Luana Silva1*, Sónia Lemos2, João Cabral1 , Cristina Alves1
1Department of Pediatric Orthopaedics - Hospital Pediátrico - CHUC, EPE, Coimbra, Portugal
2Pediatric Allergology Department - Hospital Pediátrico - CHUC, EPE, Coimbra, Portugal
*Corresponding Author: Luana Silva, Department of Pediatric Orthopaedics - Hospital Pediátrico - CHUC, EPE, Coimbra, Portugal
Abstract
Local complications after vaccine inoculation have a wide range of severity. Intramuscular abscess formation is a known but rare occurrence. It can be sterile or of infectious etiology. We report a previously healthy 5-week-old boy that presented at the emergency department with a swelling in the right thigh, at the injection site of hepatitis B vaccine, pain, and pseudo paralysis of the right lower limb. An intramuscular abscess was suspected on clinical examination and ultrasound and confirmed by magnetic resonance. He underwent surgical drainage and antibiotic treatment. A methicillin-sensitive Staphylococcus aureus was isolated from the intraoperative pus culture. At 8 months, the patient was asymptomatic, without sequelae.
Severe inflammatory signs at common vaccine inoculation sites should evoke deep soft tissue complications. Imaging plays an important role in the differential diagnosis. Clinicians should be aware of such complications. Infection prevention strategies should be reinforced regarding vaccine administration techniques.
Keywords: Abscess, vaccination, surgical drainage, Staphylococcus aureus
Introduction
Immunization is important for disease prevention and is used in different healthcare systems around the world. Since 2000, the hepatitis B vaccine was implemented in our country’s National Vaccination Program, with a recommendation for the first dose to be administered shortly after birth, in the right thigh [1].
Adverse reactions to vaccine administrations are well described, with post-injection abscess being one of them, albeit less frequent [2]. Mostly they are subcutaneous, but deep intramuscular abscess has been reported, especially in the first year of life. They may be sterile, secondary to an exacerbated immune response, or infectious, related to bacterial contamination of the vaccine or errors in the administration technique [3]. The latter are mostly caused by skin commensals, such as methicillin-sensitive Staphylococcus aureus (MSSA) or methicillin-resistant Staphylococcus aureus (MRSA), and recently described vancomycin-resistant Staphylococcus aureus [4]. We report the clinical case of a 5-week-old boy presenting with an intramuscular abscess that required surgical drainage, caused by MSSA, following a hepatitis B vaccine.
Case Presentation
A male full-term newborn, with 3350 g of birth weight, had an intramuscular administration of hepatitis B (HepB) vaccine in the right thigh, 48 hours after birth. At 5 weeks of age, in a routine appointment, it was observed swelling in the right thigh (Figure 1) and reduced active right lower limb movements. There was a pain when mobilizing the limb and fever was absent. The family had noticed the reduced movements of the right limb during the previous week. The infant was referred to a pediatric emergency department (ED) in another institution. He had blood tests, which showed leukocytosis (18.40 x 10⁹/ uLuL). C-Reactive Protein (CRP) and erythrocyte sedimentation rate (ESR) couldn’t be obtained. In the ultrasound, it was found around an area in the muscular plane of the rectus femoris muscle, that could be an intramuscular hematoma.
He was discharged under amoxicillin and clavulanic acid (60 mg/Kg/day).
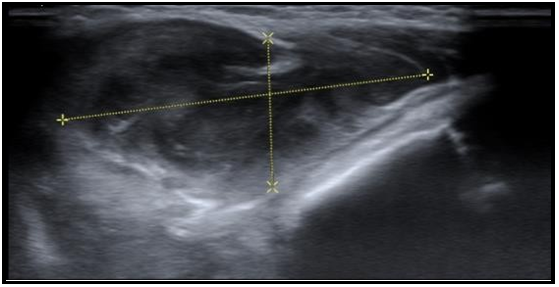
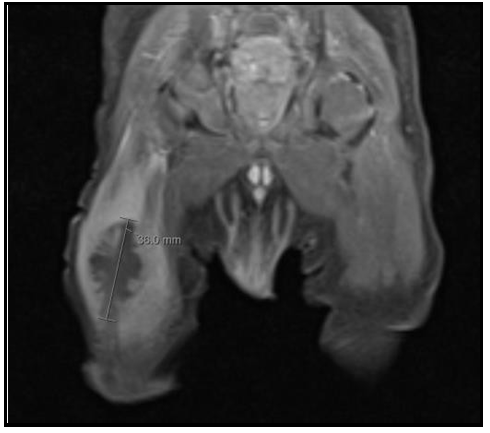
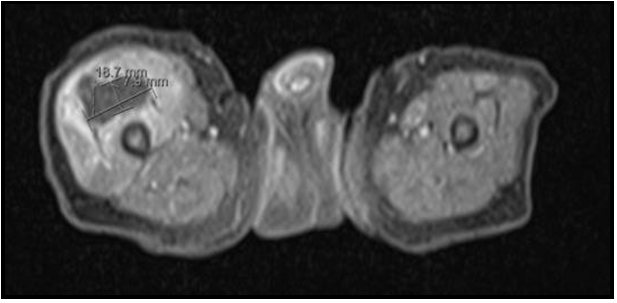
As the child was not improving, two days later he was brought to our ED. On physical examination, he was looking well and had normal vital signs, but cried upon touching the right lower limb; an anterior tumefaction in the right thigh was observed, measuring roughly 3 cm in diameter. There was no erythema or heat. Laboratory investigations revealed discrete leukocytosis (16.70 x 10⁹/uL) with 43 % neutrophils, 37 % lymphocytes, anemia (hemoglobin concentration of 10.7 g/dl) and normal platelet count; CRP was 1.25 mg/dL and a ESR 95/mm1ªh. Ultrasound showed a fusiform, heterogeneous, hypoechogenic image (Figure 2) in the quadriceps muscle. Magnetic resonance imaging (MRI) identified a lobulated nodular image with 36 x 19 x 8 mm (Figure 3 and 4), in the central portion of the rectus femoris, hyperintense in T2-weighted and hypointense in T1 weighted images, suggesting an intramuscular abscess.
Figure 1: Right thigh swelling 2 days before emergency department presentation.
Figure 2: Soft tissue ultrasound: fusiform, heterogeneous, hypoechogenic image in the quadriceps muscle.
Figure 3: Magnetic resonance imaging, coronal cut: T1 image shows a intramuscular fluid collection in the right quadriceps muscle.
Figure 4: Magnetic resonance imaging, transversal cut: T1 image shows an intramuscular fluid collection in the right quadriceps muscle.
Based on clinical symptoms and the imaging findings, the patient was diagnosed with a rectus femoris intramuscular abscess following a vaccine inoculation. The infant was taken to the operating room for incision and drainage of the abscess. He was started on intravenous flucloxacillin 200 mg/Kg/day during 11 days, the first-line therapy for the community-acquired invasive staphylococcal disease, with full resolution of the symptoms. The pus culture was positive for MSSA.
After full recovery, a primary immunodeficiency (PID) screening was made, with normal neutrophil oxidative burst test, normal lymphocyte populations, immunoglobulin A and G within the normal range, and high immunoglobulin M (0.77 g/L (N 0.06 - 0.21)) that gradually decreased reaching normal values at 2.5 months of age. At 8 months of age, he was asymptomatic, had normal growth and neurodevelopment.
Discussion
This report describes a 5 weak infant with an infectious intramuscular abscess following a vaccine inoculation, a rare complication of vaccine administration. Most post-vaccination local reactions include injection-site pain, erythema, edema, and less frequent injection-site abscess (ISA). This entity may be due to local trauma of the procedure, reaction to the irritating content of the vaccine, such as adjuvants, or the vaccine injection technique [5,6].
In a ten-year review of adverse events following immunizations in the USA, 426 ISA were reported in a total of 128,717 events (0,033 %) [1,2]. They can be sterile, probably related to a delayed hypersensitivity reaction to an adjuvant or excipient agent used in the vaccines. The reaction induces the formation of a nodule that can evolve into an abscess. Abscesses following aluminum-containing vaccines are well known [7–9]. Lauren et al presented a case of persistent subcutaneous nodules and sterile abscesses in a 7 months infant in the setting of delayed hypersensitivity to aluminum, confirmed by patch testing and recurrence on re-exposure [9].
Infectious ISA is related to contamination or inadequate disinfection of the vaccine vial rubber stopper in a multi-dose drug vial, lack of infection control such as not handwashing between vaccinating children [3]. In 1993 Simons et al. reported 9 cases of pyogenic abscesses after diphtheria, tetanus toxoids, and pertussis vaccination. Staphylococcus aureus was isolated in 4 pus cultures and Group a Streptococcus (GAS) in 8. After epidemiologic investigation, it was revealed that 3 children had been diagnosed with streptococcal pharyngitis within the hour of the first child’s vaccination. Laboratory studies proved that GAS can survive 4 days in the external surface of the rubber stopper of the vaccine vial, contaminating the needles inserted through the stopper [10].
In our case, an MSSA, the most common agent, [3,11,12], was identified. A cluster of community-acquired MRSA transmitted by a colonized healthcare professional has been described [13]. Lucca et al and Kuyubasi et al reported abscesses following the HepB vaccine, the first one sterile, the second one caused by MSSA infection [8,12]. Imaging plays an important role in the differential diagnosis of soft skin tissues masses. The ultrasound, the first line exam, is fast, cost-effective, and doesn’t expose the patient to ionizing radiation. However distinguishing abscesses from hematomas can be difficult, as both have a hypoechogenic fluid collection [14]. MRI was important to characterize the nodule and therefore to help establish the best management.
Surgical treatment associated with antibiotics insured the best outcome. In 2010 Tan et al, reported a series of cases of intra-femoral post-vaccination abscesses that required surgical drainage in a tertiary child´s hospital in Singapore. All seven cases ranged from 4 to 7 months, had a positive culture for MSSA, and resolved after drainage and a course of cloxacillin [3].
At this age, susceptibility to infections is common due to immunological immaturity [15], but although in our patient the PID screening was negative, it is important to remember that a severe atypical infectious disease, particularly at an early age, can be a sign of immunodeficiency [16]. HyperIgE syndrome is a combined immunodeficiency disorder characterized by Staphylococcal infections including abscesses with a lack of inflammatory signs. Abscesses can also be seen in phagocyte disorders such as chronic granulomatous disease [17,18]. The transient rise in IgM in our patients can be interpreted as an immunological response to infection. Despite being described, these less frequent complications are still unknown to many clinicians, therefore the importance of reporting such cases. The vaccine was administered in the maternity and it was an isolated case. We believe, as shown in previous cases, that this infection must be related to a lack of aseptic technique during the administration of the vaccine. Efforts to perform a correct and aseptic vaccination technique should be reinforced in the maternities and primary care centers.
What This Report Shows?
Swelling and pain in at a previous vaccination site should evoke soft tissue abscess
Post-vaccination abscesses can be sterile or secondary to an infection, and Staphylococcus aureus is the most commonly implicated agent
Ultrasound is the first-line imaging exam, but MRI may be important for differential diagnosis
Antibiotic therapy and surgical drainage are important for treating these infectious abscesses
A correct and aseptic vaccination technique should be reinforced
Authors contribution:
Writing original draft – Luana Silva
Review and editing – Sónia Lemos, João Cabral
Review, editing, and approval of manuscript – Cristina Alves
References
- Direção-Geral da Saúde (2020) Programa Nacional de Vacinação 2020. Lisboa.
- Zhou W, Pool V, Iskander JK, English-Bullard R, Ball R, et al. (2003) Surveillance for safety after immunization: Vaccine Adverse Event Reporting (VAERS) — United States , 1991 – 2001. MMWR Surveill Summ. 52(1):1-24.
- Tan NWH, Pan WJ, Yunos HHBM, Tan WC, Lim KBL (2010) Post-vaccination abscesses requiring surgical drainage in a tertiary children’s hospital in Singapore. J Pediatr Infect Dis. 5(2): 139-147.
- Sambandam SN, Rohinikumar GJ, Gul A, Mounasamy V (2016) Intramuscular Injection Abscess Due to VRSA: A New Health Care Challenge. Arch Bone Jt Surg. 4(3): 277–81.
- Polat AV, Bekci T, Dabak N, Ulu EMK, Selcuk MB (2015) Vaccine-induced myositis with intramuscular sterile abscess formation: MRI and ultrasound findings. Skeletal Radiol. 44(12): 1849–52.
- Tomás-Pérez M, Gómez-Traseira C, González-Muñoz M, Quirce S (2020) Adverse reaction with hexavalent vaccine: An unusual case. Allergol Immunopathol (Madr). 48(6): 801-803.
- Bernier RH, Frank JA, Nolan TF (1981) Abscesses Complicating DTP Vaccination. Am J Dis Child. 135(9): 826–8.
- Lucca JM, Sebastian J, Ravi MDR, Parthasarathi G (2019) Sterile Abscess Following Hepatitis B Vaccination in a New Born- A Case Report. J Clin Diagnostic Res. 13(9).
- Lauren CT, Belsito DV, Morel KD, LaRussa P (2016) Case report of subcutaneous nodules and sterile abscesses due to delayed type hypersensitivity to aluminum-containing vaccines. Pediatrics. 138(4): e20141690.
- Simons PA, Chen RT, Elliott JA, Schwartz B (1993) Outbreak of pyogenic abscesses after diphtheria and tetatus toxoids and pertussis vaccination. Pediatr Infect Dis J. 12(5): 368–71.
- Addison M, Lazzaro T, Crawford N (2019) Injection site abscess (ISA) following an infant vaccine. Vaccine. 37(9): 1151-1152.
- Kuyubasi SN, Cagatay E, Çıraklı A, Çıraklı S, Kılıç M (2013) Unusual cause of thigh abscess in infant following hepatitis B vaccine administration. J Exp Clin Med. (30): 181-182.
- Tang CT, Nguyen DT, Ngo TH, Nguyen TM, Le VT, et al. (2007) An Outbreak of Severe Infections with Community- Acquired MRSA Carrying the Panton-Valentine Leukocidin Following Vaccination. PLOSone. 2(9): 5-10.
- O’Rourke K, Kibbee N, Stubbs A (2015) Ultrasound for the Evaluation of Skin and Soft Tissue Infections. Mo Med. 112(3): 202–5.
- Diniz LMO, Figueiredo B de CG e (2014 ) The newborn’s immune system. Rev Médica Minas Gerais. 24(2): 227-233.
- Connell AEO (2019) Primary Immunodeficiency in the NICU. Neoreviews. 20(2): e67-e78.
- McCusker C, Upton J, Warrington R (2018) Primary immunodeficiency. Allergy, Asthma Clin Immunol. 14(s2): 1–12.
- Minegishi Y, Saito M (2012) Cutaneous Manifestations of Hyper IgE Syndrome. Allergol Int. 61(2): 191–196.