper &lower lobe consolidation |
Male |
2(3.2%) |
0(0.0%) |
0(0.0%) |
2(3.2%) |
|
Female |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|
|
upper lobe consolidation |
Male |
0(0.0%) |
1(1.6%) |
1(1.6%) |
2(3.2%) |
|
Female |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|
|
middle &lower cavitations |
Male |
1(1.6%) |
0(0.0%) |
0(0.0%) |
1(1.6%) |
|
Female |
1(1.6%) |
0(0.0%) |
0(0.0%) |
1(1.6%) |
|
|
lower lobe cavitations |
Male |
0(0.0%) |
1(1.6%) |
0(0.0%) |
1(1.6%) |
|
Female |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|
|
diffuse consolidation |
Male |
2(3.2%) |
6(9.6%) |
0(0.0%) |
8(12.6%) |
|
Female |
1(1.6%) |
1(1.6%) |
0(0.0%) |
2(3.2%) |
|
|
diffuse cavitations |
Male |
1(1.6%) |
1(1.6%) |
0(0.0%) |
2(3.2%) |
|
Female |
1(1.6%) |
1(1.6%) |
0(0.0%) |
2(3.2%) |
|
|
upper &middle |
Male |
1(1.6%) |
0(0.0%) |
0(0.0%) |
1(1.6%) |
|
Female |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|
|
Total |
34(54.8%) |
22(35.4%) |
66(9.6%) |
62(100.0%) |
|
4.8 Regarding the relation between CT consolidation findings according to lung and lobe involved: Who were (42 out 110) 38.2%of study group:
Lower lobe involved with consolidation bilaterally in 11.9% of males & 38%of females, right side only in 0% of males 9.5% of females, left side 0% of males, and 2.3% of females. The upper lobe involved consolidation bilaterally in 2.3% of males & 0% of females, the right side only in 2.3% of males and 2.3% of females, left side in 0% of males and 0% of females.
Both middle and lower lobes involved consolidation bilaterally in 2.3% of males & 0% of females, the right side only in 0%of 2.3% of females, and the left side in 0% of males and 0% of females. Both upper and lower lobes involved consolidation bilaterally in 0% of males & 0% of females, the right side only in 0% of males and 0% of females, left side in 2.3% of males and 0% of females.
Diffuse lung involved with consolidation bilaterally in 7.14% of males & 7.14% of females, right side only in 0% of males and 0% of females, left side 0% of males and 0% of females. Peripheral lung involved consolidation bilaterally in 4.7% of males & 4.7% of females, right side only in 0% of males 0% of females, left side 1.6% of males, and 0% of females. [Table 8]
Table 8: Relation between the study groups between CT Consolidation finding according to lung & lobe involved (P.V=.132)
|
Finding |
Gender |
Bilateral |
Right |
Left |
Total |
|
Lower lobe |
Male |
5(11.9%) |
0(0.0%) |
0(0.0%) |
5(11.9%) |
|
Female |
16(38.0%) |
4(9.5%) |
1(2.3%) |
21(50.0%) |
|
|
Diffuse |
Male |
3(7.14%) |
0(0.0%) |
0(0.0%) |
3(7.14%) |
|
Female |
3(7.14%) |
0(0.0%) |
0(0.0%) |
3(7.14%) |
|
|
Peripheral |
Male |
2(4.7%) |
0(0.0%) |
0(0.0%) |
2(4.7%) |
|
Female |
2(4.7%) |
0(0.0%) |
0(0.0%) |
2(4.7%) |
|
|
Upper lobe |
Male |
1(2.3%) |
1(2.3%) |
0(0.0%) |
2(4.7%) |
|
Female |
0(0.0%) |
1(2.3%) |
0(0.0%) |
1(2.3%) |
|
|
Middle& lower |
Male |
1(2.3%) |
0(0.0%) |
0(0.0%) |
1(2.3%) |
|
Female |
0(0.0%) |
1(2.3%) |
0(0.0%) |
1(2.3%) |
|
|
Upper & lower |
Male |
0(0.0%) |
0(0.0%) |
1(2.3%) |
1(2.3%) |
|
Female |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|
|
Total |
33(78.5%) |
7(16.6%) |
22(4.7%) |
42(100.0%) |
|
4.9. Mean Age:
In CT, a total of one hundred ten and about sixty-three are male patients mean age of 59.0 and forty-seven are female patients mean age of 58.0.
In the x-ray total of fifty and about thirty-nine male patients mean age of 55.0 and 11 are female patients mean age of 56.0. [Table 9]
Table No 9: Mean Age:
|
|
Gender |
N |
Mean |
|
CT |
Male |
63 |
59.0 |
|
Female |
47 |
58.0 |
|
|
Total |
110 |
||
|
X-ray |
Male |
39 |
55.0 |
|
Female |
11 |
56.0 |
|
|
Total |
50 |
||
4.10. Compare mean between Finding CT and Finding X-ray:
In CT Total number is one hundred ten; the mean is about 41.900 and the standard deviation is about 3.1134.
The index-ray Total number is fifty; the mean is about 37.100 and the standard deviation is about .3307. [Table 10]
Table No 10: Compare between CT finding and X- ray finding:
|
Finding |
Total |
Mean |
Std. Deviation |
P.V |
|
CT |
110 |
41.900 |
3.1134 |
.054 |
|
X-ray |
50 |
37.100 |
.3307 |
Table No 11: Distribution of the study group according to the consolidation of CT (P.V= .034):
|
Finding CT |
Gender |
Total |
||
|
Male |
Female |
|||
|
Bilateral lower consolidation |
N |
5 |
0 |
5 |
|
% |
11.9% |
0.0% |
11.9% |
|
|
Bilateral diffuse |
N |
3 |
3 |
6 |
|
% |
7.1% |
7.1% |
14.2% |
|
|
Bilateral Pericardial |
N |
2 |
2 |
4 |
|
% |
4.7% |
4.7% |
9.4% |
|
|
Bilateral upper |
N |
1 |
0 |
1 |
|
% |
2.3% |
0.0% |
2.3% |
|
|
Bilateral lower |
N |
0 |
16 |
16 |
|
% |
0.0% |
38.0% |
38.0% |
|
|
Bilateral Middle and lower |
N |
1 |
0 |
1 |
|
% |
2.3% |
0.0% |
2.3% |
|
|
Right upper |
N |
1 |
1 |
2 |
|
% |
2.3% |
2.3% |
4.7% |
|
|
Right lower |
N |
0 |
4 |
4 |
|
% |
0.0% |
9.4% |
9.4% |
|
|
Left upper and lower |
N |
1 |
1 |
2 |
|
% |
2.3% |
2.3% |
4.7% |
|
|
Right Middle and lower zenal consolidation |
N |
0 |
1 |
1 |
|
% |
0.0% |
2.3% |
2.3% |
|
|
Total |
N |
14 |
28 |
42 |
|
% |
33.4% |
66.4% |
100.0% |
|
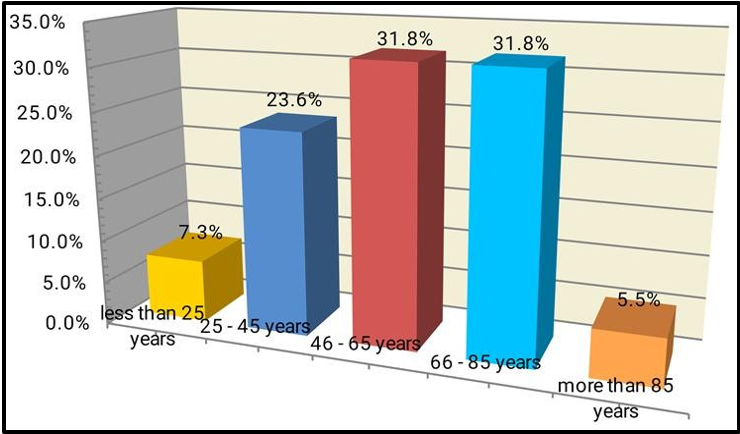
Figure 1: Distribution of the study group according to the Age Patient_ CT
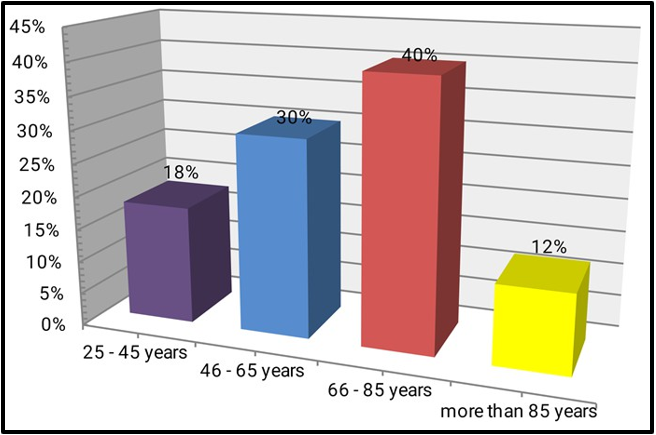
Figure 2: Distribution of the study group according to the Age Patient_ X-ray
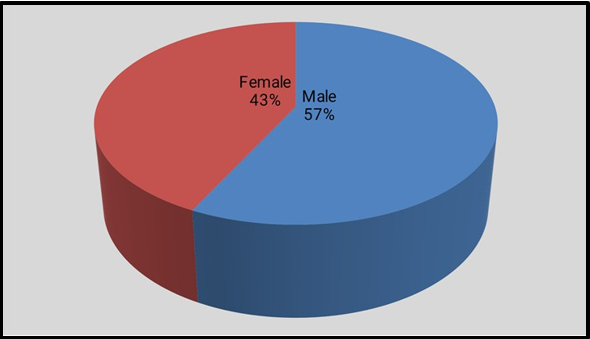
Figure 3: Distribution of the study group according to the Gender Patient _CT
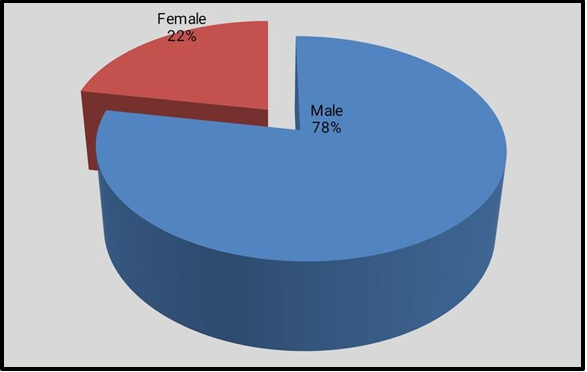
Figure 4: Distribution of the study group according to the Gender Patient _ X-ray
5. Discussion:
We assessed and described a variety of radiological patterns and their relationship to age and gender in this hospital-based descriptive retrospective study. We also calculated the incidence rate of COVID- 19 radiological patterns. One hundred sixty adult Sudanese patients in total, of whom fifty had chest x-rays (39 males and 11 females) and 110 had CT chests (63 males and 47 females) after testing positive for SARS-CoVID-2 infection on rRT-PCR and being admitted to different Sudanese isolation centers.
We found that 100% of them had positive radiological manifestations, in contrast to other studies done in multi-institutional centers in the United States that reported 88% of them having positive manifestations. [15]
Ages 46–65 and 66–85 are the most common age groups with positive chest CT findings (31.8% and 40%, respectively), while age groups 66–85 are the most common age group with positive chest X-ray findings.
Gender-wise, we found that positive chest X-ray results (78% in men and 22% in women) and positive chest CT results (57.3% in men and 42% in women) are more common in men than in women.
Regarding CT imaging results, ground glass opacity (91.8%) is the most frequent indicative feature, and consolidation (34.5%) was detected in more than 25.4% of COVID-19 patients. These results show a strong correlation with the multifocal pathogenesis, bilateral involvement, and progression of the disease. Which one most closely resembles the results of a study done in Hong Kong in April 2020? [16]
According to the CT scan results, involvement was detected in 2.7% of cases in the right upper lobe, 0.9% in the right middle lobe, 1.8% in the right lower lobe, and 2.7% in the left upper lobe. On the other hand, 92.9% of cases involved the right upper lobe, 92.9% in the right lower lobe, and 92.9% in the left upper lobe, according to an Italian study by Pascal Lomoro et al. [18]. Left upper lobar involvement was found in 76% of cases, right lower lobar involvement in 76% of cases, right upper lobar involvement in 67% of cases, and right middle lobar involvement in 48% of cases, according to a different study conducted by Ming-Yen Ngin Hong Kong. 81% had involvement in the left lower lobar region [16]
In addition, we discovered consolidation in 34.5% of patients as opposed to the 51.5% reported in the research by Thomas C. and Robert M. Kwee and the 62% found in the study by Ming-Yen Ngin. [15, 16] We discovered 11.8% of patients had pleural effusion, compared to 5.2% in the studies by Thomas C. and Robert M. Kwee, no patients had pleural effusion in Ming-Yen Ng and 7.1% in the Italian study by Pascal Lomoroet al. [15, 16, 18] We discovered nodules in 0.9% of the samples, compared to 19.8% for Thomas C. and Robert M. Kwee and 4.8% for Ming-Yen Ng's study. [15,4] We discovered that there was 30% mediastinal lymphadenopathy and 15.4% paratraceal lymphadenopathy, in contrast to the 5.1% lymphadenopathy reported in the studies by Thomas C. and Robert M. Kwee and the 14.3% found in the Italian study by Pascal Lomoroet al. [17, 18]
The majority of cases (66%) involving chest X-ray imaging involve both sides. This aligns with the findings of Pascal Lomoro et al's Italian study (78.1%). [18] In another study, Ho Yeun Frank Wong et al. in Hong Kong discovered that 50% of cases involved bilateral involvement. Neither in our study nor in the subsequent Hong Kong study was any pulmonary nodules found [37]. Pleural effusion was found in 3% of the cases, which is the same number as reported in the Hong Kong study (3%).
6. Conclusion:
This study highlights the significant role of both chest X-ray (CXR) and computed tomography (CT) in the diagnosis of COVID-19 among adult Sudanese patients, shedding light on how these patterns correlate with clinical severity and demographic factors. The finding revealed that ground- glass opacity and consolidations were the most common imaging features, consistent with global studies. However, unique variations in the frequency and distribution of these patterns were observed, potentially influenced by local factors such as genetic predispositions, environmental conditions, and healthcare accessibility. Radiological imaging, particularly CT scans, proved to be a critical tool in diagnosing and assessing the severity of COVID19 in Sudanese population. The study also highlighted a strong correlation between extensive radiological finding and severe clinical presentations, emphasizing the prognostic value of imaging in resources-limiting like Sudan. CXR findings bilateral lower zonal consolidation is a common feature in both male and female patients, reinforcing its utility in initial screening, especially in resources- limited settings. Given the observed variations, further studies could explore the prognostic significance of these patterns and their correlation with clinical outcomes.
7. Recommendations:
Based on the findings of this study, the following recommendations are proposed
1. Integration of radiological assessment into COVID-19 management protocols: radiological imaging, particularly CT scan, should be incorporated into the clinical guidelines for diagnosing and managing COVID-19 in Sudan. This will aid in early detection and severity assessment, especially in patients with atypical symptoms
2. Capacity building in radiology: enhance the training of radiologist and healthcare professionals in recognizing COVID-19-specific imaging patterns. Invest in advanced imaging technology and infrastructure, especially in underserved regions, to improve diagnostic capabilities.
3. Focus on resource-limited settings: develop simplified imaging protocols tailored to the Sudanese healthcare system, where resources may be constrained. For example, using portable chest x- rays as a preliminary diagnostic tool in remote areas.
4. Future research: conduct larger, multicenter studies to validate the findings and explore regional variations in radiological patterns. Also investigate the potential influence of genetic, environmental, and lifestyle factors on radiological manifestations of COVID-19 in Sudanese patients.
5. Public health initiatives: raise awareness among healthcare providers about the significance of imaging in diagnosis and monitoring COVID-19. Also strengthen collaboration between radiology departments and public health authorities to facilitate rapid diagnosis and response.
6. Utilization of Telemedicine and Teleradiology: establish teleradiology systems to ensure that rural and underserved areas have access to expert radiological interpretations.
By implementing these recommendations, Sudan's healthcare system can better leverage radiological insights to enhance the diagnosis, treatment, and overall management of COVID-19.
8. Note On The Authors' Contribution
The idea and design of the study were contributed to by all authors. They took care of the material preparation and data collection. The analysis and final draft were finished by Mohammad Mahgoub Altayib adabalfila, Ahmed Awadelkareem Omer Mahmoudd, Ahmed Hassan Abushama Altom. The manuscript was written by Motwakil Imam Awadelkareim in its initial draft. Every author offered feedback on earlier drafts of the work. All authors have read and approved the final manuscript.
9. Acknowledgment: Deep appreciation to all of the students at the fascinating Shendi University
10. List of abbreviations:
|
Abbreviation |
Term |
|
RNA |
Ribonucleic Acid |
|
SARS |
severe acute respiratory syndrome |
|
MERS |
Middle East respiratory syndrome |
|
CT |
Computerized Tomography scan |
|
CXR |
Chest X Ray |
|
RT-PCR |
real-time reverse transcription polymerase Chain reaction |
|
GGO |
Ground Glass opacity |
|
SARS-CoV |
Severe Acute Respiratory Syndrome Covid |
|
USA |
United States of America |
|
WHO |
World Health Organization |
|
PUI |
patient under investigation |
|
CFR |
case fatality rate |
|
IFR |
infection fatality rate |
|
RBD |
Receptor Binding Domain |
|
EOC |
Emergency Operations Center |
|
WBC |
White blood cell |
|
CRP |
C- reactive protein |
|
LDH |
Lactate dehydrogenase |
|
AST |
Aspartate transaminase |
|
ALT |
Alanine transaminase |
|
SPSS |
Statistical package for social science |
11. Conflict Interest
The authors declared no conflict of interest.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors.
12. Appendixes: Examples of imagines of some patients enrolled in this study with different types of radiological patterns
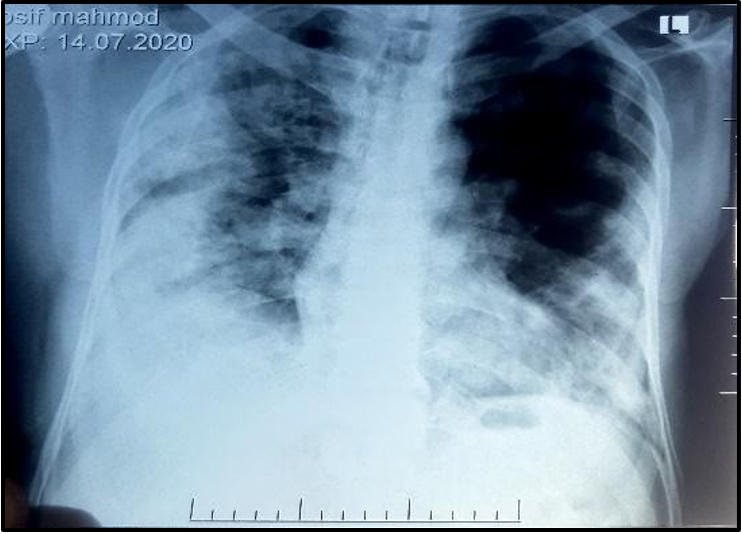
Figure 1: CXR shows bilateral middle
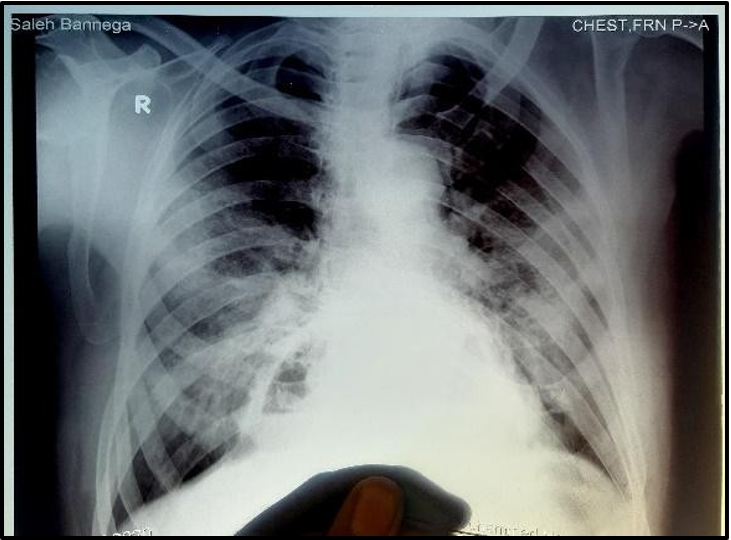
Figure 2: CXR shows bilateral peripheral ground glass opacities and Lower zone opacity with lung retiicular shadowing air bronchogram denoting consolidation
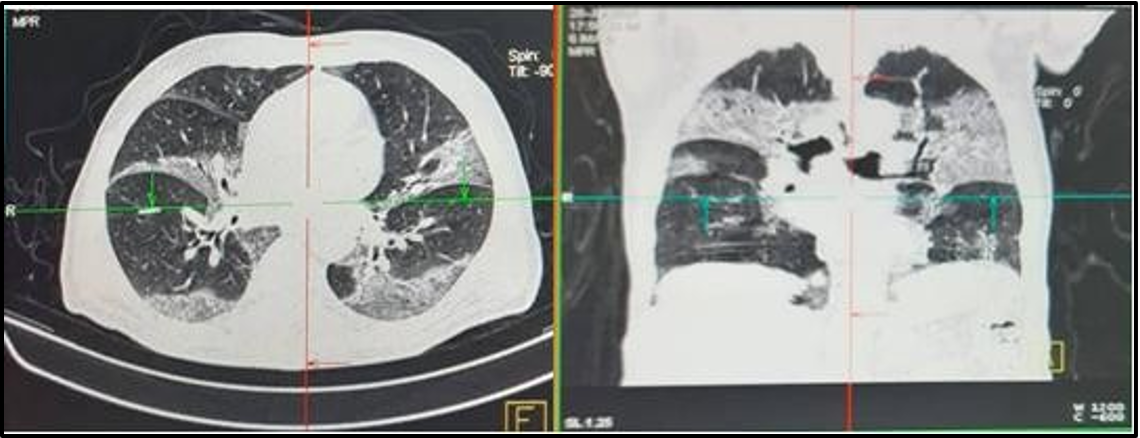
Figure 3: HR- CT-Chest (Axial and segetal views) revealed: bilateral sub-segmental peri-lymphovascular dense posterior ground glass opacities (Consistent with COVID pneumonia)
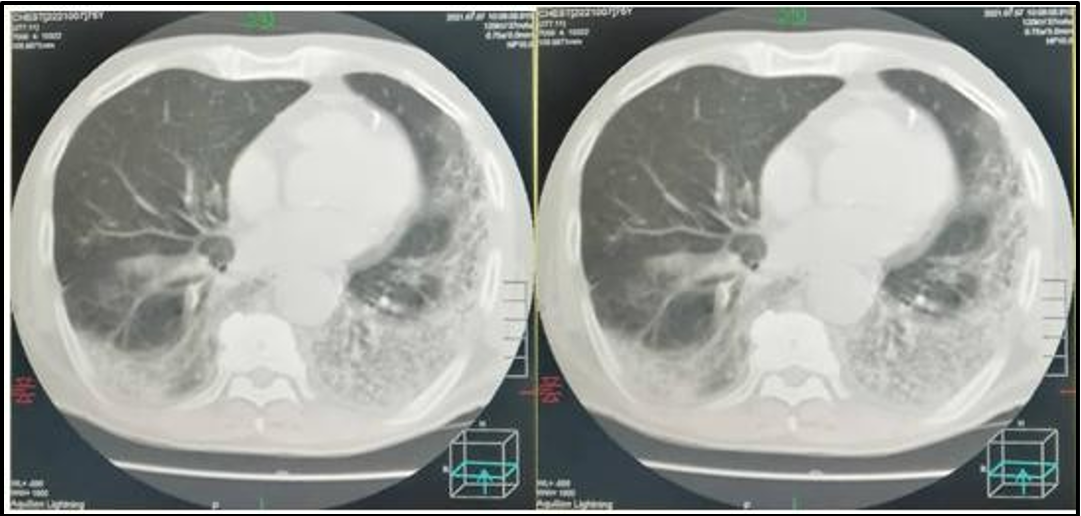
Figure 4: HR- CT-Chest revealed: Dense peripherally located mainly posterior ground glass opacities. More noted at the left lung (Consistent with COVID pneumonia)
13. References
- Singh T (2020) A review of coronavirus disease-2019 (COVID- 19), The Indian journal of pediatrics 87(4): 281-286.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC (2020) Path physiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. Jama. 324(8): 782-93.
- Poongothai S, Anjana RM, Aarthy R, Kasthuri S, Begum MA, et al. (2020) Strategies adopted in the conduct of clinical trials amidst coronavirus disease-2019 (COVID-19). Journal of Dialectology. 11(2): 81-85.
- Ng M, Lee E, Yang J, Yang F, Li X, et al. (2020) Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review, Radiology: Cardiothoracic Imaging. 2(1): e200034.
- Atherstone C, Siegel M, Schmitt-Matzen E, Sjoblom S, Jackson J, et al. (2021) SARS-CoV-2 transmission associated with high school wrestling tournaments—Florida, December 2020–January 2021. Morbidity and Mortality Weekly Report. 70(4): 141.
- Centers for Disease Control and Prevention (2020) Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). CDC.
- Bohn MK, Hall A, Sepiashvili L, Jung B, Steele S, et al. (2020) Path physiology of COVID-19: mechanisms underlying disease severity and progression. Physiology. 35(5): 288-301.
- Bohn MK, Hall A, Sepiashvili L, Jung B, Steele S, et al. (2020) Path physiology of COVID-19: mechanisms underlying disease severity and progression. Physiology. 35(5): 288-301.
- Abougazia A, Alnuaimi A, Mahran A, Ali T, Khedr A, et al. (2021) Chest X-Ray Findings in COVID-19 Patients Presenting to Primary Care during the Peak of the First Wave of the Pandemic in Qatar: Their Association with Clinical and Laboratory Findings. Pulmonary Medicine. 2021: 4496488.
- Gandhi D, Jain N, Khanna K, Li S, Patel L, et al. (2020) Current role of imaging in COVID-19 infection with recent recommendations of point of care ultrasound in the contagion: a narrative review. Annals of Translational Medicine. 8(17): 1094- 1094.
- https://emedicine.medscape.com/article/2500114-clinical#b1
- https://www.ecdc.europa.eu/en/covid-19/latest-evidence/clinical
- https://emedicine.medscape.com/article/2500114-workup
- Kermali M, Khalsa RK, Pillai K, Ismail Z, Harky A (2020) The role of biomarkers in diagnosis of COVID-19: A systematic review. Life Sci. 254: 117788.
- Azevedo RB, Botelho BG, Hollanda JVG, Ferreira LVL, de Andrade LZJ, et al. (2021) Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens. 35(1): 4-11.
- Ng MY, Lee EYP, Yang J, Yang F, Li X, et al. (2020) Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. The British journal of radiology. 2(1): e200034.
- Palabiyik F, Kokurcan SO, Hatipoglu N, Cebeci SO, Inci E (2020) Imaging of covid-19 pneumonia in children. The British Journal of Radiology. 93(1113): 20200647.
- Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, et al. (2020) COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review,European Journal of Radiology Open. 7: 100231.