Adebayo BE, Adigun MB, Folayan OS*, Omotosho O, Akindolire AE, Omokhodion SI
Department of Paediatrics, University College Hospital, Ibadan, Oyo State, Nigeria.
*Corresponding Author: Folayan OS, Department of Paediatrics, University College Hospital, Ibadan, Oyo State, Nigeria.
Abstract
The era of rapidly advancing technology has heralded an increase in the use of central lines for diagnostic and therapeutic procedures in caring for critically ill children. There has also been an attendant increase in the incidence of catheter-related complications. Femoral cannulation for rapid fluid resuscitation in children with high output fluid losses is lifesaving, but complications like intravascular fracture of the femoral catheter may occur. An urgent surgical or percutaneous retrieval will prevent migration or embolization that could be life-threatening.
We report the case of a 4-year-old girl with dextrocardia and tetralogy of Fallot who had hypovolemic shock complicating acute diarrheal disease. She required a femoral venous catheter insertion for rapid fluid replacement. The catheter fractured into her left femoral vein following repeated knee-chest posture but was retrieved by surgical intervention before it could migrate.
The use of central lines and their attendant complications have increased in the care of critically ill children. Intravascular catheter fracture and embolization are life-threatening complications that require urgent surgical or percutaneous removal.
Keywords: Femoral cannulation, Central venous catheter complication, Fractured catheter.
Introduction
Intravascular fracture of an indwelling catheter is a rare, life-threatening complication of femoral vein cannulation. The femoral vein is a common site of catheterization in children and a common site of catheter fracture due to the frequent limb movement and compression of the catheter against the pelvic bone. The incidence of catheter fracture varies from 0.5 % to 3 % based on the type and duration of catheterization.[1] Risk factors include defective catheter material, improper handling, or kinking of the catheter during insertion or use. Following such fractures, an urgent surgical retrieval is needed to prevent embolization.
Case Profile
A 4-year-old girl presented with a 3-year history of cyanosis and recurrent fast breathing that worsened about once in a fortnight but resolved spontaneously after squatting. She frequently sleeps with her hips flexed. She had a 1/7 history of low-grade intermittent fever and eight bouts of large-volume watery stools before presenting to the emergency room. Examination findings showed she was severely dehydrated, plethoric, centrally cyanosed, and febrile (38.7°C) with a grade IV digital clubbing. Her respiratory rate was 36cpm, with vesicular breath sounds. Oxygen saturation ranged between 67- 87 % on room air and 90 % on intranasal oxygen. Her peripheral pulses were small in volume, with 150 beats per minute heart rate and a blood pressure reading of 98/54mmHg. Her apex was at the 4th suitable intercostal space, mid-clavicular line. The first heart sound was average, but the second was soft and single.
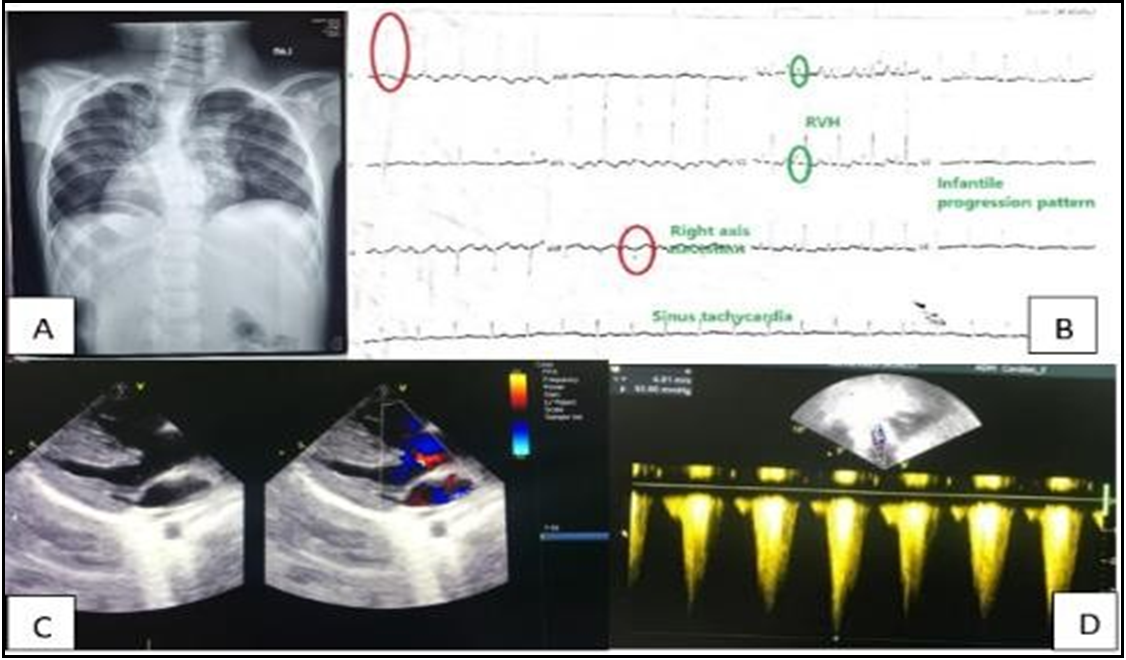
Figure 1: A Radiograph showing dextrocardia. B.ECG features of Fallot's tetralogy. C.Large VSD and right ventricular hypertrophy on echocardiography. D. High velocity in the right ventricular outflow tract suggesting stenosis.
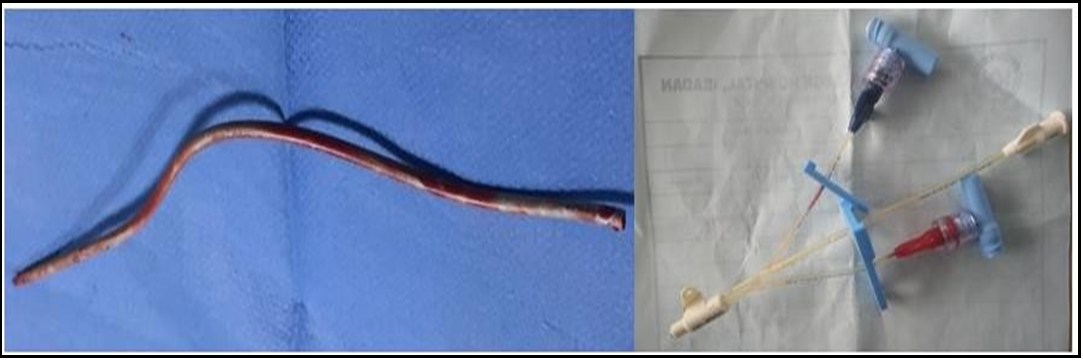
Following a diagnosis of dextrocardia with Fallot’s tetralogy and acute diarrheal disease in hypovolemic shock, a femoral venous catheter was inserted for rapid fluid resuscitation. As a result of her default posture of repeated hip joint flexion, the catheter fractured at its joint with the hub eight hours after insertion. The venous catheter was palpated in the right femoral vein, and its extent and degree of thrombosis were determined with an ultrasound scan. The affected limb was immobilized, and a firm adhesive tape was applied to limit migration while she was worked up for urgent exploration surgery. The fractured segment retrieved following a surgical exploration of the right femoral vein measured 15cm long. She had good distal lower limb pulses following surgery and awaits open heart surgery to correct congenital heart disease.
Figure 2: The retrieved segment of the femoral catheter and the proximal hub.
Discussion
Intravascular fractures of indwelling catheters are rare but can result in serious complications, such as embolization, infection, and vessel occlusion.[2] In the pediatric population, the three veins commonly used for cannulation are the internal jugular, subclavian, and femoral veins.3 The femoral vein is a common site of catheter placement in children because of its easy access, predictable anatomy, ease of arresting hemorrhage in the advent of an arterial puncture, and because it is further away from the airway or the heart.[4] It is vital in rapid fluid replacement when high output fluid losses occur in children.[3]
The more common complications associated with femoral vein cannulation include puncture site infection, femoral artery or femoral vein thrombosis, phlebitis, arteriovenous fistula, injury to the femoral nerve, and retroperitoneal hemorrhage.[5] Catheter fracture is a rare complication with an incidence of 0.5% to 3% reported for fractures that occurred in the subclavian and internal jugular veins.[6] Reports on femoral catheter fractures are rare, probably because the route is not commonly used in most developed countries or because such incidents are underreported.[7], however, it is a standard dialysis route in many resource-limited settings. [6] Fractures can occur either spontaneously or at the time of port removal, the most typical point of fracture being the junction of the catheter with its hub and the catheter tip.[8]
Factors that have caused an increase in catheter fracture occurrence include defective catheter material that escapes quality control checks, forceful insertion, or removal, bent or kinked catheter, and catheter damage at the time of insertion.[8] A fractured catheter within a vessel increases blood stasis and causes vessel damage, thereby increasing the risk of thrombosis. The fragment can also embolise into the cardiac chambers and cause life-threatening arrhythmias.[4]
Our patient's catheter fractured at the hub and was attributed to the repeated flexion of her hip joint, a compensatory posture that relieves the hypercyanotic spell of Fallot's tetralogy. [9] The hip flexion could have also kinked the catheter, putting it under much shear stress and increasing the risk for a fracture. The soaked plaster dressing and the bedding drew attention and prompt intervention that averted life-threatening complications.
Imaging studies, such as ultrasound and X-ray, can help locate the fractured segment of the catheter. We identified the fragmented portion of the catheter using an ultrasound scan. Open surgical exploration or interventional radiology can retrieve the fragmented piece using percutaneous endovascular retrieval. [2,10] The method employed depends on the personnel's skill and the facility's availability for minimally invasive recovery.
In this case, the fragment was removed by surgical exploration as this was the readily available option.
Conclusion
Central lines are life-saving medical devices whose use and associated complications have increased in pediatric emergency and critical care. Though rare, femoral catheter fragmentation and embolization are life-threatening and require urgent retrieval. Healthcare providers should be aware of the risk factors for catheter fracture and take appropriate precautions to prevent its occurrence.
References
- Maisey NR, Sacks N, Johnston SR (2003) Catheter fracture: A rare complication of totally implantable venous devices. Breast. 12(4): 287–9.
- Andrews RE, Tulloh RM, Rigby ML (2002) Percutaneous retrieval of central venous catheter fragments. Arch Dis Child. 87(2): 149–50.
- Haas NA (2004) Clinical review: Vascular access for fluid infusion in children. Crit Care. 8(6): 478–84.
- Gray RM (2012) The where, what and how of paediatric central venous access. South African J Anaesth Analg. 18(5): 249–53.
- Al-Jawder SE, Hameed AA (2004) Complications of femoral venous catheterization in critically ill patients. Saudi Med J. 25(2): 240–1.
- Awobusuyi JO, Falase B, Johnson A, Ogbera AO, Sanusi M (2009) Fractured Femoral Catheter Tip in Repeated Femoral Vein Cannulation for Haemodialysis Vascular Access. Trop J Nephrol. 4(2): 121–4.
- Helal I, Elyounsi F, Hamida FB, Aderrahim E, Hedri H, et al. (2010) Fracture and embolization of a temporary hemodialysis femoral catheter. J Vasc Access. 11(1): 74–5.
- Kale SB, Ramalingam S (2017) Spontaneous arterial catheter fracture and embolisation: Unpredicted complication. Indian J Anaesth. 61(6): 505-507.
- Murakami, T., Shiraishi, M., Fukuoka, S., Higashi, K., Nakajima, H., Aotsuka. H. (2016) The hemodynamic change by squatting is induced by diminished vascular distensibility and enhanced pressure wave reflection. J Hypertens. 34(September): 20–5.
- Bessoud B, de Baere T, Kuoch V, Desruennes E, Cosset MF, et al. (2003) Experience at a single institution with endovascular treatment of mechanical complications caused by implanted central venous access devices in pediatric and adult patients. Am J Roentgenol. 180(2): 527–32.